* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Immunology 3 – Innate Immunity
Survey
Document related concepts
Hygiene hypothesis wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Molecular mimicry wikipedia , lookup
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Transcript
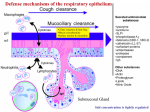
MCD – Immunology 3 – Innate Immunity Anil Chopra 1. Briefly describe the functions of the important phagocytic cells: neutrophils, monocytes/macrophages. Innate immunity is that which is “inbuilt”, present from birth. It is not antigen-specific, but is able to recognise pathogen-specific molecular patterns. It is the same at every time the body is exposed to an antigen (has no memory). Neutrophils – 50-70% leukocytes, these are the first cells to arrive at the site of damage/infection. They move into tissues, phagocytose and kill pathogens. They are more effective after opsonisation. This is where the antigen is given a coat of various proteins that the neutrophils recognise and can bind to. Both antibodies and complement act as opsonins. They have oxygen independent ways of killing: • Enzymes • Lysozyme • Hydrolytic enzymes • Antimicrobial peptides (defensins) There are also oxygen dependent ways of killing: Respiratory burst: toxic metabolites Superoxide anion Hydrogen peroxide Singlet oxygen Hydroxyl radical Reactive nitrogen intermediates Nitric oxide Phagocyte deficiency is associated with infections due to extracellular bacteria and fungi. Macrophages - when blood monocytes enter tissues they become tissue macrophages. They express receptors for many different kinds of antigen. They are concerned with pattern recognition which they use to phagocytose antigens and the pathogens causing them. They release soluble mediators. 2. Define cytokines and describe their general properties. Cytokines: • Small secreted proteins • Cell-to-cell communication • “messengers” of the immune system • Generally act locally • Biological effects at very low concentrations • Short-lived There are 5 types of cytokine: • INTERLEUKINS (IL-x): Between leukocytes • INTERFERONS (IFN): Anti-viral effects • CHEMOKINES: Chemotaxis, movement • GROWTH FACTORS • CYTOTOXIC: Tumour necrosis factor (TNF) Important cytokines include • IL-1 ALARM CYTOKINE, FEVER • TNF- ALARM CYTOKINE • IL-6 ACUTE PHASE PROTEINS, LIVER • IL-8 CHEMOTACTIC FOR NEUTROPHILS • IL-12 DIRECTS ADAPTIVE IMMUNITY, ACTIVATES NK CELLS In the condition of bacterial septic shock, the bacterial endotoxins release large amounts of TNF- AND IL-1 which causes increased vascular permeability, severe drop in blood pressure and death in about 10% of cases. Dendritic Cells: form networks of cells near sites of infection. They secrete cytokines and also bring pathogens to lymph nodes where they bring them into contact with cells of the adaptive immune system. 3. Define complement, list its major functions, and draw a simple diagram of the complement pathways. Complement Complement is a set of enzymes that complements the activity of specific antibodies. They form a cascade which results in rapid, amplified response from the antibodies. Complement Cascade: This cascade is controlled by: • Liability of components • Dilution of components in biological fluids • Specific regulatory proteins Functions of Complement: 4. Describe a typical inflammatory response to a localised infection involving recruitment of neutrophils, and phagocytosis and killing of bacteria. Mast Cells • Secrete histamine and other inflammatory mediators, including cytokines. • Mucosal mast cells (lung) • Connective tissue mast cells (skin and peritoneal cavity, near blood vessels) • Can recognise, phagocytose and kill bacteria. • Can be activated by complement products. (anaphylatoxins) • Leads to vasodilation and increased vascular permeability. 5. Briefly outline the events involved in a systemic acute phase response. This is a reaction that may accompany inflammation and may consist of fevers, increased leukocytosis, and production of “acute phase” proteins from the liver. These include: • C-reactive protein (CRP) – C polysaccharide of pneumococcus – Activates complement – Level may increase 1000 fold • Mannan binding lectin (MBL) – Opsonin for monocytes, activates complement • Serum amyloid a (similar to CRP) • Complement • Fibrinogen (clotting) 6. Outline the phenotype and functions of natural killer (NK) cells. Natural Killer Cells These are large granulated lymphocytes that are cytotoxic i.e. they lyse target cells. They account for around 5-10% peripheral blood lymphocytes. They contain no antigen-specific receptors but are important in defence against tumour cells and viral infections. (esp. herpes) They are recruited to sites of infection by chemokines; they secrete IF- and have receptors which bind to antibody-coated cells (ADCC).