* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CARDIAC EXAM TWO Patient Assessment Assessment should
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Transcript
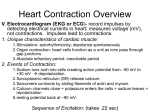
CARDIAC EXAM TWO Patient Assessment I. II. III. IV. Assessment should include a. Physical Examination, Palpitation, percussion, auscultation, medications, nutrition, elimination, activity and exercise, sleep and rest, VS, self perception, roles and relationships, sexuality and reproduction, coping and stress tolerance, prevention strategies, family history Heart Inspection a. Aortic Area i. 2nd intercostal space to the right of the sternum b. Pulmonic Area i. 2nd intercostal space to the left of the sternum c. Erb’s Point i. 3rd intercostal space to the left of the sternum d. Tricuspid Area i. 4th and 5th intercostal spaces to the left of the sternum e. Mitral (Apical) Area i. Left 5th intercostal space at the midclavicular line ii. Apical pulse to be taken for one full minute f. Epigastric Area i. Below the xiphoid process Ask regarding health promotion and preventative practices type questions Laboratory Tests a. CPK- Creatinine Phosphokinase i. Usually caused by heart attack ii. Onset: 4-6 hours iii. Peak: 24 hours iv. Return to Normal: 2-3 days v. N or S Values: nl=<100 ug/mL b. CPK-MB Creatinine Phosphokinase i. Follow up test to CPK in order to determine if increased CPK value was due to heart damage or skeletal muscle damage ii. Onset: 4-6 hours iii. Peak: 15-20 hours iv. Return to Normal: 2-3 days v. N or S Values: sig= >5% of total c. LDH – Lactate Dehydrogenase i. High levels indicate tissue damage ii. Onset: 8-12 hours V. iii. Peak: 2-4 days iv. Return to Normal: 7-10 days v. N or S Values: nl= 150-300 U/mL d. LDH-1 i. Primarily found in the heart muscle and RBC ii. Onset: 6-14 hours iii. Peak: 1-2 days iv. Return to Normal: 3-4 days v. N or S Values: sig= >30-35% of total e. SGOT- Serum glutamic oxaloacetic transaminase i. Releases into blood stream when there is heart tissue damage ii. Onset: 8-12 hours iii. Peak: 1-2 days iv. Return to Normal: 3-6 days v. N or S Values: nl= 8-40 U/mL f. Troponin I, and Troponin T i. Increase in levels may indicate heart damage from heart attack ii. Onset: 2-6 hours iii. Peak: 15-20 days iv. Return to Normal: 7 days v. N or S Values: nl= < 0.5 ngml Electrocardiography a. Continuous monitoring: hardwire, telemetry b. Continuous ambulatory monitoring c. Transtelephonic monitoring d. Wireless mobile monitoring e. Cardiac Stress testing i. Exercise Stress testing ii. Pharmocologic stress testing f. Echocardiography i. Transthoracic (ECHO) 1. Through the chest ii. Transesophageal (TEE) 1. Down the throat g. 12 lead ECG h. Electrocardiogram i. Electrode Placement 1. 2. We use Lead II ii. Electrode Adhesion 1. Shave or cut hair from electrode site a. In emergency can use one set of electrodes to rip hair away from desired location 2. Clean each site thoroughly with soap and water or a non alcoholic wipe a. Alcohol is discouraged because it can dry the skin and diminish electrical flow 3. Dry skin vigorously to increase capillary blood flow to tissues 4. Use skin prep pad or 4x4 (something abrasive) in order to remove part of stratum corneum for better conduction iii. Reading an EKG (Video version) 1. Evaluate P wave a. Represents atrial depolarization b. 0.05-0.25 mV c. 0.06-0.11 seconds d. If not looking consistent may be something wrong with SA Node 2. Evaluate Atrial Rhythm a. Look for consistency 3. Evaluate Atrial Rate a. Using Methods 1, 2, or 3 4. Calculate Duration of PR Interval a. Indicates AV conduction time b. From beginning of P wave to beginning of QRS Complex c. 0.12-0.2 seconds d. Interval will shorten with increased HR 5. Evaluate Ventricular Rhythm 6. Evaluate ventricular rate a. Used for HR b. Count QRS Complexes 7. Calculate duration of QRS Complex a. Indicates ventricular depolarization (ventricular contracting) b. Measure from the end of the PR Interval to the end of S wave c. 0.04-0.12 seconds 8. Calculate Duration of QT Interval a. Time of ventricular activity including both depolarization and repolarization b. May get prolonged by anti-biotics c. Measured from beginning of the QRS Complex to the end of the T wave d. 0.36-0.44 seconds 9. Although not part of reading the EKG, the ST segment represents the early part of ventricular repolarization a. Goes from the end of the QRS Complex to the beginning of the T wave b. Is typically flat, being neither positive nor negative relative to the baseline 10. If a U wave is most common for bradycardia. However, prominent U waves may indicate hypokalemia 11. T wave represents full ventricular repolarization 12. Q wave may represent Myocardial Infarction. Only significant if they are ¼ the height of the positively inflected QRS complex 13. STEMI- elevated ST segment indicates myocardial infarction iv. Reading an EKG (Cardiac Packet Version) 1. Is it regular 2. What is the rate 3. What is the PR Interval 4. P waves (present, normal, all the same) 5. How long is the QRS Complex 6. Is there a QRS after every P wave VI. 7. Look at ST segment 8. Look at QT interval 9. T waves and U waves if present (primarily amplitude) v. EKG changes seen with electrolyte imbalances 1. Hyperkalemia: tented T waves 2. Hypokalemia: U wave 3. Hypercalcemia: short QT interval 4. Hypocalcemia: prolonged QT Interval 5. Quinidine Effects: wide knotched P waves, wide QT interval, presentation of U wave Diagnostic Tests a. Radionuclide Imaging i. Myocardial perfusion imaging (Nuclear stress test) 1. Non-invasive imaging test that shows how well blood perfuses through the heart muscle. 2. Will also show areas of the heart muscle that aren’t getting enough blood flow 3. Examines blood flow during exercise and rest (if cant exercise will be given medication) 4. Uses tracers (radioactive) that can be captured by gamma camera ii. Computed Tomography 1. Uses x ray to create sliced images of the internal structures 2. Helps to look at blood vessels and organs iii. Positron emission tomography 1. Uses radioactive tracers 2. Tracks blood flow and perfusion iv. Magnetic Resonance Angiography 1. Non invasive 2. Looks at blood vessels 3. NO METAL b. Cardiac Catheterization i. Invasive procedure study used to measure cardiac chamber pressures ii. Assess patency of coronary arteries iii. Requires EKG, hemodynamics monitoring iv. Emergency equipment must be available v. Must assess allergies and blood work prior to procedure Heart Rhythms I. Atrial Rhythms a. Premature Atrial Complex i. Occurs when an electrical impulse starts in the atrium before the next normal impulse of the sinus node ii. May be caused by caffeine, alcohol, nicotine, stretched atrial myocardium, anxiety, hypokalemia, or atrial ischemia iii. On EKG 1. Early P waves 2. Short PP interval b. Atrial Flutter i. Occurs because conduction defect in the atrium causes a rapid, regular atrial rate between 250-400 bpm 1. Atrial rate is faster than the AV node can conduct so not all atrial impulses are conducted into ventricles causing therapeutic block at the AV Node ii. Often in patients with COPD, pulmonary hypertension, valvular disease iii. On EKG 1. Atrial rate between 250-400bpm 2. Ventricular rate between 75-100 bpm 3. P waves will be saw toothed shape and are then referred to as F waves 4. Multiple F waves may appear 5. P:QRS 2:1, 3:1, 4:1 c. Atrial Fibrillation i. Atrial electrical activation that causes a rapid, disorganized, and uncoordinated twitching of atrial musculature ii. Most common dysrhythmia iii. On EKG 1. Atrial rate is 300-600 bpm 2. Ventricle rate is 120-200 bpm 3. A and V rates will be highly irregular 4. No discernible P waves- referred to as F waves 5. PR interval cannot be measured II. Junctional Rhythms a. Junctional Rhythm i. AV Node instead of the SA Node becomes the pacemaker of the heart ii. On EKG 1. Ventricular rate 40-60bpm 2. P wave may be absent b. Nonparoxysmal Junctional Tachycardia i. Caused by enhanced automaticity in the junctional area, resulting in a rhythm similar to JR except at a rate of 70-120 bpm c. Atrioventricular Nodal Reentry Tachycardia i. Impulse is conducted to an area in the AV Node that causes the umpulse to be rerouted back into the same area over and over again at a very fast rate. It is also then conducted into the ventricles ii. On EKG 1. Atrial rate is 150-250bpm 2. Ventricular rate is 120-200 bpm 3. P wave is difficult to discern III. Ventricular dysrhythmias a. Premature Ventricular Complex i. Impulse that starts in a ventricle and is conducted through the ventricles before the next normal sinus impulse ii. Can occur in healthy people especially with intake of caffeine, nicotine, or alcohol iii. On EKG 1. V and A rhythms are irregular 2. P wave may be hidden in the QRS or T b. Ventricular Tachycardia i. Defined as three of more PVC’s in a row occurring at a rate exceeding 100bpm ii. On EKG 1. V rate is 100-200bpm 2. P wave difficult to detect c. Ventricular Fibrillation i. Rapid, disorganized ventricular rhythm that causes ineffective quivering of the ventricles ii. On EKG 1. No atrial activity seen 2. V rate is greater than 300 bpm 3. V rhythm highly irregular 4. QRS irregular without recognizable complexes d. Idioventricular Rhythm i. Impulse starts in the conduction system below the AV Node ii. On EKG 1. V rate is 20-40 bpm 2. QRS is bizarre and abnormal shaped e. Ventricular Asystole i. Flatline