* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Everything You Wanted to Know About Pituitary Hormone
Gynecomastia wikipedia , lookup
Sexually dimorphic nucleus wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hormonal breast enhancement wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Hypothalamus wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Testosterone wikipedia , lookup
Hypothyroidism wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Kallmann syndrome wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Congenital adrenal hyperplasia due to 21-hydroxylase deficiency wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Hormone replacement therapy (female-to-male) wikipedia , lookup
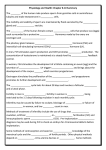
Theodore C. Friedman, M.D., Ph.D. Associate Professor of Medicine - UCLA Chief, Division of Endocrinology, Molecular Medicine and Metabolism Charles R. Drew University Everything You Wanted to Know About Pituitary Hormone Replacement That Your Doctor Never Told You MAGIC Foundation Affected Adult Convention February 11, 2007 Pituitary Hormone Replacement What’s the Big Deal? • Pituitary disorders are common, but experts in treating them are not! • Small changes in replacement may make a big improvement in symptoms • Many endocrinologists do not understand how to properly replace patients with hypopituitarism – They do not understand (or don’t believe in) monitoring hormone levels • We need to do more! What’s the Big Deal, Doc? (cont.) • Patients with hypopituitarism that receive conventional therapy have increased mortality – This is suggested - but not proven - to be due to GH deficiency (Rosen and Bengtsson, Lancet, 1990, 336:285; Bates, et al., JCEM, 1996, 81:1169) • The quality of life was seen to decrease in patients with hypopituitarism – This may be due to suboptimum replacement of pituitary hormones Hormonal Axes • Adrenal (corticotropes)=CRH-ACTH-Cortisol • Thyroid (thyrotropes)= TRH-TSH-T4/T3 • Gonads (gonadotropes)= GnRH-LH/FSHTestosterone/estrogen • GH (sommatotropes) =GHRH-GH-IGF1 • Prolactin-sommatomamotropes • Posterior Pituitary-ADH, oxytocin Order of Hormone Deficiencies • • • • • • GH Gonadotropins (FSH, LH) TSH ACTH Prolactin Posterior pituitary hormones Glucocorticoid Insufficiency • Needs significant impairment of pituitary function • Classically, pituitary only affects cortisol, not mineralocorticoids (salt regulating hormones from the adrenals) • Can be life-threatening, but most patients do surprisingly well • Fatigue, lethargy, nausea, vomiting, joint pains, abdominal pain, weight loss, hypoglycemia (rare in adults), low sodium Glucocorticoid Insufficiency Diagnosis • Screen with 8 AM cortisol • If < 3 mg/dL-clear glucocorticoid insufficiency • If > 12 mg/dL and not severe stress, glucocorticoid insufficiency unlikely • 3-12 mg/dL-gray zone-do cosyntropin test (unless acute) • Stimulation tests need to be performed in a place that has expertise. Standard (1 hr) Cosyntropin Test • 250 mg of IV cosyntropin (ACTH1-24) • Plasma cortisol at time 0, 30 and 60 minutes – Any value over 20 mg/dL is normal • If peak response is less than 10 mg/dL, glucocorticoid replacement is required • If peak response is between 10 and 20 mg/dL – Glucocorticoid replacement is recommended during stresses, – Otherwise replacement needs to be individualized One mcg Cosyntropin Test • 1 mg of IV cosyntropin (ACTH1-24) (diluted in saline) • Plasma cortisol at time 0 and 30 minutes (action ends after 30 min) – Any value over 18 mg/dL is normal (?) • Will pick up more mild cases – Should they be treated or just covered? 1 mg vs. 250 mg Cosyntropin Test • 250 mg is supraphysiological – Will miss subtle glucocorticoid insufficiency • Mild ACTH deficiency, like mild hypothyroidism exists – Consequences of misdiagnosis may be severe • Why do the test? – My Philosophy • Want as many patients to know they have borderline HPA function • Want as few patients as possible on replacement steroids – True physiological replacement (10-15 mg/day of hydrocortisone), though, may be relatively benign – Cutoffs unclear, but I use cortisol of 18 ug/dL for one mcg and 20 ug/dL for 250 mcg test ITT/ metyrapone Tests • • • • Both can exacerbate glucocorticoid insufficiency Both are non-physiological Rarely needed ITT requires physician supervision, but can also be used to diagnose GH deficiency • Patients feel horrible after metyrapone test Daily Cortisol Production Rate In Man • Esteban et al. (JCEM, 72: 39, 1991) measured daily cortisol production rates in normal volunteers with a stable cortisol isotope method – 9.9 +/- 2.7 mg/day, 5.7 mg/m2 day • Most, but not all of oral cortisol is absorbed – Need to take 12-15 mg/day • Most glucocorticoid replacement is supraphysiological – Leads to osteoporosis, glucose intolerance and increased infections • True physiological replacement is likely to be benign • Cortisol secretion is highly regulated – Stress, circadian rhythm-doubt we can do as well as mother nature Glucocorticoid Replacement • Glucocorticoids can be dangerous – Should be clear indication for treatment • Patients with burn out (“adrenal fatigue”) have normal HPA axis (Mommersteeg et al., Psychoneuroendocrinology 2006) • Increase stress should activate, not “burn out” the adrenals • Would be careful about “isocort” or other adrenal extracts – These contain cortisol plus other bioactive adrenal hormones – Once you start, hard to get off, so decide careful Glucocorticoid Replacement (2) • Most patients are over-treated • Earliest manifestation of excess treatment is – Easy bruisability – Weight gain, central obesity, etc. • Earliest manifestation of inadequate treatment is joint pain • Reasonable to mimic circadian rhythm with most or all cortisol, given first thing in the morning • Other studies suggest highest dose in AM, with lower doses throughout the day – May mimic cortisol secretion • Want to avoid large nighttime administration as it could lead to sleep disturbances – But some patients need a bit of cortisol to go into deep sleep Glucocorticoid Replacement (3) • No studies comparing different treatment regimens • My approach is to use hydrocortisone mainly in AM • Aim for dose between 15 and 20 mg/day in a woman – Slightly higher in a man • Decrease dose slowly until some symptoms develop, then go back a dose • Small changes make a big difference, especially between 15 and 25 mg a day of hydrocortisone • Increase dose with illness • Short term: it’s better to err on giving more • Long term: it’s better to give less • Can take 5 mg more during heavy exercise Glucocorticoid Replacement (Try To Avoid Adrenal Crisis) • Patients on lower doses of glucocorticoids more likely to have a crisis – But they still do better long-term • • • • • • • • • Exacerbated by the flu, other illnesses Less likely in hypopit patients than in those with adrenal disease Med-alert bracelet Double glucocorticoid dose first Then Act-O-vial 100 mg solucortef plus syringe, available for IM injection Lots of salt and fluids (Gatorade) Florinef (synthetic aldosterone) Lots of anti-nausea meds (zofran, phenergan), pain meds, anxiety meds (ativan) on hand Do not be stoic - GO TO ER! Monitoring Glucocorticoid Replacement • Signs and Symptoms – 24 hr urine for 17-hydroxysteroids (17-OHS) – UFC tends to be high during replacement • In replacement, most of UFC excretion occurs right after taking the cortisol – High doses are not bound to CBG • Exceed reabsorption by the kidney • 17-OHS (corrected for creatinine excretion in g/day) reflects cortisol metabolism – More integrated throughout the day • Other hormones affect glucocorticoid metabolism Central Hypothyroidism • Common, even with small tumors • Mild cases may be more manifest clinically – More than “subclinical hypothyroidism” due to actual low thyroid hormones in central hypothyroidism • • • • Similar signs/symptoms as in primary hypothyroidism Low free T4 in the face of lowish TSH In mild cases, free T4 between 0.7 and 1.0 ng/dL T3 usually not helpful Central Hypothyroidism Confirmation • TRH test – Hard to get – Can show blunted TSH response to TRH • Nocturnal TSH test – TSH should rise at least 1.5-fold between 5 PM and midnight in normals – Not in patients with central disease – Not easy to get blood at midnight • Usually base on baseline free T4 and TSH Central Hypothyroidism Treatment • L-thyroxine in most cases – Some patients with primary hypothyroidism, though, do better on T4/T3 combinations (Buneviius et al, NEJM, 1999, 340:424) – Some patients with central hypothyroidism may do better on T4/T3 or T4/Armour combinations • GH deficiency can lead to impaired T4 to T3 conversion – T3 may be especially beneficial in central hypothyroidism • Treating with GH can decrease FT4 levels and unmask central hypothyroidism – Recommended to treat borderline central hyopthyroidism to get full benefit of GH therapy Central Hypothyroidism Treatment (2) • Thyroid hormone treatment increases cortisol breakdown – Can put someone with adrenal insufficiency into an adrenal crisis • Make sure adrenal insufficiency is considered/tested before starting thyroid hormone • Monitor by aiming for free T4 in upper-normal range (1.5-1.7 ng/dL) • TSH will be suppressed – Usually not worth measuring after starting treatment • Patients with both primary hypothyroidism and a central component – Should also be monitored with free T4 and not TSH measurements Growth Hormone Deficiency • Patients with hypopituitarism have increased mortality – Suggested, but not proven, to be due to GH deficiency • Growth hormone deficiency in adults results in – – – – – – – – – Decreased bone formation Increased fat mass (central obesity) Decreased muscle mass Lipid abnormalities Increased thickness of blood vessels Increased inflammatory markers Impaired quality of life Increased number of sick days Impaired exercise tolerance • Microadenomas may cause GH deficiency Growth Hormone Deficiency Diagnosis • Screen with IGF-I – If in top 75% of normal range for age and sex (> 150 ng/mL), GH deficiency unlikely – If < 75 ng/mL, GH deficiency likely • Stimulation testing – Arginine-GHRH- GH deficient if GH (by RIA) is < 9 ng/mL – (RIA is 2X ICMA; 9 by RIA=4.5 by ICMA) – ITT- GH deficient if GH (by RIA) is < 5 ng/mL • I use Arginine-GHRH, unless need to use ITT for adrenal insufficiency workup – Blunted response in obesity – Blunted response in males Growth Hormone Deficiency Diagnosis (cont.) • Stimulation tests are non-physiological – Day-to-day GH/IGF-I axis more important than with stimulation • Unclear what to do with patient with hypopituitarism, lowish IGF-I and normal stimulation testing Adult Growth Hormone Treatment • 10% of dose/body weight than that of children • Don’t need to adjust for body weight • Women, especially on oral estrogens, need higher doses than men • Start at 0.4 mg/day in women, 0.2 mg/day in men • Final dose varies widely and can not be predicted • Titrate upwards with IGF-I measurements monthly • Aim for IGF-I in upper 1/3 of normal range – 300 ng/mL, but depends on assays – Usually not much improvement in symptoms until in this range • Too much GH-joint (hand mainly) swelling and pain Diabetes Insipidus • Defect in ADH – Also called AVP – Posterior pituitary • Excessive urination and thirst • Mild cases are probably common and worthy of treatment • Chronic polyuria may lead to bladder/kidney problems • How many times are you waking up at night? Diabetes Insipidus (2) • I screen by having the patient collect urine for 24 hours, then measure the volume – Greater than 3 L indicates diabetes insipidus likely • I confirm with a 12 hour fast (no water!) – Collect an 8 AM serum and urine osmolality and ADH level • DI – High serum osmolality (>300 mOsm/kg) – Low urine osmolality (<500 mOsm/kg) – Low ADH (< 1.5 pg/mL) • Formal water deprivation test probably not needed Diabetes Insipidus (cont.) • DDAVP pills probably the best – Most endocrinologists still recommend nasal puffs • Take most of the dose at night to prevent waking up at night • Should have a period of “break-through” urination, usually in the evening. • Treatment is pretty benign Abnormalities Of Gonadotropes • Gonadal Axis – GnRH-LH/FSH -Testosterone/estrogen/progesterone • • • • • • • Lack of ovulation Irregular or no periods Infertility Vaginal dryness Osteoporosis Decreased libido Possibly poor sense of well-being What To Do If You Have Gonadotropin Dysfunction? • If trying to get pregnant – Determine ovulation – See reproductive endocrinologist • If not trying to get pregnant – Replace estrogen – Testosterone – Possibly Progesterone Estrogen Replacement in Women • Amenorrhea or oligomenorrhea indicates gonadotropin deficiency • Irregular periods may be early sign of pituitary dysfunction • Previous WHI and HERS studies on post-menopausal women were not on estrogen – Average age in WHI: 63 • Younger hypogonadal women likely to benefit from estrogen replacement • Young women ‘feel better” on higher estrogen preparations – May require higher doses than post-menopausal women – Less clear for older women • Replacement and decision to have periods or not based on patient preference and age Estrogen Replacement in Women • Choices include (cont.) – Premarin (pregnant mare urine, “conjugated estrogen”, multiple estrogenic compounds) – Oral estrogen compounds (estrace) – Birth control pills • Contain relatively high doses progesterone and low doses estrogen – – – – Estrogen patches (Climara, Vivelle) Estrogen creams (Estrogel) Vaginal estrogen (Fem-ring, Estring) Compounded Estrogen (creams, sublingual drops, pills) Oral Estrogen Replacement, But Not Other Routes • First pass effect in the liver • Blocks the action of GH at the liver to raise IGF-1 – Leads to high GH and low IGF-1 (both bad) • Raises sex hormone binding globulin (SHBG) • Raises total testosterone, but decreases free testosterone – Low free testosterone may lead to decreased libido (and maybe low energy, decreased muscle mass) • Recent study showed that effects of oral estrogens (including birth control pills) decrease free testosterone levels for at least a year after discontinuing Oral Estrogen Replacement, But Not Other Routes (2) • Raises thyroid-binding globulin (TBG) – Can lead to an increase in thyroid hormone requirements • Raises cortisol-binding globulin (CBG) – Leads to high levels of total cortisol – Makes testing for adrenal insufficiency difficult Oral Estrogen Replacement • In women with hypopituitarism, avoid it! What Type of Estrogen is Best? • Ovaries make estrone (E1), estradiol (E2), estriol (E3) • Estradiol is most abundant (“bioidentical”) • Slight evidence that estrone is detrimental (breast cancer) and estriol is good • Oral estrogens get converted to estrone • I use mainly estradiol (Climara or Estrogel) – Titrate dose so that estradiol is in the upper normal range for the follicular period (50-100 pg/mL) • Some compounding pharmacies encourage bi-est (estradiol/ estriol) or tri-est (estrone/ estradiol/ estriol) • Young hypopit patients should take estrogen daily Should You Take Estrogen/Progesterone to Induce A Period? • Taking 5-10 mg of Provera (synthetic Progestin) or 100-200 mg of Prometrium (progesterone “bioidentical”) for 10 days, then stopping, will usually induce a period • Taking 2.5 mg of Provera or 100 mg of Prometrium daily will usually not induce a period • I tend to have women less than 40-45 have a monthly period, older than that not to have a period • Women with an intake uterus should take a progesterone Androgen Replacement - Men • Symptoms include low libido, impotence, fatigue, decreased muscle mass • Soft testes may be the earliest sign of gonadotropin deficiency • Small testes or gynecomastia may be seen – Helpful in borderline testosterone levels • Measure total testosterone levels – If < 200 ng/dL, testosterone deficiency likely • If 200-350 ng/dL – Borderline result, use clinical judgment or – measure bioavailable testosterone (free plus available) or – free testosterone by equilibrium dialysis, if possible • LH/FSH helpful only to exclude primary hypogonadism Androgen Replacement – Men (2) • Testosterone gel or patch probably preferable to injections • HCG is another possibility – Making a come-back (doesn’t cause testicular shrinkage) – May be used in combination with other treatments • Aim for total testosterone levels in the upper normal range • Androderm patch 5 mg – May need 2 patches to achieve appropriate levels (lots of skin irritation) • AndroGel 1% 5 G delivers 5 mg – May also need higher doses (7.5 or 10 G) – Comes in a pump • Graded dosing for all preparations would be desirable What’s the Problem? • Most patients are – – – – On too much cortisol On not enough thyroid medication On not enough growth hormone Not on testosterone • These lead to weight gain and depression • Get your doses adjusted! Hormonal Interactions • Treating a patient with adrenal insufficiency and hypothyroidism with thyroid hormone – Increases the breakdown of cortisol – May lead to an adrenal crisis • Thyroid hormone may also – increase catabolism of other hormones (GH, testosterone) – lead to increased requirements when thyroid dose is increased • Treating with GH may increase T4 to T3 conversion – Dose of T3 (if on T3) may need to be reduced • GH may decrease TSH – Treating with GH may unmask or exacerbate central hypothyroidism – May need a higher dose of thyroid hormone once GH treatment is started Hormonal Interactions (2) • Oral, but not transdermal estrogens, increase the need for Lthyroxine in women with hypothyroidism (Arafah, BM, NEJM, 344:1743) • Oral, but not transdermal estrogens, increase the need for GH replacement • Stopping oral estrogens leads to an elevated IGF-1 (hand swelling) • Patients on GH replacement should probably not be on oral estrogens • Treating adrenal insufficiency may unmask Diabetes Insipidus Hormonal Interactions (3) • Increased GH/ IGF-I leads to lower levels of cortisol (11HSD1) – Thus, treating a patient with hypopituitarism with GH will decrease cortisol levels • We had one patient that was over-replaced on glucocorticoids, under-replaced on thyroid hormone and not treated with GH – We started GH, decreased her glucocorticoids and increased her L-thyroxine – she went into adrenal crisis • Make changes slowly • Monitor frequently Testosterone for Women The Physiologic Role Of Testosterone In Women Remains Poorly Understood • Previous studies of testosterone supplementation, largely in surgically or naturally menopausal women, have reported improvements in – subjective measures of sexual function – sense of well being – variable changes in markers of bone formation and resorption Potential Benefits of Androgen Supplementation in Women • • • • • • • • Improved sexual function Improved bone mineral density Improved muscle mass and function Improved mood and sense of well-being Improved cognitive function Amelioration of autoimmune disease Amelioration of premenstrual syndrome Improvement in dry eye syndrome Testosterone in Hypopituitarism • A recent large study demonstrated that patients with hypopituitarism have increased mortality – mainly due to cardiovascular, respiratory, and cerebrovascular events • Hypopituitarism in women is associated with a number of symptoms, including – – – – Obesity Poor quality of life Decreased libido Osteopenia • These persist in spite of standard hormonal replacement Severe Androgen Deficiency in Women with Hypopituitarism • Women with hypopituitarism – Have impairment of both the adrenal and ovarian sources of androgen production – Have lower T and DHEAS levels than women with ovarian failure alone Ref Miller et al., J Clin Endocrinol Metab 2001;86:561-7. Potential Adverse Effects Associated with Testosterone Supplementation • The potential risks of testosterone administration to women include – – – – – virilization hirsutism acne effects on plasma lipids effects on behavior Testosterone Delivery • Currently, the only FDA-approved drug for testosterone in women is Estratest – Contains methyl testosterone – It is a compound that, when given orally, is associated with liver toxicity in animals and humans • DHEA is a considered a prohormone of testosterone – Most of its actions are probably due to binding to the testosterone receptor • DHEA (25-50 mg)/day is a reasonable approach in women • Other possibilities include – – – – Patches (Procter & Gamble, no FDA approval, 2005) Gels (compounded or investigational) Injections Sublingual Testosterone in Hypopituitarism • Miller et al. JCEM 91, 1683-1690, 2006 • Design: This was a 12-month randomized, placebo-controlled study • Study Participants: 51 women of reproductive age with androgen deficiency due to hypopituitarism participated • Intervention: Physiologic testosterone administration using a patch that delivers 300 µg daily or placebo was administered Testosterone in Hypopituitarism • Results: Mean free testosterone increased into the normal range during T administration. • Mean hip (P = 0.023) and radius (P = 0.007), bone mineral density increased in the group receiving testosterone, compared with placebo, • In testosterone treated group, fat-free mass (P = 0.040) and thigh muscle area (P = 0.038) increased, but there was no change in fat mass. • Mood (P = 0.029) and sexual function (P = 0.044) improved, as did some aspects of quality of life, but not cognitive function. • Testosterone at physiologic replacement levels was well tolerated, with few side effects. Demographic Characteristics of Women with Hypopituitarism (T < 20 ng/dL) Name Patients A.P. C.B. C.O.W. D.G. E.S. J.R. K.T. M.R. M.V. M.Z. N.S. S.G. Mean SD Age BMI Ethnicity Disorder Surgery 24 41 43 29 28 38 48 31 26 44 50 37 36.6 8.8 28.6 30.5 25.8 34.9 34.6 34.6 22.8 28.1 28.1 21.1 30.2 24.0 28.6 3.6 H H H H H C C H H H C H Acromegaly Acromegaly Sheehan's Non-secreting Macroadenoma Craniopharygioma Acromegaly Cushings Prolactinoma Craniopharyn Sheehans Hypothalamic-Pituitary Dysfunction Non-secreting Macroadenoma Y Y* N Y Y Y* Y Y Y N N Y 12 patients completed most of the study Deficiencies Go, ADH Go Go, GH, TSH Go, TSH, ADH Go, GH, TSH, ACTH, ADH Go,TSH, ACTH, ADH Go, GH, TSH, ACTH Go, GH, TSH, ACTH Go, GH, TSH, ACTH, ADH Go, TSH Go, GH, TSH, ACTH Go, GH, ACTH GH status high nl nl on gh-now nl not tested on gh-now nl nl on gh-now nl on gh-now nl on gh-now nl not tested on gh-now nl not tested Testosterone Testosterone Levels in hypopituitary and Healthy Volunteers testosterone levels ng/dL 80.0 70.0 ** 60.0 50.0 40.0 30.0 20.0 10.0 0.0 Hypopituitarism Healthy Volunteers ** P < 0.0001 Cholesterol Cholesterol 300 * 250 mg/dL 200 150 100 50 0 Hypopituitarism Healthy Volunteers * P < 0.005 LdL Cholesterol LdL 250 200 * mg/dL 150 100 50 0 Hypopituitarism Healthy Volunteers * P < 0.05 HdL Cholesterol P =NS HdL 120 100 mg/dL 80 60 40 20 0 Hypopituitarism Healthy Volunteers Triglycerides Triglycerides 300 * 250 mg/dL 200 150 100 50 0 Hypopituitarism Healthy Volunteers * P < 0.05 400 m walk 400m Walk 300 * 250 Seconds 200 150 100 50 0 Hypopituitarism Healthy Volunteers * P < 0.05 Chest press Chest Press 50.0 45.0 * 40.0 35.0 kg 30.0 25.0 20.0 15.0 10.0 5.0 0.0 Hypopituitarism Healthy Volunteers * P < 0.05 SCL - 90 (higher score worse) ** P < 0.0001 SCL-90R (GSI) 2.50 ** 2.00 1.50 1.00 0.50 0.00 Hypopituitarism Healthy Volunteers Female Sexual Distress Scale 35 * score range 0 to 48 30 normal range: <15; abnormal range: 15+ 25 20 p < 0.0001 15 10 5 0 Healthy Patients Hypopituitarism FSFI-Desire 4.5 4 Levels of Desire 3.5 P<0.0001 3 2.5 * 2 1.5 1 0.5 0 Healthy Volunteers Hypopituitarism FSFI-Orgasm 5 Levels of Orgasm 4.5 4 3.5 P<0.0001 3 2.5 2 * 1.5 1 0.5 0 Healthy Volunteers Hypopituitarism Less Pain Experienced During Vaginal Penetration FSFI-Pain 5 4.5 4 P<0.001 3.5 3 * 2.5 2 1.5 1 0.5 0 Healthy Volunteers Hypopituitarism FSFI-Lubrication 5 4.5 Level of Lubrication 4 P<0.001 3.5 3 2.5 * 2 * 1.5 1 0.5 0 Healthy Volunteers Hypopituitarism FSFI-Arousal 4.5 4 Levels of Arousal 3.5 3 2.5 P<0.001 2 * 1.5 1 0.5 0 Healthy Volunteers Hypopituitarism FSFI-Satisfaction 4.5 4 Levels of Satisfaction 3.5 3 P<0.0002 2.5 * 2 1.5 1 0.5 0 Healthy Volunteers Hypopituitarism Warm Sensation-Vagina 50 P<0.05 units * 45 40 Healthy Volunteers Hypopituitarism Elevated warm sensation threshold indicates impairment of C-fiber sensory nerve function Vibratory Threshold-Vagina p < 0.05 12 * 10 units 8 6 4 2 0 Healthy Volunteers Hypopituitarism Elevated vibratory threshold indicates impairment of A-beta sensory nerve function Objective Sexual Function (Blood-flow) Labia-post-stimulation Blood Flow Labia -Post 100.0 90.0 80.0 cm/sec 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 Healthy Volunteers 4 patients and 2 normals below the cut-off of 30 cm/sec Hypopituitarism Objective Sexual Function (Blood-flow) Clitoral-post-stimulation Blood Flow Clitoris-Post 100.0 90.0 80.0 cm/sec 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 Healthy Volunteers 4 patients and 1 normal below the cut-off of 30 cm/sec Hypopituitarism Differences in Pre-Post Clitoral Blood Flow 40 35 P<0.05 cm/sec 30 * 25 20 15 10 5 0 Healthy Volunteers Hypopituitarism Conclusions Of Short-Term Studies • • • • • • • Low free and total serum testosterone levels in patients Impaired chest press strength and 400 m walk High cholesterol, LdL and TG Very reduced psychological well-being Impaired vaginal, but not clitoral thresholds Slightly impaired genital blood flow Recruitment is ongoing Testosterone Replacement Study at Drew University • Funded as part of Reproductive Center Grant • Now recruiting patients • 80 women (ages 18 to 50 years) with testosterone deficiency secondary to hypopituitarism – Will be randomized to receive either placebo or transdermal testosterone gel • Leading to a targeted serum testosterone in the upper range of normal – Double-blind study of 6 months duration • All patients will be on stable physiological replacement regimens for other hormones including – Growth hormone – Transdermal estrogen replacement Criteria for Subjects • • • • • • Women ages 18 to 55 Pituitary gland problems Low serum testosterone level (can be tested at study site) Written informed consent No other significant medical conditions Patients must discontinue their current testosterone or DHEA replacement, if on either of these hormones Testosterone Replacement Study at Drew University • Location – King/Drew Medical Center in Willowbrook – UCLA in West Los Angeles • Patient Compensation – Up to $1500, plus pituitary hormone medications provided by the study • Recruitment ongoing – Call 323-563-9385 or – email [email protected] Study Perks For Patients • Free growth hormone during all parts of the study • Open label period – All patients would get testosterone gel for one year following randomization period • Free hormonal testing including GH testing • Climara patch and Provera supplied without charge Conclusion • Sexual dysfunction in women matters! • Psychological dysfunction in women matters! – We hope this study will address these problems • We expect this study will – accurately assess the important benefits and deleterious effects of physiological testosterone replacement in women with hypopituitarism • At the conclusion of this study, we expect to – determine whether it is of benefit to add testosterone to the standard hormonal replacement for women with hypopituitarism For More Information and To Schedule An Appointment With Dr. Friedman • www.goodhormonehealth.com • [email protected] • My book on thyroid diseases – “ The Everything Health Guide to Thyroid Disease” – Published by Adams Media – Just came out – Available at Amazon.com A BIG Thanks! • To Magic Foundation for inviting me and doing great work! • To Dianne Tambourine for hosting a great conference