* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Digestive System Part Two
Liver support systems wikipedia , lookup
Wilson's disease wikipedia , lookup
Colonoscopy wikipedia , lookup
Liver transplantation wikipedia , lookup
Liver cancer wikipedia , lookup
Cholangiocarcinoma wikipedia , lookup
Hepatic encephalopathy wikipedia , lookup
Intestine transplantation wikipedia , lookup
Hepatotoxicity wikipedia , lookup
Fecal incontinence wikipedia , lookup
Surgical management of fecal incontinence wikipedia , lookup
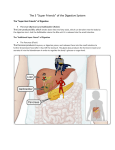
Digestive System Part 2 Anatomy and Physiology of the Digestive System Small intestine Major organ of digestion and absorption 2–4 m long; from pyloric sphincter to ileocecal valve Subdivisions Duodenum Jejunum Ileum Anatomy and Physiology of the Digestive System Small intestine Structural modifications Villi Intestinal glands Mucosa Submucosa Mouth (oral cavity) Tongue Esophagus Liver Gallbladder Duodenum Jejunum Small intestine Ileum Anus Parotid gland Sublingual gland Salivary Submandibular glands gland Pharynx Stomach Pancreas (Spleen) Transverse colon Descending colon Ascending colon Large Cecum intestine Sigmoid colon Rectum Vermiform appendix Anal canal Figure 23.1 Vein carrying blood to hepatic portal vessel Muscle layers Circular folds Villi Lumen (a) Figure 23.22a Microvilli (brush border) Absorptive cells Lacteal Goblet cell Blood capillaries Mucosa associated lymphoid tissue Intestinal crypt Muscularis mucosae Duodenal gland (b) Vilus Enteroendocrine cells Venule Lymphatic vessel Submucosa Figure 23.22b Microvilli (b) Absorptive cell Figure 23.3b Anatomy and Physiology of the Digestive System Chemical digestion in the small intestine Food entering SI = partially digested Intestinal juice Water, mucous Crypt cells produce lysozyme Microvilli (brush border) Absorptive cells Lacteal Goblet cell Blood capillaries Mucosa associated lymphoid tissue Intestinal crypt Muscularis mucosae Duodenal gland (b) Villus Enteroendocrine cells Venule Lymphatic vessel Submucosa Figure 23.22b Anatomy and Physiology of the Digestive System Chemical digestion in the small intestine Pancreatic juice Enzymes Amylase o Carbohydates Lipase o Fats Trypsinogen, chymotrypsinogen, carboxypeptidase o Activated to digest protein Sodium bicarbonate Neutralize stomach acid Stomach Pancreas Epithelial cells Membrane-bound enteropeptidase Trypsinogen Trypsin (inactive) Chymotrypsin Chymotrypsinogen (inactive) Carboxypeptidase Procarboxypeptidase (inactive) Figure 23.27 Anatomy and Physiology of the Digestive System Chemical digestion in the small intestine Bile Emilsify lipids Disaccharides and peptidases Protective mucous secreted as well Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct and sphincter Accessory pancreatic duct Mucosa with folds Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter Tail of pancreas Pancreas Jejunum Duodenum Main pancreatic duct and sphincter Head of pancreas Figure 23.21 Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Pancreas Gallbladder Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Largest internal surface area of any body organ Blood supply Hepatic artery Hepatic-portal vein Hepatic vein Inferior vena cava (not part of hepatic portal system) Hepatic veins Liver Hepatic portal vein Small intestine Gastric veins Spleen Inferior vena cava Splenic vein Right gastroepiploic vein Inferior mesenteric vein Superior mesenteric vein Large intestine Rectum (c) The hepatic portal circulation. Copyright © 2010 Pearson Education, Inc. Figure 19.29c Interlobular veins (to hepatic vein) Central vein Sinusoids Bile canaliculi Plates of hepatocytes Bile duct (receives bile from bile canaliculi) Fenestrated lining (endothelial cells) of sinusoids Portal vein Hepatic macrophages in sinusoid walls Bile duct Portal venule Portal arteriole Portal triad (c) Copyright © 2010 Pearson Education, Inc. Figure 23.25c Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Microscopic compartments = lobules Lined by hepatocytes = screen blood o Store nutrients o Manage toxins Sternum Nipple Liver Bare area Falciform ligament Left lobe of liver Right lobe of liver Gallbladder (a) Round ligament (ligamentum teres) Figure 23.24a (a) Lobule Copyright © 2010 Pearson Education, Inc. (b) Central vein Connective tissue septum Figure 23.25a, b Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Hepatocyte functions Process blood borne nutrients Store fat-soluble vitamins Perform detoxification Produce ~900 ml bile per day Glucose is stored as glycogen Cystic, Hepatic and Bile ducts Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct and sphincter Accessory pancreatic duct Mucosa with folds Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter Copyright © 2010 Pearson Education, Inc. Tail of pancreas Pancreas Jejunum Duodenum Main pancreatic duct and sphincter Head of pancreas Figure 23.21 Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Bile Yellow-green, alkaline solution Bile salts o Cholesterol derivatives that function in fat emulsification and absorption Bilirubin o Pigment formed from heme Metabolized to form urobilinogen → stercobilin Lack of bile = grayish stools with fatty streaks (Acholic feces) Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Other functions Makes heparin and other plasma proteins Stores vitamins, minerals and lipid soluble toxins Stores nutrients Catabolizes nitrogenous wastes Anatomy and Physiology of the Digestive System Accessory digestive organs Liver Gallbladder Thin-walled muscular sac on the ventral surface of the liver Stores and concentrates bile by absorbing its water and ions Releases bile via the cystic duct o Flows into the bile duct Anatomy and Physiology of the Digestive System Accessory digestive organs Pancreas Function Delivers digestive fluids and NaHCO3 to duodenum via pancreatic duct Tissue types Endocrine o Islets of Langerhans → insulin and glucagon Exocrine o Acinar tissue → pancreatic juice Mouth (oral cavity) Tongue Esophagus Liver Gallbladder Duodenum Jejunum Small intestine Ileum Anus Parotid gland Sublingual gland Salivary Submandibular glands gland Pharynx Stomach Pancreas (Spleen) Transverse colon Descending colon Ascending colon Large Cecum intestine Sigmoid colon Rectum Vermiform appendix Anal canal Figure 23.1 Anatomy and Physiology of the Digestive System Accessory digestive organs Pancreas Secretion mediated by hormones Secretin o Released in response to acid o Stimulates release of base Cholecystokinin o Released when protein and fat enter intestine o Stimulates the release of bile and pancreatic juice Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct and sphincter Accessory pancreatic duct Mucosa with folds Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter Tail of pancreas Pancreas Jejunum Duodenum Main pancreatic duct and sphincter Head of pancreas Figure 23.21 Small duct Acinar cells Basement membrane Zymogen granules Rough endoplasmic reticulum (a) Figure 23.26a Slide 1 1 Chyme entering duodenum causes release of cholecystokinin (CCK) and secretin from duodenal enteroendocrine cells. 2 CCK (red dots) and secretin (yellow dots) enter the bloodstream. 3 CCK induces secretion of enzyme-rich pancreatic juice. Secretin causes secretion of HCO3–-rich pancreatic juice. 4 Bile salts and, to a lesser extent, secretin transported via bloodstream stimulate liver to produce bile more rapidly. 5 CCK (via bloodstream) causes gallbladder to contract and hepatopancreatic sphincter to relax; bile enters duodenum. 6 During cephalic and gastric phases, vagal nerve stimulation causes weak contractions of gallbladder. Figure 23.28 Anatomy and Physiology of the Digestive System Large intestine About 1.5 meters in length in a cadaver (SI about 6m long) Functions Vitamins, water, and electrolytes are reclaimed Propulsion of feces toward the anus Colon is not essential for life Left colic (splenic) flexure Transverse mesocolon Epiploic appendages Right colic (hepatic) flexure Transverse colon Superior mesenteric artery Haustrum Descending colon Ascending colon IIeum Cut edge of mesentery Teniae coli IIeocecal valve Cecum Vermiform appendix Sigmoid colon Rectum Anal canal (a) External anal sphincter Figure 23.29a Anatomy and Physiology of the Digestive System Regions Cecum Colon Rectum Anal canal Anatomy and Physiology of the Digestive System Regions Cecum Blind pouch Appendix attaches to this area Bacteria Immune function Anatomy and Physiology of the Digestive System Regions Colon Ascending Retroperitoneal Transverse Anchored via mesocolons (mesenteries) Descending Retroperitoneal Sigmoid Anchored via mesocolons (mesenteries) Greater omentum Transverse colon Transverse mesocolon Descending colon Jejunum Mesentery Sigmoid mesocolon Sigmoid colon Ileum (c) Figure 23.30c Liver Lesser omentum Pancreas Stomach Transverse mesocolon Duodenum Transverse colon Mesentery Greater omentum Jejunum Ileum Visceral peritoneum Parietal peritoneum (d) Urinary bladder Rectum Figure 23.30d Anatomy and Physiology of the Digestive System Regions Rectum Rectal valves stop feces from being passed with gas Anal canal Last segment of the large intestine Internal anal sphincter Smooth muscle (involuntary) Spinal reflex arcs External anal sphincter Skeletal muscle (voluntary) Rectal valve Rectum Hemorrhoidal veins Levator ani muscle Anal canal External anal sphincter Internal anal sphincter Anal columns Pectinate line Anal sinuses Anus (b) Figure 23.29b Anatomy and Physiology of the Digestive System Defectation Mass movements force feces into rectum Distension initiates spinal defecation reflex Parasympathetic signals Stimulate contraction of the sigmoid colon and rectum Relax the internal anal sphincter Conscious control allows relaxation of external anal sphincter Valsalva’s maneuver Impulses from cerebral cortex (conscious control) 1 Sensory nerve fibers Distension, or stretch, of the rectal walls due to movement of feces into the rectum stimulates stretch receptors there. The receptors transmit signals along afferent fibers to spinal cord neurons. 2 Voluntary motor nerve to external anal sphincter Sigmoid colon A spinal reflex is initiated in which parasympathetic motor (efferent) fibers stimulate contraction of the rectal walls and relaxation of the internal anal sphincter. Stretch receptors in wall Rectum External anal sphincter (skeletal muscle) Involuntary motor nerve (parasympathetic division) Internal anal sphincter (smooth muscle) 3 If it is convenient to defecate, voluntary motor neurons are inhibited, allowing the external anal sphincter to relax so that feces may pass. Figure 23.31 Questions?