* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biology 232
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
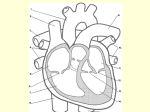
VT 106 Comparative Anatomy and Physiology Cardiovascular System CARDIOVASCULAR SYSTEM – HEART Function of the Heart pump – circulates blood through the blood vessels dual circulation pulmonary circuit – deoxygenated (blue) blood from tissues right heart lungs for oxygenation left heart systemic circuit – oxygenated (red) blood from pulmonary circuit left heart body tissues right heart External Anatomy of Heart apex – narrow caudal end base – wide cranial end where major blood vessels emerge lies in thoracic cavity within the mediastinum sits just dorsal to the sternum apex points to the left lies between 2nd – 7th ribs (size varies with species) pericardial sac (pericardium) – membrane surrounding heart 2 layers: fibrous pericardium – outer dense irregular connective tissue protects heart, prevents overstretching attached to diaphragm serous pericardium – secretes serous fluid parietal pericardium – lines inner fibrous pericardium visceral pericardium (epicardium) – lines heart pericardial cavity – space between parietal and visceral layers lubricated with pericardial fluid Internal Anatomy of Heart 3 layers of heart wall: epicardium – outermost; visceral pericardium mesothelium + areolar connective tissue myocardium – middle layer cardiac muscle + endomysium endocardium – innermost; thin, smooth layer endothelium + areolar connective tissue Chambers of the Heart – cavities within the heart 2 atria – thin-walled chambers at base of heart right atrium, left atrium auricles – extensions of atria 2 ventricles – thick-walled chambers forming apex of heart right ventricle, left ventricle 1 septa – walls separating the different heart chambers interatrial septum – between right and left atria interventricular septum – between right and left ventricles right side of heart is completely separated from left side of heart atrioventricular septum – between atria and ventricles atrioventricular (AV) valves – gates between atria and ventricles sulci – superficial grooves between heart chambers; contain adipose tissue and blood vessels supplying the heart coronary sulcus – between atria and ventricles anterior and posterior interventricular sulci – between right and left ventricles Right Heart (pulmonary circuit) – receives deoxygenated blood from tissues and pumps it to the lungs to be oxygenated Right atrium – receives deoxygenated blood from tissues cranial and caudal vena cava – large veins from body tissues coronary sinus – venous sinus from heart tissue right auricle – increases volume of right atrium right atrium contracts Right AV valve (tricuspid valve) – blood flows through from right atrium to right ventricle 3 cusps (flaps) – connected to tendon-like chordae tendineae in ventricle Right ventricle trabeculae – raised bundles of muscle fibers in inner wall papillary muscles – cone-shaped trabeculae which attach to chordae tendineae right ventricle contracts Pulmonary valve (semilunar valve) – blood flows through into pulmonary trunk right and left pulmonary arteries pulmonary capillaries pulmonary veins left heart (pulmonary arteries contain deoxygenated blood) Left Heart (systemic circuit) – receives oxygenated blood from lungs and pumps it to tissues throughout the body Left atrium – receives oxygenated blood from pulmonary circuit 4-6 pulmonary veins carry oxygenated blood returning from lungs left auricle – increases volume of left atrium left atrium contracts Left AV valve (mitral valve or bicuspid valve) – blood flows through from left atrium to left ventricle 2 cusps – chordae tendineae 2 Left ventricle thickest myocardial wall structure similar to right ventricle left ventricle contracts Aortic valve (semilunar valve) – blood flows through into ascending aorta aortic arch descending aorta arterial branches to all tissues systemic capillaries systemic veins right heart Fibrous Skeleton of the Heart dense fibrous connective tissue rings surround heart valves continuous with dense fibrous connective tissue in atrioventricular septum functions: supports valves origin for cardiac muscle electrical insulation between atria and ventricles os cordis – bone found in this region in cattle Function of Heart Valves one-way valves open and close due to pressure changes as heart contracts blood always flows from high pressure to low pressure AV valves (tricuspid and bicuspid) cusps connected to papillary muscles in ventricles (like parachutes) low ventricular pressure – when ventricles are relaxed blood flows through open valve into ventricles high ventricular pressure – when ventricles are contracting AV valves close blood pushes cusps toward atria papillary muscles and chordae tendineae prevent backflow Semilunar valves (aortic and pulmonary valves) 3 cusps - crescent moon-shaped (form convex-concave shape) high ventricular pressure – when ventricles are contracted semilunar valves open (blood pushes between convex cusps) blood flows into aorta and pulmonary trunk low ventricular pressure – when ventricles relax semilunar valves close blood in aorta and pulmonary trunk flows back towards ventricles filling concave cusps and pushing them closed valvular incompetence – valve doesn’t close completely regurgitation – blood leaks backwards valvular stenosis – narrowing of valve, doesn’t open fully 3 Cardiac Muscle Function branched fibers, one nucleus, many large mitochondria striated – thick and thin filaments overlap to form A & I bands sarcomeres contract when an action potential causes calcium ions to flow into cytoplasm from sarcoplasmic reticulum (SR) and through cell membrane intercalated discs – connect neighboring muscle cells gap junctions allow action potentials to conduct between cells syncytium – cardiac muscle cells contract as a functional unit Autorhythmicity – electrical stimulation comes from specialized cardiac muscle cells (NOT the nervous system) autorhythmic cells – 1% of cardiac muscle cells spontaneously depolarize (ions leak in) cells reach threshold at regular intervals voltage-gated Ca+2 channels cause depolarization pacemaker – sets rhythm for contractions (depolarizes fastest) conduction system – pathway for propagation of pacemaker signal ensures coordinated contractions Conduction Pathway 1) sinoatrial (SA) node – normal pacemaker in right atrial wall resting potential is not stable – spontaneously reaches threshold faster than any other autorhythmic cells threshold depolarization produces an action potential action potential propagates through both atrial walls via gap junctions 2) atrioventricular (AV) node – in atrial septum 3) atrioventricular (AV) bundle (bundle of His) only site for conduction from atria to ventricles (fibrous skeleton insulates other regions the of AV septum) 4) right and left bundle branches – in interventricular septum conduct impulse to apex of heart 5) Purkinje fibers – conduct impulse from apex upward throughout ventricular walls AV node can act as a pacemaker, but depolarizes more slowly other autorhythmic fibers fire even more slowly than AV node ectopic pacemaker – abnormal site depolarizes too rapidly electrolyte imbalances, hypoxia, toxin 4 Cardiac Muscle Action Potential 1) depolarization resting membrane potential is about -90mV autorhythmic fibers cause threshold depolarization voltage-gated sodium channels open sodium ions rush in – rapid depolarization sodium channels close 2) plateau – maintained depolarization voltage-gated calcium channels open – calcium ions flow in from SR and interstitial space 3) repolarization Ca channels close voltage-gated potassium channels open – potassium ions rush out and restore negative charge inside cell long refractory period – another action potential cannot occur until muscle relaxation has occurred (prevents tetanus) contraction is like skeletal muscle calcium ions bind to troponin actin and myosin filaments bind and slide past each other Electrocardiogram (ECG or EKG) – composite recording of action potentials generated by the heart measured on body surface by electrodes in specific locations (leads) normal sinus rhythm – generated by sinoatrial node P wave – atrial depolarization QRS complex – ventricular depolarization T wave – ventricular repolarization (atrial repolarization is masked by QRS) size of waves and intervals between them can indicate condition of the heart Cardiac Cycle – time between 1 heartbeat and the next systole – phase of contraction atrial systole – atria contract together (follows P wave) ventricular systole – ventricles contract together (follows QRS complex) diastole – phase of relaxation atrial diastole – atria relax (follows QRS) ventricular diastole – ventricles relax (follows T wave) 5 1 Cardiac Cycle: atrial systole – atria contract pressure increases in atria blood flows through open AV valves into relaxed ventricles end-diastolic volume – volume of filled ventricle ventricular systole – ventricles contract (simultaneous atrial diastole – atria relax) pressure increases in ventricles AV valves close isovolumetric contraction – pressure in ventricle increases but volume stays the same until pressure is greater than pressure in aorta or pulmonary trunk semilunar valves open ventricular ejection – ventricles continue to contract blood pumped into aorta/pulmonary trunk end-systolic volume – volume remaining in ventricle ventricular diastole – ventricles relax pressure decreases in ventricles and semilunar valves close isovolumetric relaxation – pressure in ventricle decreases but volume stays the same until pressure is less than atrial pressure AV valves open – ventricular filling begins Blood Pressure – pressure in systemic circulation (pulmonary pressure is lower) systolic pressure – due to maximum left ventricular contraction diastolic pressure – during ventricular relaxation, pressure maintained by smooth muscle in arteries Heart Sounds due to turbulence as blood flow patterns are altered 1st sound – closing of AV valves 2nd sound – closing of semilunar valves 3rd sound – opening of AV valves 4th sound – contraction of atria murmurs – abnormal sounds (valve disorders, septal defects) Circulation in the Fetal Heart 2 shunts – by-pass lungs (no oxygen in fetal lungs!) foramen ovale – hole between right and left atria shunts blood from right atrium to left atrium fossa ovalis – closes following birth ductus arteriosus – artery between pulmonary trunk and aorta shunts blood from pulmonary trunk to aorta ligamentum arteriosum – closes following birth 6 CARDIODYNAMICS stroke volume (SV) – ml of blood ejected by each ventricle/cardiac cycle SV = end-diastolic volume(EDV) – end-systolic volume(ESV) (eg. 130ml – 60ml = 70ml stroke volume) heart rate (HR) – heart beats/minute (eg. 75 bpm) Cardiac Output (CO) - volume of blood ejected by each ventricle/minute (equal for right and left ventricles) CO = stroke volume X heart rate (eg. 70ml/beat X 75 beats/min = 5.25 liters/minute) CO changes to meet body needs cardiac reserve – difference between maximum cardiac output and resting cardiac output normally 4-5 times resting CO Increasing Cardiac Output Increase stroke volume 3 factors affect SV: 1) preload – stretch (fullness) of ventricle before contraction >EDV = >preload = stronger contraction (Starling’s law) pericardial sac prevents overstretching heart muscle preload is affected by filling time and venous return 2) contractility – strength of contraction positive inotropic agents – increase contractility (most increase Ca entering cardiac muscle cells) sympathetic NS, epinephrine, digitalis, Ca ions negative inotropic agents – decrease contractility parasympathetic NS, calcium-channel blockers, beta-blockers (block sympathetic response) 3) afterload – pressure in aorta/pulmonary trunk resists ejection of blood from ventricles high blood pressure and atherosclerosis decrease SV Increase heart rate – up to a maximum heart rate (too high HR decreases filling time = decreases preload) Regulation of Heart Rate HR depends on: tissue demands – basal metabolic rate and activity level stroke volume – as SV decreases HR must increase 7 Autonomic Nervous System Regulation cardiovascular center – medulla oblongata inputs – emotions (fear, excitement, anxiety) sensory – proprioceptors – physical activity chemoreceptors – oxygen, carbon dioxide levels baroreceptors – blood pressure output – sympathetic (norepinephrine) cardiac accelerator nerves – beta receptors in SA and AV nodes – increases depolarization rates output – parasympathetic (acetylcholine) vagus nerves – SA and AV nodes decreases depolarization rates predominates at rest Chemical Regulation hormones adrenal medulla (sympathetic) – epinephrine, norepinephrine increases heart rate thyroid hormone – increases heart rate Other Factors Affecting Heart Rate body temperature high (hyperthermia) – faster HR low (hypothermia) – slower HR fitness – decreases HR electrolyte levels Na+ and K+ decrease HR Ca+2 increases HR arrhythmia – abnormal heart rhythm tachycardia – high resting heart rate bradycardia – low resting heart rate 8