* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Periplasmic adaptor protein AcrA has a distinct
Gene nomenclature wikipedia , lookup
Skewed X-inactivation wikipedia , lookup
Point mutation wikipedia , lookup
X-inactivation wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Public health genomics wikipedia , lookup
Pathogenomics wikipedia , lookup
Mir-92 microRNA precursor family wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
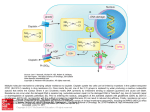
Journal of Antimicrobial Chemotherapy (2009) 64, 965– 972 doi:10.1093/jac/dkp311 Advance Access publication 10 September 2009 Periplasmic adaptor protein AcrA has a distinct role in the antibiotic resistance and virulence of Salmonella enterica serovar Typhimurium Jessica M. A. Blair1, Roberto M. La Ragione2, Martin J. Woodward2 and Laura J. V. Piddock1* 1 School of Immunity and Infection, College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK; 2Department of Food & Environmental Safety, Veterinary Laboratories Agency, Weybridge, Surrey, UK Received 24 June 2009; returned 21 July 2009; revised 3 August 2009; accepted 4 August 2009 Objectives: AcrA can function as the periplasmic adaptor protein (PAP) in several RND tripartite efflux pumps, of which AcrAB-TolC is considered the most important. This system confers innate multiple antibiotic resistance. Disruption of acrB or tolC impairs the ability of Salmonella Typhimurium to colonize and persist in the host. The aim of this study was to investigate the role of AcrA alone in multidrug resistance and pathogenicity. Methods: The acrA gene was inactivated in Salmonella Typhimurium SL1344 by insertion of the aph gene and this mutant complemented with pWKS30acrA. The antimicrobial susceptibility of the mutant to six antibiotics as well as various dyes and detergents was determined. In addition, efflux activity was quantified. The ability of the mutant to adhere to, and invade, tissue culture cells in vitro was measured. Results: Following disruption of acrA, RT–PCR and western blotting confirmed that acrB/AcrB was still expressed when acrA was disrupted. The acrA mutant was hypersusceptible to antibiotics, dyes and detergents. In some cases, lower MICs were seen than for the acrB or tolC mutants. Efflux of the fluorescent dye Hoechst H33342 was less than in wild-type following disruption of acrA. acrA was also required for adherence to, and invasion of, tissue culture cells. Conclusions: Inactivation of acrA conferred a phenotype distinct to that of acrB::aph and tolC::aph. These data indicate a role for AcrA distinct to that of other protein partners in both efflux of substrates and virulence. Keywords: AcrAB-TolC, efflux, pathogenicity Introduction Salmonella enterica is a Gram-negative bacterium capable of infecting a range of animals and causing a variety of diseases in humans and animals, including bacteraemia, enteric fever and enterocolitis, the most common manifestation. Enteric fever is caused by Salmonella Typhi and Salmonella Paratyphi, while nontyphoidal Salmonella serovars, such as Salmonella Enteritidis and Salmonella Typhimurium, are most commonly responsible for an enterocolitis with symptoms including headache, severe diarrhoea, abdominal pain and vomiting. Annually, there are 350000 reported cases in Europe1,2 and 200000 in the USA, although it has been suggested that the true number of cases is probably around three times higher as infection is usually self-limiting, does not require treatment and therefore goes unreported.3,4 Resistance to antibiotics is a growing clinical concern, with an increasing number of multiply resistant strains being isolated.5 Active efflux, where antimicrobial compounds are pumped out of the cell through membrane-spanning efflux pumps such as AcrAB-TolC, has been shown to be a clinically relevant mechanism of resistance to multiple antibiotics.6 – 8 Efflux can be responsible for resistance to multiple, structurally distinct, antibiotics and also for the innate resistance of some bacteria to whole classes of antibiotics.9,10 Overexpression of these pumps has been detected in human and animal clinical isolates of Salmonella Typhimurium, where it has been associated with multiple drug resistance (MDR).6 – 8,11,12 In clinical isolates shown to overexpress AcrB, the MICs of nalidixic acid, tetracycline and chloramphenicol were above the concentrations used to define resistance according to the BSAC.13 In addition, ..................................................................................................................................................................................................................................................................................................................................................................................................................................... *Corresponding author. Tel: þ44-121-414-6966; Fax: þ44-121-414-6819; E-mail: [email protected] ..................................................................................................................................................................................................................................................................................................................................................................................................................................... 965 # The Author 2009. Published by Oxford University Press on behalf of the British Society for Antimicrobial Chemotherapy. All rights reserved. For Permissions, please e-mail: [email protected] Blair et al. inactivation of acrB led to increased susceptibility to a range of antibiotics, dyes and detergents, including the quinolones, tetracycline, chloramphenicol, bile salts, SDS, ethidium bromide and triclosan.8,12,14 AcrAB-TolC is a tripartite efflux pump found in Enterobacteriaceae and is a member of the resistance nodulation division (RND) family of efflux pumps. It has a broad substrate range, including various antibiotics, dyes and detergents.12,15 The three components are AcrB, the inner membrane transporter protein, AcrA, the periplasmic adaptor protein (PAP), and TolC, the outer membrane channel. AcrA from Escherichia coli is an elongated sickle-shaped protein,16 which has been shown to interact with both AcrB and TolC17 – 20 as well as being bound to the inner membrane by an N-terminal lipid moiety.21 Suggested roles for AcrA include assembly and maintenance of a stable complex in vivo,19,22 and transmitting conformational changes in AcrB to TolC, facilitating the opening of the outer membrane channel.16 Although the components of the AcrAB-TolC pump function together as a tripartite pump, the individual components can also function in conjunction with other efflux systems. For example, TolC, in E. coli, has been shown to be required for the function of many efflux systems, including the RND pumps AcrD,23,24 AcrEF,24 MdsAB25 and MdtABC,26 as well as for the MFS systems EmrAB and EmrKY,27 and also the ABC drug transporter MacAB.28 Similarly, AcrA has been shown to associate with AcrD29,30 and AcrF,30,31 as well as with AcrB and TolC. In contrast, AcrB is not known to cooperate with other efflux pump components, but in E. coli it has been shown recently to have a role in contact-dependent growth inhibition (CDI), possibly as a downstream target for the CDI signal, which is independent of both AcrA and TolC.32 The amino acid sequence of AcrAB-TolC of E. coli is very similar to that of Salmonella, with 94%, 97% and 94% similarity for AcrA, AcrB and TolC, respectively, so it is thought that they are also functionally similar.9 In addition to an established role in antimicrobial resistance, MDR efflux pumps, including AcrAB-TolC, have been shown to have a role in pathogenicity in a variety of organisms.14,25,33 – 38 In Salmonella Typhimurium, disruption of either acrB or tolC led not only to hypersusceptibility to a range of antimicrobial compounds, but also to a significantly reduced ability to adhere to, or invade, human intestinal epithelial cells (INT-407) or mouse macrophages (RAW 264.7) in vitro. Inactivation of either acrB or tolC also led to reduced colonization and persistence in poultry14 and reduced virulence in the mouse model of invasive Salmonella infection.25 The effect seen in vivo can be partially explained by the finding that many MDR efflux pumps, or certain components thereof, are also responsible for exporting host-derived substrates, such as bile salts and fatty acids. Deletion of acrAB in E. coli led to increased susceptibility to bile salts and decanoate (a fatty acid), and the expression of these genes was elevated in the presence of decanoate.39 These data support the hypothesis that AcrAB-TolC exports these compounds and therefore has a physiological role in enabling these enteric bacteria to survive within the hostile environment of the host.40 However, this does not explain the effect seen in vitro in tissue culture. In previous work, only the transporter (e.g. AcrB), the outer membrane protein (e.g. TolC) or AcrA with AcrB have been investigated for their contribution to innate MDR and pathogenicity. However, we wished to investigate the contribution of the PAP, AcrA, along with the hypothesis that AcrA has a role in the MDR and pathogenicity of S. enterica serovar Typhimurium. Materials and methods Bacterial strains and construction of mutants S. enterica serovar Typhimurium strain SL1344 was used throughout this study.41 Strains L109 (tolC::aph) and L110 (acrB::aph) were constructed during a previous study and are the P22 transductants of L108 and L643, respectively.14 The acrA gene was inactivated in Salmonella Typhimurium SL1344 by insertion of the aph gene between nucleotides 99 and 1088 as described previously,12,42 using the primers shown in Table 1. Sequences were taken from xbase (http://xbase.bham.ac.uk/colibase/) and primers designed using PRIMER v.2.00 software (Scientific and Educational Software, UK) and produced by Invitrogen (Invitrogen Ltd, UK). PCR and sequencing was used to confirm that the aph gene had inserted in the correct position. The acrA::aph construct was transduced into SL1344 using P22 phage, with selection for kanamycin resistance. Putative transductants were selected on LB agar containing kanamycin, and allelic replacement was confirmed by PCR and sequencing. The aph gene was removed using the pCP20 plasmid, encoding the FLP recombinase gene.42 Removal was confirmed by the loss of kanamycin resistance, followed by PCR and sequencing. The acrA mutant (L884) was complemented by cloning wild-type acrA, along with the native promoter, into the low copy number vector pWKS3043 after digestion of both the plasmid and insert with BamHI and HindIII. The resulting plasmid ( pWKS30acrA) was sequenced to confirm insert identity. The growth kinetics of parent and mutant strains was determined using a FLUOstar OPTIMA (BMG Labtech, Aylesbury, UK). Overnight cultures were diluted 1:100 in LB broth and grown at 378C with shaking at 150 rpm. The optical density (at 600 nm) was measured every 10 min for 24 h. RT – PCR Bacterial strains were grown in minimal medium (Teknova, USA) at 378C with aeration until mid-logarithmic phase. A 95% ethanol/5% phenol mixture was added and incubated on ice for 30 min. After centrifugation, the supernatant was discarded and the pellets resuspended in TE buffer with 50 mg/L lysozyme and incubated at room temperature for 5 min. RNA was then isolated using the Promega SV Total RNA Purification Kit (Promega Corporation, UK, Z3100), according to the manufacturer’s instructions. Residual DNA was removed by digestion with Promega RNase-free DNase (Promega Corporation, UK, M6101), according to the manufacturer’s instructions. cDNA was synthesized using Invitrogen Superscript II Reverse Transcriptase (Invitrogen, UK). PCRs for acrA, acrB and 16s RNA were set up using the cDNA as a template and the internal primers shown in Table 1. For the 16s RNA PCR, cDNA was used at a 1:1000 dilution, while for both acrA and acrB PCRs the cDNA was used at a dilution of 1:5.12 The PCR amplimers were quantified using dHPLC, as described previously.12 Western blotting Bacterial strains were grown in LB broth (Sigma) at 378C with aeration until mid-logarithmic phase. Total cellular protein was obtained following sonication and samples were run on 12% Bis-Tris gels (Invitrogen) along with the Magic MarkTM XP molecular weight 966 Role of AcrA in Salmonella Table 1. Primer sequences Description acrA knockout primer forward acrA knockout primer reverse Upstream acrA Downstream acrA Internal acrA forward Internal acrA reverse Internal 16s forward Internal 16s reverse Internal acrB forward Internal acrB reverse Internal aph forward Internal aph reverse acrA complementation forward acrA complementation reverse a Primer sequence AGC GCT AAC AGG ATG TGA CGA CAA ACA GGA CCA GCA AGG CGT GTA GGC TGG AGC TGC TTCa CTG TAC TTT AAC CTG TGC GCC AGG ACG TAC TTT TTG CAG CGG GAA TTA GCC ATG GTC CATa ACA TCC AGG ATG TGT TGT CG CAA TCG TCG GAT ATT GCG CT GCA GTA CAT CAG TAA GCA GG CCT TGC GTT ACG GAT GAC TT CCT CAG CAC ATT GAC GTT AC TTC CTC CAG ATC TCT ACG CA CGT GTT ATG ACG GAA GAA GG GCC ATA CCG ACG ACG ATA AT CGG TGC CCT GAA TGA ACT GC CGG CCA CAG TCG ATG AAT CC TCA AGC TTA CAT CCA GGA TGT GTT GTC G TCG GAT CCA TCG TCG GAT ATT GCG CTA C Underlined sequences correspond to the 20 bp homology to the aph gene encoding kanamycin resistance. marker (Invitrogen). For subsequent immunoblotting, proteins were transferred to a PVDF membrane (Amersham) by electrophoresis for 3 h at 48C. The membrane was blocked with 5% non-fat milk solution. After overnight incubation with either AcrA or AcrB primary antibody [kindly provided by Helen Zgurskaya and Elena Tikhonova (University of Oklahoma) and Eva and Vassilis Koronakis (University of Cambridge), respectively], the proteins were visualized using an HRP-linked anti-rabbit secondary antibody raised in donkey (GE Healthcare) and an ECL western blotting detection system (GE Healthcare). Determination of the antimicrobial susceptibility to antibiotics, dyes and detergents The MICs of a range of antibiotics, dyes and detergents were determined using the standardized agar doubling dilution method as described by the BSAC.13 Each value is the modal value from at least three independent experiments and the inherent error of the doubling dilution method is + one dilution.13 (Sigma). To measure association of bacterial cells with either INT-407 or RAW 264.7 cells, the washed monolayers were inoculated with 5107 cfu bacteria and incubated for 2 h at 378C in 5% CO2. The infected monolayers were then washed six times with HBSS and disrupted by adding 1% Triton X-100 and stirring with a magnetic flea for 10 min. The number of cfu/mL was determined by serial dilution onto LB agar and incubation for 16 h. Invasion assays were performed in parallel with the association assays. After the initial 2 h incubation as described, the infected monolayers were washed six times with HBSS before addition of either MEM or DMEM containing 100 mg/L gentamicin to kill all external bacteria. Plates were incubated for a further 2 h and monolayers disrupted by adding 1% Triton and stirring with a magnetic flea for 10 min, and the cfu/mL determined by serial dilution onto LB agar. Adhesion was calculated as the number of bacteria associated with the eukaryotic cells minus the number that had invaded. Each assay was repeated a minimum of three times, with each repeat including four technical replicates per bacterial strain. The results were analysed using Student’s t-test and P values of 0.05 were taken as significant. Adhesion and invasion assays The ability of the strains to adhere to, and invade, INT-407 (human embryonic intestine cells) and RAW 264.7 (mouse macrophages) was determined as previously described.14,44 Briefly, INT-407 cells were maintained in minimal essential medium (MEM), while RAW 264.7 cells required Dulbecco’s modified Eagle’s medium (DMEM), both supplemented with 10% heat-inactivated fetal calf serum (Invitrogen), 1% non-essential amino acids (NEAAs) (Sigma), 1% glutamine (Sigma) and 50 mg/L gentamicin (Sigma). Plates (24-well) were seeded with either INT-407 or RAW 264.7 cells and incubated for 48 h at 378C and 5% CO2 until confluent. Confluent monolayers contained 4–6105 cells per well. Prior to the assays, the monolayers were washed three times in Hanks’ balanced salt solution (HBSS) (Sigma). For tissue culture assays, bacterial cultures were grown overnight in LB broth at 378C, with agitation and washed in PBS before being diluted in MEM or DMEM supplemented with 1% NEAAs (Sigma) and 1% glutamine Accumulation of Hoeschst H33342 (bis-benzamide) Hoechst H33342 (bis-benzamide) fluoresces when bound to DNA and therefore its accumulation can be used to assess the relative level of active efflux in the mutants.45,46 Bacteria were grown overnight in LB broth, pelleted and resuspended in PBS to an OD600 of 0.1. Hoechst H33342 was added to a final concentration of 2.5 mM. Fluorescence intensity was measured over 30 min at excitation and emission wavelengths of 350 and 461 nm, respectively, in a FLUOstar OPTIMA (BMG Labtech). The experiments were performed in duplicate on three separate occasions (i.e. three biological replicates each with two technical replicates). Student’s t-tests of the mean values accumulated after 50 min were performed to compare the accumulation of Hoescht H33342 by each strain with that of the parental wild-type strain, SL1344; P values of ,0.05 were taken to be significant. 967 Blair et al. Table 2. Salmonella Typhimurium strains used in this study Strain SL1344 L109a L110a L823 L884 L976 L979 Mean generation time (min)+SD P value Reference 32.0+2.65 28.5+1.29 28.6+0.57 — 0.07 0.09 30.5+1.22 0.26 41 14 12 this study this study this study this study tolC::aph acrB::aph acrA::aph acrA::aph transduced in SL1344 DacrA acrA::aph, pWKS30acrA L109 and L110 are the P22 transductants of L108 and L643, respectively.14 L979 (acrA::aph, pWKS30acrA) Results Inactivation of acrA alone leads to hypersusceptibility to a range of antibiotics, dyes and detergents, and reduced efflux Salmonella Typhimurium SL1344 was susceptible to all 13 agents tested (Table 3). The acrA mutants L884 (acrA::aph) and L979 (acrA::aph, pWKS30acrA) showed the expected increase in kanamycin resistance to .256 mg/L due to the incorporation of the aph gene and increased susceptibility to almost all other agents. MIC values for the acrB and tolC mutants were all within one dilution of previously published data from this laboratory.12,14 The susceptibility profile of the acrA mutant (L884) L884 (acrA::aph) L976 (ΔacrA) L110 (acrB::aph) (b) AcrB L109 (tolC::aph) (a) AcrA SL1344 (WT) The acrA gene was inactivated by insertion of the aph gene conferring kanamycin resistance. The inserted sequence also includes a ribosomal binding site and an inframe start codon to allow expression of downstream acrB. The mutant was designated L823 (Table 2). The disrupted region was transduced into the wild-type SL1344 background using P22 phage to eliminate non-specific mutations caused by the l red recombinase used in the creation of the mutant. The transduced strain was designated L884 (Table 2). The aph gene was removed using the pCP20 plasmid as previously described42 to ensure there were no polar effects from the insertion and this kanamycin susceptible mutant was named L976 (Table 2). All constructs were verified by PCR and sequencing. Mutants containing acrA::aph or DacrA were complemented with wild-type acrA cloned into the low copy number vector pWKS30 (Table 2).43 There was no significant difference between the generation times or the optical density at which stationary phase occurred in minimal medium for SL1344 or any of the constructs (Table 2). RT –PCR was performed to confirm that acrB was transcribed in L884 (acrA::aph). This was necessary because acrA and acrB are found in a single operon, so to determine the role of AcrA alone it is crucial that transcription of acrB is not affected by the disruption of the acrA region. RT – PCR showed that acrA was expressed by SL1344 and L979 (acrA::aph, pWKS30acrA), but was not expressed by L884 (acrA::aph). The acrB gene was expressed by all strains tested. Western blotting with anti-AcrB antibody confirmed the expression of the AcrB protein in all three strains, while blotting with anti-AcrA antibody confirmed that AcrA expression had been abolished in the acrA mutants (Figure 1). SL1344 Construction of a mutant with inactivation of acrA alone L884 (acrA::aph) a Genotype Figure 1. Western Blotting for AcrA and AcrB. (a) AcrA expression was eliminated after disruption of acrA in L884 (acrA::aph) or L976 (DacrA), but expression was detected in the complemented strain L979 (acrA::aph, pWKS30acrA). (b) AcrB expression was eliminated by disruption of acrB (L110), but expression was not affected by disruption of either acrA (L884) or tolC (L109). was distinct from that of the acrB (L110) and tolC (L109) inactivated strains (Table 3). While L884 (acrA::aph) was as susceptible (+1 dilution) as L110 (acrB::aph) to ampicillin, nalidixic acid, chloramphenicol, tetracycline, ethidium bromide, bile, SDS and Triton, it was more susceptible than the acrB mutant to triclosan, acriflavine and fusidic acid. The acrA mutant (L884) was as susceptible as the tolC mutant (+1 dilution) to ampicillin, nalidixic acid, chloramphenicol, tetracycline, acriflavine and fusidic acid, while L109 (tolC::aph) was more susceptible to ethidium bromide, bile, SDS and Triton. The acrA mutant was more susceptible than the tolC mutant to ciprofloxacin and triclosan. Complementation of both acrA::aph and DacrA restored antibiotic susceptibility to that of the parental strain, SL1344 (Table 3). In order to compare the levels of active efflux in the acrA mutant, accumulation of Hoechst H33342 was determined and compared with that in SL1344 and the acrB and tolC mutants. Accumulation of Hoechst H33342 was 2-fold higher following inactivation of acrA compared with the wild-type strain SL1344 968 Role of AcrA in Salmonella Table 3. MICs of antibiotics, dyes and detergents MIC (mg/L) Strain Genotype SL1344 L823 L884 L976 L979 L110 L109 KAN AMP 8 1 acrA::aph .256 0.25 acrA::aph .256 0.25 DacrA 8 0.25 acrA::aph, pWKS30acrA .256 .128 acrB::aph .256 0.25 tolC::aph .256 0.25 NAL CIP 4 0.5 0.5 0.5 4 1 1 0.015 0.002 0.002 0.002 0.015 0.015 0.015 CHL TET TRIC EtBr ACR FUS 4 0.5 0.5 0.5 4 1 1 1 0.5 0.5 0.5 1 1 0.5 bile SDS Triton X-100 0.06 .256 256 .512 .1024 .512 0.008 64 16 4 2048 256 0.008 64 16 4 2048 256 0.008 64 16 4 2048 256 0.06 .256 256 512 .1024 512 0.03 64 64 16 1024 128 0.015 16 16 4 256 64 .20000 .20000 .20000 .20000 .20000 .20000 1200 (a) 3500 Inactivation of acrA alone attenuates virulence in vitro Arbitrary fluorescence units KAN, kanamycin; AMP, ampicillin; NAL, nalidixic acid; CIP, ciprofloxacin; CHL, chloramphenicol; TET, tetracycline; TRIC, triclosan; EtBr, ethidium bromide; ACR, acriflavine; FUS, fusidic acid. Bold formatting indicates significantly increased susceptibility (MIC changed 2-fold). Triton X-100 was used in all the tissue culture assays to disrupt the eukaryotic cell monolayer, allowing the number of bacteria to be determined. It has been shown previously that this concentration of the detergent does not affect viability of either the acrB or tolC mutants (L110 and L109, respectively) during the timespan of the assay.14 Susceptibility to Triton X-100 was not affected by inactivation of acrA or acrB (Table 3). To ensure that Triton X-100 was not affecting the viability of the acrA mutant during the tissue culture assays, bacterial recovery after exposure to Triton X-100 and water were compared. As shown previously for the other strains,14 there was no significant difference in the viable count over the time period studied (data not shown). In addition, growth kinetics of the bacterial strains in the continuous presence of 1% Triton X-100 and with 1% Triton X-100 added after 2 h (logarithmic growth phase) were measured. There was no significant difference between the generation times of the wild-type parental strain, SL1344, and the mutants when in the continuous presence of 1% Triton X-100 or with Triton X-100 added during logarithmic growth phase (data not shown). The ability of Salmonella Typhimurium L884 (acrA::aph) and L979 (acrA::aph, pWKS30acrA) to adhere to, and invade, human embryonic intestine cells (INT-407) in vitro was determined and compared with that of SL1344, L109 (tolC::aph) and L110 (acrB::aph) (Figure 3). As previously published,14 the ability of L109 (tolC::aph) to adhere to INT-407 cells was significantly decreased compared with SL1344 (P ¼ 0.0002), while L110 (acrB::aph) and L884 (acrA::aph) were unaffected (P ¼ 0.07 and 0.34, respectively). All the mutants, L109 (tolC::aph), L110 (acrB::aph) and L884 (acrA::aph), had a significantly reduced ability to invade the INT-407 cell line compared with the parental strain, SL1344 (0.003%, 1.00% and 5.77% of wild-type invasion, respectively; P values ranging from 0.00019 to 0.00021). When the acrA mutation was complemented with pWKS30acrA, the mutant phenotype was abolished (Figure 3). A similar pattern was seen with a mouse macrophage cell line (RAW 264.7); however, in this case the ability of all mutants to adhere to, and invade, the eukaryotic cells was significantly impaired and L109 (tolC::aph) completely lost the ability to invade (data not shown). 3000 2500 2000 1500 1000 SL1344 500 L884 (acrA::aph) 0 20 0 40 0 60 0 80 0 10 00 12 00 14 00 16 0 18 0 00 20 00 22 00 24 00 26 00 28 00 30 00 0 Time (s) Fold change (b) * 5 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 * * SL1344 L884 L979 (L884 + L110 L109 (acrA::aph) pWKS30acrA) (acrB::aph) (tolC::aph) Figure 2. Hoechst H33342 efflux. (a) The accumulation of Hoechst H33342 in L884 (acrA::aph) and SL1344 over time. (b) The mean fold change in accumulation of Hoechst H33342 after 50 min in SL1344, the acrA mutant (L884), the acrA-complemented strain (L979), the acrB mutant (L110) and the tolC mutant (L109). Student’s t-tests were performed to compare the accumulation of each strain with that of the wild-type, SL1344, returning P values of 0.04, 0.21, 0.005 and 0.003, respectively. P values of ,0.05 are indicated by asterisks. (P ¼ 0.04), indicating a lower level of efflux. This phenotype was abolished in the complemented strain (L979). The acrB mutant accumulated 2.9-fold more Hoechst H33342 (P ¼ 0.005), while the tolC mutant accumulated 3.6-fold more (P ¼ 0.003) (Figure 2). 969 Blair et al. 1.0E + 07 * 1.0E + 06 * cfu/mL 1.0E + 05 * 1.0E + 04 1.0E + 03 * 1.0E + 02 1.0E + 01 SL1344 L884 L979 L110 L109 (acrA::aph) (L884 + (acrB::aph) (tolC::aph) pWKS30acrA) Adhesion Invasion Figure 3. Ability of Salmonella Typhimurium SL1344 and mutants thereof to adhere to, and invade, human intestinal cells (INT-407). Adhesion of the acrA::aph mutant strain to the INT cell line was not significantly different from the parental strain. However, the mutant had a significantly reduced ability to invade. This phenotype was abolished when the acrA mutation was complemented with pWKS30acrA. P values of ,0.05 are indicated by asterisks. Discussion Inactivation of acrA, as found previously with mutants lacking AcrB or TolC, led to increased susceptibility to a range of antibiotics, dyes and detergents compared with the parental strain Salmonella Typhimurium SL1344; however, subtle differences were seen in phenotype, dependent upon which gene (acrA, acrB or tolC) was inactivated. The susceptibility of L884 (acrA::aph) to antimicrobials, although distinct, was generally similar to, and in some cases greater than, that of L110 (acrB::aph), which suggests an important role for the periplasmic adaptor protein, AcrA, in efficient efflux. These data can be partially explained by the reported promiscuity of the AcrA protein with other efflux proteins of the RND family of efflux pumps, including AcrD and AcrF.29 – 31 The greatest increase in susceptibility was seen with the inactivation of tolC, particularly to fusidic acid, nalidixic acid and Triton X-100, as previously reported for both Salmonella and E. coli.14,24,25 TolC also acts as the outer membrane component for many efflux systems, including other RND pumps,23 – 26 as well members of the MFS27 and ABC drug transporter families;28 therefore, disruption of TolC will not only affect the ability of the AcrAB pump to function, but will interfere with other export pathways. Interestingly, the acrA mutant was more susceptible to ciprofloxacin and triclosan than the tolC mutant. This may be because the AcrA protein is also promiscuous and may associate with efflux pumps of other families, which can also transport ciprofloxacin and triclosan. Accumulation of the fluorescent dye Hoechst H33342 was increased 2-fold in the acrA mutant (L884 acrA::aph), showing a significant decrease in efflux. These data suggest that the PAP is an integral component of the efflux process and that without it efficient function is diminished. This supports the hypothesis that the PAP has an active role in the pump function.47 The observed decrease in efflux goes some way to explain the increase in susceptibility of strains lacking AcrAB-TolC to the antimicrobials tested. The decreased efflux means that toxic compounds are not extruded as efficiently and, therefore, accumulate inside the cell and are lethal at a lower total concentration. However, the effect is substrate-specific, as the acrA mutant is the most susceptible to triclosan while it does not have the most attenuated efflux. As previously published,14 inactivation of either acrB or tolC led to a reduced ability to invade INT-407 cells compared with the parental strain and inactivation of tolC also affected adherence. In addition, we have now shown that inactivation of acrA also affects the ability to invade host cells. The involvement of RND efflux pump proteins, including AcrB and TolC and homologues thereof in other bacteria, in pathogenicity is now well established.14,25,33 – 38,40,48 This study extends these findings from this, and from other laboratories, to include the role of the periplasmic adaptor protein, AcrA, in this process. Loss of functional acrA significantly affected the efflux activity, antibiotic susceptibility and also the virulence of the mutant. This suggests a key role for AcrA in the efficient operation of this pump, which is separate and distinct from that of AcrB (or other protein partners) or TolC. This is complementary to the growing body of structural data showing that AcrA physically interacts with both AcrB and TolC,17,18,49 and that the conformational flexibility seen in E. coli AcrA could mediate the opening of the TolC channel.16,50 The extent of the change in phenotype is probably augmented by the promiscuity of AcrA, such that disruption of acrA will also cause the function of other RND pumps to be impaired.23,24,29 – 31 Acknowledgements We are grateful to Helen Zgurskaya and Elena Tikhonova for their gifts of the anti-AcrA antibodies and technical advice with regard to western blotting. We are grateful to Eva and Vassilis Koronakis for the gift of anti-AcrB antibodies. We thank Sarah Coleman for her technical assistance. Funding The study was funded by the Medical Research Council doctoral training account to the University of Birmingham Medical School for J. M. A. B. Transparency declarations None to declare. References 1. Fisher I. Dramatic shift in the epidemiology of Salmonella enterica serotype Enteritidis phage types in western Europe, 1998– 2003—results from the Enter-net international salmonella database. Euro Surveill 2004; 9: pii¼486. 2. Fisher IS. International trends in salmonella serotypes 1998– 2003—a surveillance report from the Enter-net international surveillance network. Euro Surveill 2004; 9: pii¼487. 970 Role of AcrA in Salmonella 3. Mead PS, Slutsker L, Dietz V et al. Food-related illness and death in the United States. Emerg Infect Dis 1999; 5: 607– 25. 4. Rhen M, Maskell D, Mastroeni P et al., eds. Salmonella: Molecular Biology and Pathogenesis. Norfolk: Horizon Bioscience, 2007. 5. Meakins S, Fisher IST, Berghold C et al. Antimicrobial drug resistance in human nontyphoidal Salmonella isolates in Europe 2000–2004: a report from the Enter-net International Surveillance Network. Microb Drug Resist 2008; 14: 31 –5. 6. Piddock LJV, White DG, Gensberg K et al. Evidence for an efflux pump mediating multiple antibiotic resistance in Salmonella enterica serovar Typhimurium. Antimicrob Agents Chemother 2000; 44: 3118–21. 7. Giraud E, Cloeckaert A, Kerboeuf D et al. Evidence for active efflux as the primary mechanism of resistance to ciprofloxacin in Salmonella enterica serovar Typhimurium. Antimicrob Agents Chemother 2000; 44: 1223– 8. 8. Baucheron S, Tyler S, Boyd D et al. AcrAB-TolC directs effluxmediated multidrug resistance in Salmonella enterica serovar Typhimurium DT104. Antimicrob Agents Chemother 2004; 48: 3729–35. 9. Piddock LJV. Clinically relevant chromosomally encoded multidrug resistance efflux pumps in bacteria. Clin Microbiol Rev 2006; 19: 382–402. 10. Li XZ, Nikaido H. Efflux-mediated drug resistance in bacteria. Drugs 2004; 64: 159–204. 11. Baucheron S, Imberechts H, Chaslus-Dancla E et al. The AcrB multidrug transporter plays a major role in high-level fluoroquinolone resistance in Salmonella enterica serovar Typhimurium phage type DT204. Microb Drug Resist 2002; 8: 281– 9. 12. Eaves DJ, Ricci V, Piddock LJV. Expression of acrB, acrF, acrD, marA, and soxS in Salmonella enterica serovar Typhimurium: role in multiple antibiotic resistance. Antimicrob Agents Chemother 2004; 48: 1145–50. 13. Andrews J. Determination of minimum inhibitory concentrations. British Society for Antimicrobial Chemotherapy, 2006. http://www. bsac.org.uk/_db/_documents/Chapter_2_Determination_of_MICs_2006. pdf (20 August 2009, date last accessed). 14. Buckley AM, Webber MA, Cooles S et al. The AcrAB-TolC efflux system of Salmonella enterica serovar Typhimurium plays a role in pathogenesis. Cell Microbiol 2006; 8: 847–56. 15. Yu EW, Aires JR, Nikaido H. AcrB multidrug efflux pump of Escherichia coli: composite substrate-binding cavity of exceptional flexibility generates its extremely wide substrate specificity. J Bacteriol 2003; 185: 5657–64. 16. Mikolosko J, Bobyk K, Zgurskaya HI et al. Conformational flexibility in the multidrug efflux system protein AcrA. Structure 2006; 14: 577–87. 17. Tikhonova EB, Zgurskaya HI. AcrA, AcrB, and TolC of Escherichia coli form a stable intermembrane multidrug efflux complex. J Biol Chem 2004; 279: 32116– 24. 18. Husain F, Humbard M, Misra R. Interaction between the TolC and AcrA proteins of a multidrug efflux system of Escherichia coli. J Bacteriol 2004; 186: 8533–6. 19. Touze T, Eswaran J, Bokma E et al. Interactions underlying assembly of the Escherichia coli AcrAB-TolC multidrug efflux system. Mol Microbiol 2004; 53: 697– 706. 20. Zgurskaya HI, Nikaido H. Cross-linked complex between oligomeric periplasmic lipoprotein AcrA and the inner-membrane-associated multidrug efflux pump AcrB from Escherichia coli. J Bacteriol 2000; 182: 4264–7. 21. Ma D, Cook DN, Alberti M et al. Molecular cloning and characterization of acrA and acrE genes of Escherichia coli. J Bacteriol 1993; 175: 6299–313. 22. Lobedanz S, Bokma E, Symmons M et al. A periplasmic coiledcoil interface underlying TolC recruitment and the assembly of bacterial drug efflux pumps. Proc Natl Acad Sci USA 2007; 104: 4612–7. 23. Hirakawa H, Nishino K, Hirata T et al. Comprehensive studies of drug resistance mediated by overexpression of response regulators of two-component signal transduction systems in Escherichia coli. J Bacteriol 2003; 185: 1851–6. 24. Nishino K, Yamada J, Hirakawa H et al. Roles of TolC-dependent multidrug transporters of Escherichia coli in resistance to b-lactams. Antimicrob Agents Chemother 2003; 47: 3030–3. 25. Nishino K, Latifi T, Groisman EA. Virulence and drug resistance roles of multidrug efflux systems of Salmonella enterica serovar Typhimurium. Mol Microbiol 2006; 59: 126–41. 26. Nagakubo S, Nishino K, Hirata T et al. The putative response regulator BaeR stimulates multidrug resistance of Escherichia coli via a novel multidrug exporter system, MdtABC. J Bacteriol 2002; 184: 4161–7. 27. Nishino K, Yamaguchi A. EvgA of the two-component signal transduction system modulates production of the YhiUV multidrug transporter in Escherichia coli. J Bacteriol 2002; 184: 2319–23. 28. Kobayashi N, Nishino K, Yamaguchi A. Novel macrolide-specific ABC-type efflux transporter in Escherichia coli. J Bacteriol 2001; 183: 5639–44. 29. Elkins CA, Nikaido H. Substrate specificity of the RND-type multidrug efflux pumps AcrB and AcrD of Escherichia coli is determined predominately by two large periplasmic loops. J Bacteriol 2002; 184: 6490–8. 30. Elkins CA, Nikaido H. Chimeric analysis of AcrA function reveals the importance of its C-terminal domain in its interaction with the AcrB multidrug efflux pump. J Bacteriol 2003; 185: 5349–56. 31. Kobayashi K, Tsukagoshi N, Aono R. Suppression of hypersensitivity of Escherichia coli acrB mutant to organic solvents by integrational activation of the acrEF operon with the IS1 or IS2 element. J Bacteriol 2001; 183: 2646–53. 32. Aoki SK, Malinverni JC, Jacoby K et al. Contact-dependent growth inhibition requires the essential outer membrane protein BamA (YaeT) as the receptor and the inner membrane transport protein AcrB. Mol Microbiol 2008; 70: 323–40. 33. Burse A, Weingart H, Ullrich MS. The phytoalexin-inducible multidrug efflux pump AcrAB contributes to virulence in the fire blight pathogen, Erwinia amylovora. Mol Plant Microbe Interact 2004; 17: 43–54. 34. Hirakata Y, Srikumar R, Poole K et al. Multidrug efflux systems play an important role in the invasiveness of Pseudomonas aeruginosa. J Exp Med 2002; 196: 109–18. 35. Jerse AE, Sharma ND, Simms AN et al. A gonococcal efflux pump system enhances bacterial survival in a female mouse model of genital tract infection. Infect Immun 2003; 71: 5576–82. 36. Lin J, Sahin O, Michel LO et al. Critical role of multidrug efflux pump CmeABC in bile resistance and in vivo colonization of Campylobacter jejuni. Infect Immun 2003; 71: 4250–9. 37. Piddock LJV. Multidrug-resistance efflux pumps—not just for resistance. Nat Rev Microbiol 2006; 4: 629–36. 38. Stone BJ, Miller VL. Salmonella enteritidis has a homologue of tolC that is required for virulence in BALB/c mice. Mol Microbiol 1995; 17: 701–12. 39. Ma D, Cook DN, Alberti M et al. Genes acrA and acrB encode a stress-induced efflux system of Escherichia coli. Mol Microbiol 1995; 16: 45–55. 40. Yamanaka H, Kobayashi H, Takahashi E et al. MacAB is involved in the secretion of Escherichia coli heat-stable enterotoxin II. J Bacteriol 2008; 190: 7693–8. 41. Wray C, Sojka WJ. Experimental Salmonella typhimurium infection in calves. Res Vet Sci 1978; 25: 139–43. 42. Datsenko KA, Wanner BL. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc Natl Acad Sci USA 2000; 97: 6640–5. 971 Blair et al. 43. Wang RF, Kushner SR. Construction of versatile low-copynumber vectors for cloning, sequencing and gene expression in Escherichia coli. Gene 1991; 100: 195 –9. 44. Dibb-Fuller MP, Allen-Vercoe E, Thorns CJ et al. Fimbriae- and flagella-mediated association with and invasion of cultured epithelial cells by Salmonella enteritidis. Microbiology 1999; 145: 1023–31. 45. Webber MA, Randall LP, Cooles S et al. Triclosan resistance in Salmonella enterica serovar Typhimurium. J Antimicrob Chemother 2008; 62: 83–91. 46. Webber MA, Coldham NC. Measuring Active Efflux in Gram-Negative Bacteria Using Hoescht 33342 (Bis-Benzamide). London: Humana Press, in press. 47. Aires JR, Nikaido H. Aminoglycosides are captured from both periplasm and cytoplasm by the AcrD multidrug efflux transporter of Escherichia coli. J Bacteriol 2005; 187: 1923–9. 48. Warner DM, Shafer WM, Jerse AE. Clinically relevant mutations that cause derepression of the Neisseria gonorrhoeae MtrC-MtrD-MtrE efflux pump system confer different levels of antimicrobial resistance and in vivo fitness. Mol Microbiol 2008; 70: 462–78. 49. Bavro VN, Pietras Z, Furnham N et al. Assembly and channel opening in a bacterial drug efflux machine. Mol Cell 2008; 30: 114–21. 50. Vaccaro L, Koronakis V, Sansom MSP. Flexibility in a drug transport accessory protein: molecular dynamics simulations of MexA. Biophys J 2006; 91: 558–64. 972