* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Dynamic imaging of host–pathogen interactions in vivo
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
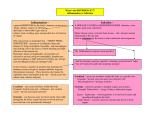
REVIEWS Dynamic imaging of host–pathogen interactions in vivo Janine L. Coombes and Ellen A. Robey Abstract | In the past decade, advances in microscopic imaging methods, together with the development of genetically encoded fluorescent reporters, have made it possible to directly visualize the behaviour of cells in living tissues. At the same time, immunologists have been turning their attention from the traditional focus on responses to model antigens to a new focus on in vivo infection models. Recently, these two trends have intersected with exciting results. Here we discuss how dynamic imaging of in vivo infection has revealed fascinating and unexpected details of host–pathogen interactions at a new level of spatial and temporal resolution. Confocal microscopy A focused beam of light is scanned across the sample. Emitted light not from the focal point of the lens on the tissue is prevented from reaching the detector by a pinhole, reducing out-of-focus signal. The microscope obtains a series of in focus images at varying tissue depths, termed optical sectioning. Two-photon laser-scanning microscopy (TPLSM). An imaging method based on the excitation of fluorophores by absorption of energy from two photons, with each photon contributing half of the energy required for excitation. Consequently, each photon is twice the wavelength that would be required for single photon excitation leading to deeper tissue penetration compared to other imaging methods. Department of Molecular and Cell Biology, Life Sciences Addition, University of California, Berkeley, California 94720, USA. Correspondence to E.A.R. e‑mail: [email protected] doi:10.1038/nri2746 Published online 16 April 2010 The interaction between pathogens and the host immune system is multilayered, with each player having to recognize, respond and adapt to the other. Pathogens have evolved strategies to manipulate and evade host immune responses to optimize their survival or transmission. For example, Streptococcus pyogenes produces virulence factors that can modulate the recruitment of immune cells to the site of infection, whereas Toxoplasma gondii is thought to use the migratory pathways of immune cells to spread throughout the body 1–4. Meanwhile, the host immune system must balance the requirement to control the pathogen with the potential for damaging its own tissues. Further complexity occurs when the influence of the local tissue environment on both immune cells and the invading pathogen is taken into account. For example, bacterial pathogens might use two component regulatory systems to sense their environment and alter the expression of virulence factors, whereas the function of dendritic cells (DCs) can be altered in response to epithelial cell-derived factors5,6. An understanding of how the tissue environment influences the interaction between the host and pathogens is crucial for the development of effective vaccines and therapies. To this end, there are many useful animal infection models that allow the study of immune responses occurring in physiologically relevant tissues. Using such models, ex vivo assays and static imaging studies have taught us much about the interaction between the host and pathogens. However, as we discuss in this Review, the dynamic behaviour of a cell or pathogen in an intact living tissue has the potential to reveal much more. Dynamic in situ imaging can be achieved using widefield epifluorescence microscopy or confocal microscopy , but both techniques are limited with respect to the depth of tissue that can be penetrated, which limits analysis to surface events. Recently, two-photon laser-scanning microscopy (TPLSM) has been used to image immune responses in intact tissues, providing increased tissue penetration and decreased photodamage and improving the ability to carry out time-lapse imaging of living tissues7. An additional advantage of TPLSM over other types of fluorescence microscopy is the generation of second harmonic signals that allow the identification of characteristic tissue structures, such as lymph node capsules and reticular fibres (BOX 1). Combined with methods for the identification and tracking of specified host cells and structures, TPLSM studies have provided surprising new insights into how immune cells interact with their environment, and one another, and what the functional outcomes of such interactions are (BOX 1). For example, in the lymph nodes, T cells were shown to migrate along a network of fibroblastic reticular cells with which DCs are also associated8–10. This behaviour is likely to have important implications for the ability of T cells to survey the lymph node for antigen. Methods for objectively quantifying cell motility and cell–cell interactions further increase the value of dynamic in situ imaging. Image analysis software can be used to track individual cells in the three dimensional area being imaged over time. Parameters such as the average speed of the cell and how long it spends in contact with defined cells or structures can then be measured. Furthermore, time-lapse imaging is often most informative when it is combined with other approaches that allow investigation of the functional nATURe RevIewS | Immunology voLUMe 10 | MAy 2010 | 353 © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS Box 1 | Approaches used to identify host cells and structures for time-lapse imaging in situ Expression of fluorescent reporters using cell-type-specific promoters • CD11c promoter driving expression of enhanced yellow fluorescent protein (CD11c–EYFP), which marks dendritic cells4,15,40,51,57,60. However, not all reporter-expressing cells are surface CD11c positive. • Lysozyme M promoter driving expression of enhanced green fluorescent protein (LysM–EGFP), which marks neutrophils, monocytes and macrophages. Neutrophils express higher levels of the reporter and have different morphology and motility to macrophages18,22–24,29,32,61. • CX3C-chemokine receptor 1 (CX3CR1) promoter driving expression of EGFP (CX3CR1–EGFP), which marks monocytes and dendritic cells62,13. • MHC class II-expressing cells, such as B cells and CD11c+ cells, can be visualized by replacing the gene encoding the I–Ab β-chain with a construct encoding an EGFP-tagged version (MHC class II–EGFP)14,16. Adoptive transfer of labelled host cells in vivo • Cell populations can be labelled using dyes, such as 5,6-carboxyfluorescein diacetate succinimidyl ester (CFSE) or by isolating them from mice expressing fluorescent proteins ubiquitously; for example, under the control of the ubiquitin or actin promoters. Genetic labels are preferable owing to the potential for dyes to be diluted with cell division. Either technique requires the transferred host cell population to migrate to the appropriate location after in vivo transfer. It is typically used to introduce labelled antigen-specific T and B cells4,7,23,32,36–41,49,51,53,56–58. Illumination of stromal cells • Mice expressing fluorescent proteins ubiquitously can be irradiated and transferred with non-fluorescent bone marrow, illuminating the stromal cell network8,39. Endogenous signals • Tissue structures such as the lymph node capsule and reticular fibres can be illuminated in two-photon laser-scanning microscopy by the generation of second harmonic signals. This occurs when two incident photons pass through a noncentrosymmetric structure (such as collagen-rich structures) and emerge as one photon with half the incident wavelength39,58. • The natural autofluorescence of the tissue can also be used to define cells and structures of interest. However, these signals lack specificity for a particular cell type and can be difficult to visualize in the presence of a brighter fluorescent protein28,29. Injection of vascular tracers • Intravenous injection of quantum dot tracers can be used to identify blood vessels and follow changes in vascular permeability22,32. Subcapsular sinus macrophages can be labelled by subcutaneous injection of antibodies specific for CD169 taking advantage of lymphatic drainage to the lymph node capsule4,23,36. Second harmonic signals Signals that occur when two incident photons pass through a structure with no centre of symmetry and emerge as one photon with half the incident wavelength. In biological tissues this is mostly a property of collagen. consequences of the observations made during imaging. For example, flow cytometry of dissociated cell populations can be used to determine how changes in motility might correlate with changes in cell activation or cytokine production. Static imaging of tissue sections can be used to assess global changes in the distribution of a cell population and, finally, new observations made during the imaging process may suggest target pathways for genetic manipulation, allowing assessment of their role in the generation of an optimal immune response. However, until recently, the dynamics of the immune response to pathogens remained under-explored. Fortunately, improved availability of tools for labelling and tracking of pathogens in vivo has allowed researchers to address questions such as how pathogens alter the behaviour of infected cells, how infected cells are recognized by the immune system and how the pathogen spreads through the host in intact tissues in real time (FIG. 1; see Supplementary information S1, S2, S3, S4 (movies)). Here, we discuss how recent studies have revealed unique features of the dynamics of the host immune response to pathogens. Although we focus on timelapse imaging of intact tissues, key supporting data from static imaging, analysis of dissociated ex vivo samples and in vitro studies are also mentioned. Host– pathogen interactions are extremely diverse and we therefore do not attempt to provide a comprehensive discussion of all of the interesting imaging studies that have been published (TABLE 1). Rather, we focus on a handful of studies that provide new insights into the dynamics of the interaction between the host immune system and pathogens across various locations and infection models. The initial encounter The site where a pathogen breaches the hosts’ epithelial cell defences is often the first opportunity for contact between the host immune system and the pathogen, and therefore it may be the first opportunity for clinical intervention. Tissue-resident populations of DCs and macrophages are among the first to encounter the pathogen and may be involved in transport of the pathogen across epithelial cell barriers11,12. In addition, monocytes constitutively patrol tissue blood vessels, ready to respond rapidly to infection or tissue damage13. Subsequently, large infiltrates of neutrophils arrive in the tissue. our understanding of these processes — how they contribute to the control of infection and how they are subverted by pathogens — has been substantially advanced by recent dynamic imaging studies. 354 | MAy 2010 | voLUMe 10 www.nature.com/reviews/immunol © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS Aa T. gondii Ab 1 min 0 min 1.5 min 2 min Release of parasite Cyst Release of parasite Ac 20 min 19 min BCG 0 min B 3.5 min 7 min Saphenous vein Capsule SCS Parenchyma VSV SCS floor 0 min 10 min 29 min Figure 1 | Examples of visualizing pathogens. A | Protozoan parasites, such as Plasmodium spp., Leishmania major and Toxoplasma gondii areNature sufficiently large that Reviews | Immunology individual fluorescently labelled parasites can be readily tracked within tissues using widefield epifluorescence, confocal or two-photon laser-scanning microscopy. In these examples, red fluorescent protein-labelled T. gondii parasites (red) were observed invading a T cell (green) during an antigen-dependent contact with another invaded cell in the lymph node (a) and emerging from a rupturing cyst in the brain (b). Bacteria engineered to express fluorescent proteins have also been detected by two-photon laser-scanning microscopy in tissues14,32. This example (c) shows uptake of Mycobacterium bovis bacille Calmette–Guérin (BCG) (red) by Kupffer cells (green) in the liver32. B | Bulk movement of fluorescently labelled virus particles has been visualized in vivo39. In this example, fluorescently labelled, inactivated vesicular stomatitis virus (VSV) particles (green) were seen to accumulate in discrete patches in the subcapsular sinus (SCS) of draining lymph nodes within minutes of subcutaneous injection. Virus-infected host cells have also been visualized using viruses that are engineered to express green fluorescent protein derivatives40,68. The image in part Aa is reproduced, with permission, from REF. 4 © (2009) Elsevier Science. The image in part Ab is reproduced, with permission, from REF. 57 © (2009) The American Association of Immunologists, Inc. The image in part Ac is reproduced, with permission, from REF. 32 © (2008) Elsevier Science. The image in part B is reproduced, with permission, from Nature REF. 39 © (2007) Macmillan Publishers Ltd. All rights reserved. Response of tissue-resident cells. Populations of peripheral tissue-resident innate immune cells function as sentinels for infection and tissue damage. DCs in both the skin and small intestine have been observed rapidly extending processes towards microorganisms following infection, confirming earlier static imaging studies11,12,14,15. In the intestine, the DCs (identified using MHC class II–enhanced green fluorescent protein (eGFP)) (BOX 1) extended processes across the epithelial cell layer and into the lumen where they were occasionally seen to interact with non-invasive Salmonella enterica subsp. enterica serovar Typhimurium organisms14,16. This is consistent with the hypothesis that DC processes may be involved in the transport of microorganisms across the intestinal epithelium11,12,14. Use of TPLSM of DCs in the skin (using CD11c promoter-driven expression of yellow fluorescent protein (yFP)) (BOX 1) led to the surprising finding that, unlike sessile Langerhans cells in the epidermis, dermal DCs could crawl actively through the tissue. However, following intradermal injection of Leishmania major, dermal DCs slowed substantially, gained a more pronounced dendritic morphology and took up L. major through the extension of dendrites15. Loss of migratory behaviour in vivo also occurred in the presence of lipopolysaccharide15. By contrast, DCs did not acquire a dendritic morphology in response to inert beads or Mycobacterium bovis bacille Calmette–Guérin (BCG). Moreover, the uptake of beads and BCG was inefficient compared with uptake of L. major. The reasons for this difference in DC behaviour warrant further investigation. For example, comparing the responses that dermal DCs have towards BCG, virulent mycobacterial strains and other intradermal vaccines might help to determine whether engineering vaccines to provide signals that alter DC behaviour would make them more effective. Real-time imaging studies have revealed that DCs are supported in their sentinel function by a population of monocytes expressing high levels of CX3C-chemokine receptor 1 (CX 3 CR1) (visualized using CX 3 CR1 promoter-driven GFP expression) (BOX 1). CX3CR1hi monocytes have an unusual patrolling behaviour for surveying blood vessels and tissues for signs of infection or damage. In the steady state, the monocytes were observed crawling along the luminal surface of the blood vessel endothelium, independently of the direction of blood flow13. This behaviour resulted in extensive monitoring of the surface of the vessel, but not in extravasation of the monocytes. However, following intraperitoneal infection with Listeria monocytogenes, CX3CR1hi monocytes extravasated into the peritoneal cavity with faster kinetics than neutrophils or GR1+ inflammatory monocytes and were an important early source of tumour necrosis factor 13. Importantly, disruption of steady-state patrolling behaviour in CX3CR1deficient mice led to delayed monocyte extravasation following infection, showing the importance of constitutive surveillance of the vessels. It will be of interest to determine whether some pathogens target the behaviour of CX3CR1hi monocytes to avoid detection. nATURe RevIewS | Immunology voLUMe 10 | MAy 2010 | 355 © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS Table 1 | Time-lapse imaging in mammalian in vivo infection models Pathogen Imaged tissue Imaged host cell population Refs Protozoan parasites Plasmodium spp. Skin Myelomonocytic cells, dermal cells and blood vessel endothelial cells Lymph nodes T cells Liver Kupffer cells and hepatocytes Brain T cells Skin Neutrophils, dendritic cells and T cells Lymph nodes NK cells, T cells and dendritic cells Lymph nodes T cells, dendritic cells, macrophages and neutrophils Brain T cells, dendritic cells and astrocytes Vaccinia virus Lymph nodes T cells and dendritic cells 40 Vesicular stomatitis virus Lymph nodes B cells 39 LCMV CNS Neutrophils, monocytes and T cells 22 Vaccinia virus Ankara BALT T cells and dendritic cells 68 Mycobacterium bovis BCG Liver Kupffer cells, macrophages and T cells 32 Listeria monocytogenes Spleen Dendritic cells and T cells 70 Skin Neutrophils 71 Streptococcus pyogenes Skin Neutrophils 18 Escherichia coli Kidney Blood vessels 72 Salmonella typhimurium Intestine Dendritic cells 14 Staphylococcus aureus Blood Blood vessels 73 Borrelia burgdorferi Blood Blood vessels 74,75 Leishmania major Toxoplasma gondii 26–28 53 29,33–35 69 24,25,56 41 4,23,51 57,58 Viruses Bacteria BALT, bronchial-associated lymphoid tissue; BCG, bacille Calmette–Guérin; CNS, central nervous system; LCMV, lymphocytic choriomeningitis virus; NK, natural killer. Bacille Calmette–Guérin (BCG). A strain of live attenuated Mycobacterium bovis used for vaccination against Mycobacterium tuberculosis in humans. Subcapsular sinus The outer region of the lymph node where afferent lymph first enters the lymph node. It consists of a sponge-like network of reticular fibroblast cells encasing collagen fibres and is separated from the lymph node cortex by a layer of sinus-lining cells and a discontinuous basement membrane. Neutrophil interactions with pathogens. The initial encounter with sentinel cells is followed quickly by the influx of leukocytes, of which neutrophils are often the most prominent. once present in the tissue, neutrophils have many functions, including the destruction of microorganisms, tissue remodelling, the production of chemokines and the eventual resolution of the inflammatory response17. Dynamic in situ imaging of neutrophils during infection has provided new insights into these various functions. Imaging of neutrophil recruitment to the site of infection following bacterial infection suggests that the rate of neutrophil extravasation is important for protection against infection and may be subject to modification by bacterial virulence factors18. Streptolysin S is a broadspectrum cytolysin, the expression of which might be regulated by conditions in the tissue environment 19. It is thought to decrease the neutrophilic infiltrate at the site of infection through a direct cytocidal effect but recent imaging studies have revealed another potential mechanism18,20. TPLSM studies of LysM–eGFP mice (in which eGFP expression is driven by the lysozyme M promoter (BOX 1)) showed that infection with both wildtype and streptolysin S-mutant S. pyogenes led to similar levels of neutrophil rolling and firm adherence in blood vessels, as well as similar neutrophil migration in the infected tissue18. However, the amount of time that the neutrophils remained in the vessels before extravasating was substantially shorter in the presence of the streptolysin S mutants. It is possible that streptolysin S may increase the virulence of S. pyogenes by impairing neutrophil diapedesis and that the delay in the arrival of neutrophils provides a short window of opportunity for the bacteria to begin replicating and establish a niche. This provides an excellent example of how dynamic imaging has helped to define a precise mechanism by which a pathogen virulence factor can modulate the host immune response. It also suggests that targeting signals in the local tissue environment that modulate expression of pathogen virulence factors could be beneficial in fine tuning the immune response to control infection while limiting pathology. neutrophil extravasation is known to be associated with vascular leakage and tissue injury 21. This process has been captured in real time during lymphocytic choriomeningitis virus (LCMv) infection of the central nervous system, in which vascular leakage results in fatal seizures. neutrophils were observed accumulating in the vasculature before a coordinated and rapid extravasation that was accompanied by leakage from the vasculature of a quantum dot tracer 22 (Supplementary information S5 (movie)). Seizure-induced death was prevented in mice depleted of both monocytes and neutrophils, suggesting that blocking their recruitment could be useful in preventing immune-mediated pathology in the central nervous system. Dynamic imaging has also provided evidence of neutrophils altering local tissue architecture. Following T. gondii infection, swarming of neutrophils in the lymph node corresponded in space and time with disruption of the layer of CD169+ macrophages in the subcapsular sinus23. Although it remains to be determined, it is possible that neutrophil-mediated remodelling of the extracellular matrix contributed to the migration of these cells to other regions of the lymph node23. Imaging the neutrophil response to L. major infection provided insight into how a pathogen may use neutrophils in the dermis for its own benefit 24. A rapid and sustained recruitment of LysM–eGFPhi neutrophils from the blood to the site of infection was observed. neutrophils accumulated near both infected and uninfected sand fly bites, seeming to form plugs within them. Initially, most of the parasites were observed in neutrophils, but they were later also found in macrophages. Interestingly, parasites in neutrophils remained viable and infectious and were observed being released from apoptotic neutrophils in the vicinity of macrophages24. This real-time observation, combined with the finding that depletion of 356 | MAy 2010 | voLUMe 10 www.nature.com/reviews/immunol © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS neutrophils decreased infection levels, suggested that the parasite could exploit the neutrophil response to tissue injury to enhance its survival and replication. It has been suggested that uptake of infected neutrophils by macrophages might allow the parasite to reach its preferred host cell without initiating an inflammatory response24. Alternatively, the microbicidal function of the macrophages may already be compromised by uptake of apoptotic neutrophils, enabling released parasites to infect them more easily. The interplay between vector, parasite and host immune cells revealed by these studies has important implications for vaccine design. Certain experimental, non-living vaccine strategies for leishmaniasis are effective against needle challenge with L. major but not against natural challenge with a sand fly bite harbouring live parasites25. TPLSM studies revealed that infected sand fly exposure led to a more sustained neutrophil response than needle inoculation, suggesting that neutro phils may dampen the antiparasite response and promote infection25. Consistent with this explanation 25, neutrophil depletion following sand fly challenge enhanced the protective effect of a killed vaccine. These findings emphasize the importance of natural challenge to assess vaccine efficacy and the power of imaging to reveal aspects of the host–pathogen interaction that are relevant to vaccine design. Liver sinusoids Specialized blood vessels lined by a fenestrated endothelium and interspersed Kupffer cells. Kupffer cells A specialized population of macrophages that reside in the liver. Granuloma An organized structure containing macrophages and other immune cells. Migration and invasion of Plasmodium spp. in the skin. The malaria-causing parasites Plasmodium spp. have provided some of the most rewarding infection models for imaging studies, both because of the high relevance for human health and because of the varied and dynamic events that take place during the parasite life cycle in the mammalian host (FIG. 2a,b). This cycle begins when parasites are injected into the dermis by the bite of an infected mosquito (FIG. 2a). Time-lapse imaging of Plasmodium berghei sporozoites (which infect mammals other than humans and are therefore used in animal model studies) in the dermis of mice has added to our appreciation of how the sporozoites disseminate from the site of infection and how this process can be locally modulated by the host immune response (Supplementary information S6 (movie)). Sporozoites remained motile for some time after infection and were seen to invade both blood and lymphatic vessels26–28. Their motility depended on the ability to traverse host cells, and this allowed them to avoid becoming trapped in stromal cells or cleared by phagocytes26. non-motile parasites rarely penetrated as far as the vasculature, limiting dissemination. Blood borne, P. berghei sporozoites invade the liver rapidly, limiting the time frame during which they are susceptible to neutralization with antibodies in the blood76. However, these studies26–28 revealed that there was a substantial period of time during which motile parasites and the host immune system could interact in the dermis, suggesting a larger window of opportunity for vaccines that target this stage of the infection than had previously been appreciated. In fact, when mice, previously immunized with radiation-attenuated parasites, were challenged by mosquito bite, sporozoites lost motility within one minute of infection28. Consistent with this, the sporozoites did not gain access to the vasculature in immunized mice. A similar effect was achieved with passive transfer of antibodies28. The liver stage of Plasmodium spp. infection Sporozoite transit through Kupffer cells. Like many pathogens, Plasmodium spp. disseminate from the initial site of infection through the blood and travel to the liver. There, the parasites enter liver sinusoids, where they encounter specialized liver macrophages known as Kupffer cells. when P. berghei sporozoites entered the liver, they bound to the sinusoidal cell layer and arrested. They were then observed gliding along the sinusoidal endothelium until they encountered a LysM–eGFPlow Kupffer cell29 (BOX 1; FIG. 2c,d; see Supplementary information S7 (movie)). The sporozoites then entered and passed through the Kupffer cells into the liver parenchyma where they traversed through multiple hepatocytes. This realtime observation confirmed the long-held hypothesis that Kupffer cells could act as a gateway to the liver for Plasmodium spp. sporozoites30. The importance of Kupffer cells for entry of the parasite into the liver is further supported by a recent study in which a reduction in Kupffer cell numbers led to a decrease in parasite load 31. Real-time imaging has also shown that Kupffer cells can participate in the uptake of BCG from the blood32 (FIG. 1Ac; see Supplementary information S3 (movie)). These Kupffer cells subsequently nucleated granuloma formation32. How merozoites avoid phagocytosis by Kupffer cells. After traversing several hepatocytes, Plasmodium spp. sporozoites invade a final hepatocyte and develop into exo-erythrocytic forms that enter exo-erythrocytic schizogony, potentially yielding thousands of merozoites in a single infected cell (FIG. 2c,e). Merozoites are then released into the blood where they infect erythrocytes. Kupffer cells are thought to have an important role in this stage of infection, as merozoites are highly susceptible to phagocytosis. However, recent intravital imaging studies have provided important details concerning how the mouse parasites P. berghei and Plasmodium yoelii are released from the liver and how they can evade phagocytosis33–35. Groups of merozoites were observed budding off from infected hepatocytes in the form of vesicles with host cell-derived membranes termed merosomes (FIG. 2e; see Supplementary information S8 (movie)). Merosomes reached the blood, possibly through endothelial cell fenestrations, and their formation was eventually followed by disintegration of the host cell. Importantly however, the merosomes did not expose phosphatidylserine on their outer surface, protecting them from phagocytosis33,34. By contrast, disintegration or rupture of infected hepatocytes left merozoites susceptible to phagocytosis and led to inflammatory cell recruitment and the formation of small granulomatous structures33. nATURe RevIewS | Immunology voLUMe 10 | MAy 2010 | 357 © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS a c Mosquito Epidermis Dermis Sporozoite Blood vessel Sinusoidal endothelial cell Hepatocyte Sinusoidal lumen Lymphatics Lymph node Merozoite Merosome Kupffer cell Sporozoite Liver Infected hepatocyte Parasitophorous vacuole b 48 0 270 180 120 108 72 d 90 0–270 sec e Merosome bud 282 sec Merosome 288 sec 300 sec Figure 2 | Dynamic imaging of Plasmodium spp. infection in mammals. a | Plasmodium spp. sporozoites are injected into the dermis by a mosquito bite, and they migrate through the dermis before actively invading across the endothelium of blood Nature Reviews | Immunology or lymphatic vessels26–28. b | These images show the path of a Plasmodium sporozoite migrating in the dermis, represented by maximum intensity projection of fluorescent signal. The sporozoite glides in the dermis (gliding sporozoite shown in red) before gliding along a blood vessel wall (green, with blood vessel marked in blue) and finally crossing the blood vessel wall (yellow). c | After dissemination through the blood to the liver, sporozoites glide along sinusoids and enter the liver parenchyma through Kupffer cells. After converting into merozoites in the hepatocytes, the parasites avoid being phagocytosed by Kupffer cells by budding as membrane covered merosomes29,33–35. d | The path of a Plasmodium spp. sporozoite (green) gliding along a liver sinusoid and then encountering a Kupffer cell (outlined with dotted line). The sporozoite is then seen traversing the Kupffer cell and continuing its migration in the liver tissue (not depicted). e | These images show a merosome (green) that is budding off from a green fluorescent exo-erythrocytic form into a sinusoid (red). The image in part b is reproduced, with permission, from Nature Medicine REF. 27 © (2006) Macmillan Publishers Ltd. All rights reserved. The image in part d is reproduced from REF. 29. The image in part e is reproduced, with permission, from REF. 34 © (2006) American Association for the Advancement of Science. Real-time imaging of Plasmodium infection has undoubtedly been successful in confirming the elegant way in which the parasite uses Kupffer cells to access the liver but later successfully avoids a potentially lethal interaction with this same cell type. First encounters in lymph nodes Encounters between pathogens and subcapsular sinus macrophages. From the site of infection, microorganisms and microbial particles drain to the lymph nodes and are deposited in the subcapsular sinus. There, they interact with a specialized subset of macrophages that protrude through the layer of sinus-lining cells36–39. These macrophages express CD169 (sialoadhesin) and differ from conventional macrophage populations in that they are poorly endocytic and poorly degradative36. However, they do have an important role in selectively trapping large and particulate antigen that enters via the lymph with important consequences for the generation of immune responses and limiting pathogen dissemination36–39. For example, fluorescently labelled inactivated vesicular stomatitis virus (vSv), injected into the footpad, rapidly accumulated on the surface of CD169+ macrophages protruding across the subcapsular sinus floor 39 (FIG. 1B). 358 | MAy 2010 | voLUMe 10 www.nature.com/reviews/immunol © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS Depletion of subcapsular sinus macrophages showed their importance in retaining the virus in the lymph node, thereby limiting its spread throughout the body. Similarly, P. berghei travelled from the dermis to the draining lymph node, where it was initially concentrated in the subcapsular sinus and was found associated with CD11c + cells 27. Parasites gradually lost motility and did not penetrate further than the lymph node, suggesting that the pathogen-trapping function of cells in the subcapsular sinus was also important in this model. Although subcapsular sinus macrophages efficiently limit pathogen dissemination, trapping of intracellular pathogens at the cell surface may expose these cells to invasion. within an hour of subcutaneous infection, T. gondii arrives in the draining lymph node and is found in CD169+ macrophages23. Many of the parasites were surrounded by dense granule protein 6 (GRA6), indicating that they resided in parasitophorous vacuoles and therefore had actively invaded the macrophages4. Furthermore, expression of virus-encoded GFP by infected host cells was used to show that vaccinia virus could also infect CD169+ macrophages following subcutaneous infection40. Activation of innate immunity: neutrophils and natural killer cells. The arrival of intact viable pathogens in the lymph node necessitates the local generation of an innate immune response. Indeed, it seems that an innate immune response analogous to that seen in non-lymphoid tissues can also be initiated in the lymph nodes following the arrival of lymph-borne pathogens. Both neutrophils and natural killer (nK) cells circulate in the blood and can be recruited to lymph nodes following infection. Recent studies have revealed new information concerning the dynamics and spatial organization of the response of these two cell types to infection with protozoan parasites in the lymph nodes23,41 (TABLE 1). For example, following T. gondii infection, neutrophils formed dynamic swarms around foci of infection in the subcapsular sinus region. Interestingly, many swarms were initiated by clustering of a few ‘pioneer’ neutrophils followed by migration of large numbers of neutrophils several minutes later 23 (FIG. 3a; see Supplementary information S9 (movie)). This suggested that the formation of neutrophil swarms was cooperative: swarming neutrophils produced chemoattractants that brought new neutrophils to the swarm. neutrophil swarms also formed rapidly in response to egress of T. gondii from an infected cell23 (Supplementary information S10 (movie)). It is likely that a diverse range of pathogens and vaccine strains will accumulate in the subcapsular sinus and initiate an inflammatory response. Given the profound effect that the neutrophil response to L. major in the skin has on vaccine efficacy, it may be informative to investigate the effect of neutrophil swarming in the lymph node on the ability of pathogens or vaccines to elicit adequate immune responses. It will also be important to determine the nature of the signals that trigger this swarming behaviour, so that they may be targeted for the generation of an optimal immune response42,43. nK cells have an important role in early defence against various infectious agents. Their effector functions can be initiated following engagement of activating cell surface receptors or in response to cytokines produced by macrophages and DCs. In fact, nK cell activation by DCs is thought to be cell-contact dependent, and nK cells have been observed forming long-lasting contacts with DCs in vitro44–46. Similarly, optimal production of interferon-γ by nK cells following L. monocytogenes infection depends on their ability to cluster around foci of myeloid cells in the spleen47. Recently, the dynamics of the nK cell response in lymph nodes and the nature of their contacts with DCs have begun to be explored using time-lapse imaging 41,48,49. For example, in L. major infection, nK cells interacted with DCs in the lymph node paracortex, suggesting a means by which they may receive activating signals41. Priming of the adaptive immune response The observation that lymph-borne pathogens became associated with CD169 + subcapsular sinus macrophages suggested that the region directly beneath the subcapsular sinus may be a previously under-appreciated location where lymphocytes could recognize their cognate antigen and be primed, and it indicates that the CD169+ macrophages may be involved in the optimal generation of adaptive immune responses. Recognition of pathogens by B cells at the subcapsular sinus. As described in the previous section, subcapsular sinus macrophages can extend across the floor of the subcapsular sinus into the lumen, and viruses arriving through lymph accumulate on their surface. This allows the macrophages to transport and present viruses to B cells in the superficial follicle39 (FIG. 3b; see Supplementary information S11 (movie)). TPLSM studies showed that these macrophages were largely immobile, suggesting that virus was transported along the surface of the cell. Specific B cells congregated beneath the floor of the subcapsular sinus, probably as a result of receiving a stop signal through the B cell receptor during random surveying of macrophages in the region. Although other pathways exist, trapping of virus by subcapsular sinus macrophages was necessary for efficient antigen presentation to B cells soon after infection. This might prove to be important, as even minor alterations to the kinetics of an immune response can affect the ability of the host to control infection. Immune complexes and other particulate antigens have also been shown to accumulate on the surface of subcapsular sinus macrophages and be transported along the cell surface into the B cell follicle36–38. Immune complexes can then be captured by non-cognate B cells and transported to the germinal centre. Disruption of this process leads to impaired affinity maturation36. Together, these imaging studies suggest a pathway for antigen capture and transport involved in the optimal generation of B cell responses. Recognition of pathogens by T cells at the subcapsular sinus. The prevailing spatial and temporal model of T cell priming in the lymph nodes is based largely on dynamic imaging of responses to model antigens7,50. nATURe RevIewS | Immunology voLUMe 10 | MAy 2010 | 359 © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS a Capsule Stage 1 Stage 2 Subcapsular sinus Neutrophil Toxoplasma gondii 7 min 24 min b Virus Subcapsular sinus macrophage Sinus-lining cell Virus-specific B cell Non-specific B cell c Toxoplasma gondii T cell Infected macrophage Dendritic cell 0 min 13 min 25 min Infected T cell Figure 3 | Dynamic imaging of immune responses in the lymph node subcapsular sinus. a | Neutrophils (expressing enhanced green fluorescent protein driven by the lysozyme M promoter) exhibit biphasic swarm formation Nature Reviewsin| the Immunology subcapsular sinus following Toxoplasma gondii (red) infection. The tracks of the neutrophils in stage 1 and stage 2 of swarm formation are depicted as white lines. b | Viral particles (green) accumulate on CD169+ macrophages in the subcapsular sinus following subcutaneous injection. This leads to accumulation of virus-specific B cells (red) within and below the subcapsular sinus floor. c | During T. gondii (red) infection, memory CD8+ T cells (green) form clusters around uninfected dendritic cells and infected CD169+ macrophages (orange), exposing themselves to invasion by parasites. The image in part a is reproduced, with permission, from REF. 23 © (2008) Elsevier Science. The image in part b is reproduced, with permission, from Nature REF. 39 © (2007) Macmillan Publishers Ltd. All rights reserved. The image in part c is reproduced, with permission, from REF. 4 © (2009) Elsevier Science. Briefly, soluble antigens arrive first in the lymph node and filter through a network of conduits extending into the cortex. DCs that reside in the cortical ridge can sample this antigen and present it to T cells arriving through high endothelial venules. Later, antigen-loaded tissue DCs arrive in the lymph node and also localize to the cortical ridge, where they present antigen to T cells. However, it remains unclear where priming of the T cell response occurs during infection and if the location of priming affects the outcome of the response. Three recent studies have carried out imaging of specific CD8+ T cell responses in the subcapsular sinus region following infection with pathogens engineered to express the model antigen ovalbumin4,40,51. In each case, the pathogen studied was shown to accumulate in the subcapsular sinus region and was found in CD169+ macrophages. This suggested that T cells might initially encounter parasite-derived antigens in this region of the lymph node. Indeed, both naive and memory CD8+ T cells accumulated in the region of the subcapsular sinus following infection. In the case of T. gondii infection, T cell relocalization was antigen independent, suggesting that the T cells responded to chemoattractants produced at the site of infection4,51. By contrast, in vaccinia virus infection, redistribution of the CD8+ T cells was shown to be more dependent on the presence of cognate antigen, implying that retention of T cells by antigen recognition has a role in relocalization40. 360 | MAy 2010 | voLUMe 10 www.nature.com/reviews/immunol © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS The nature of the antigen-presenting cells (APCs) for T cells at the subcapsular sinus is of considerable interest. In the case of naive T cell priming by viruses, T cells did not cluster around virus-infected CD169+ macrophages but, instead, around CD11c–yFP+ cells present beneath the macrophage layer. These interactions seemed to result in T cell priming, as T cells upregulated activation markers in the first 12 hours following infection and rapidly migrated back to the site of infection40. For memory CD8+ T cells responding to T. gondii, long-lived low-motility clusters formed around infected CD169+ macrophages in an antigen-dependent manner, suggesting that subcapsular sinus macrophages do serve as APCs in this setting 4 (FIG. 3c; see Supplementary information S12 (movie)). In this 4 and the related studies40,51, T cell clusters were also observed around CD11c–yFP+ cells that did not harbour visible fluorescent pathogens. Thus both direct presentation by macrophages and bystander presentation by DCs seem to contribute to T cell antigen recognition in the subcapsular sinus. Collectively, these studies suggest that the region of the lymph node beneath the subcapsular sinus is a site for early priming or reactivation of the immune response to pathogens. It is likely that tissue microenvironments have an important role in determining the course of an immune response. It is therefore of substantial interest that early CD8+ T cell responses can be activated in this region of the lymph node. It will be important to determine whether these cells differ from those primed later in the response or deeper within the lymph node, and how priming in this region shapes the overall character of the immune response. Pathogens fight back. The presence of live pathogens in the lymph node during priming of the adaptive response might allow the pathogen to manipulate this phase of the response for its own benefit. For example, CD8+ T cells clustered around T. gondii-infected cells were occasionally invaded themselves following lysis of the infected target cell4 (FIGS 1A,3c; see Supplementary information S1 (movie)). This finding implies that the parasite may take advantage of close APC–T cell contacts to invade T cells and disseminate systemically within them. Accordingly, T cells accounted for 50% of infected cells in the mesenteric lymph node following oral infection4. Furthermore, blocking egress of lymphocytes from the lymph node was effective in reducing parasite spread4. Pathogen products may also influence priming of the response to subsequent challenges. Malaria infection is known to result in impaired responsiveness to secondary infections, presenting a significant barrier to vaccination. Uptake of the malaria pigment haemozoin by DCs is thought to contribute to suppression of the immune response in this setting 52. TPLSM was used to better define how plasmodium infection might modulate DC function and, consequently, the interaction of DCs with T cells following secondary challenge53. Mice received an intraperitoneal injection with Plasmodium chabaudi-infected erythrocytes and 12 days later were administered 5,6-carboxyfluorescein diacetate succinimidyl ester (CFSe)-labelled Do11.10 CD4+ T cells and immunized with ovalbumin and lipopolysaccharide. Immunization of uninfected animals resulted in a marked decrease in T cell average speed and displacement. This decrease was less pronounced in malaria-infected mice, although T cells still upregulated early activation markers, indicating that they recognized antigen but failed to form stable contacts with DCs. Mechanistically, this was thought to be due to uptake of haemozoin by DCs. Antigen-specific DC–T cell interactions were inhibited in vivo when DCs were pulsed with haemozoin before adoptive transfer. This is similar to decreased stable contacts formed when regulatory T cells are present 54,55. It might therefore be informative to visualize regulatory T cell populations in this setting. T cell responses in peripheral tissues During activation in lymphoid tissues, T cells receive signals from DCs that lead to upregulation of tissuehoming receptors, allowing them to migrate to sites of infection. Few studies have addressed the dynamics of the interaction between T cells, infected cells and other APCs at this stage of the immune response. How do effector T cells migrate through inflamed tissues? Do all infected cells have the potential to be recognized by T cells and what are the dynamics of T cell interactions with uninfected APCs at sites of infection? These issues have recently been examined in the settings of L. major infection in the skin56, T. gondii infection in the brain57,58 and mycobacterial infection in the liver 32. In the skin. visualization of CD4 + T cell effector responses to infection with L. major in the skin revealed several unexpected features56. effector T cells entered infected regions of the skin regardless of antigen specificity, while T cells specific for an immunodominant L. major antigen slowed down and accumulated near parasites. A subset of antigen-specific T cells arrested and formed stable contacts with infected cells, whereas others made transient contacts while continuing to crawl over infected cells. Interestingly, the distribution of T cells was not uniform, with some infected areas being extensively patrolled by T cells and others seeming to be poorly accessible. Furthermore, many infected cells failed to engage T cells, even when antigen-specific T cells were in close proximity. Although this study largely focused on T helper 2 (TH2)-polarized cells and a genetically susceptible mouse strain, similar behaviour was also seen with TH1-polarized cells and in mice genetically resistant to the parasite, implying that these are general features of the CD4+ effector T cell response to L. major. These observations raise several interesting questions for future studies: what limits the ability of T cells to access certain infected regions? what determines whether T cells respond to particular APCs? And what are the consequences of the heterogeneous response of T cells to infected cells on their ability to control infection and induce pathology? nATURe RevIewS | Immunology voLUMe 10 | MAy 2010 | 361 © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS In the brain. The establishment of chronic infection by the parasite T. gondii is accompanied by stage conversion, in which parasites convert to a slowly dividing bradyzoite that forms cysts in the brain. Interestingly, effector CD8+ T cells in the brain seemed to ignore the intact cysts, but they accumulated and migrated more slowly in the vicinity of isolated parasites, which resembled those seen to emerge from rupturing cysts57 (FIG. 1Ab; Supplementary information S13 (movie)). Activated CD8+ T cells could enter the brains of infected mice independent of their antigen specificity, although antigen-specific T cells preferentially slowed and accumulated near parasites and were retained in the infected tissue for longer periods57. Rather than forming only one-to-one contacts with individual APCs, antigenspecific CD8+ T cells were seen to interact with granuloma-like aggregates of CD11b+ cells, some of which contained visible parasites. Moreover, T cells slowed when in contact with an aggregate but did not undergo further slowing when approaching a parasite within an aggregate, suggesting that the entire granuloma-like structure, rather than an individual infected cell, may be the antigen-presenting unit in this setting. Unlike in L. major-infected skin, effector CD8+ T cells in the brains of T. gondii-infected mice seemed to patrol large areas of the brain, including those that did not contain visible parasites57. Another study revealed T cells migrating along a network of reticular fibres, similar to that found in lymph nodes, that was induced in the brain in response to infection58. This intriguing observation suggests a mechanism to explain how effector T cells could access large regions of the brain parenchyma. It Box 2 | Imaging host–pathogen interactions in zebrafish models Interactions between bacterial pathogens and macrophages can also be visualized in real time in zebrafish embryo infection models63. The zebrafish embryo is transparent, and the entire intact organism can be readily imaged by widefield or confocal microscopy at single cell resolution. This makes it considerably easier to locate regions of interest and to follow the spread of the pathogen over extended periods of time. Adult zebrafish have both an innate and adaptive immune system, with many similarities to the mammalian immune system. The optically accessible embryos have only an innate immune system, but macrophage-like cells can already be observed at the start of blood circulation and have been shown to take up various bacterial pathogens and have an important host protective role64,65,67. So far studies have not only shown that the responses of mammalian and zebrafish immune cell populations to infection are similar but also that factors important for pathogen virulence in mammalian models are similar in zebrafish. For example, infection with streptolysin S-mutant Streptococcus pyogenes led to enhanced neutrophil infiltration in both zebrafish and mouse models18. Perhaps the most important contribution of intravital imaging in these models has been in revealing how bacterial pathogens use macrophages for their dissemination and growth. Zebrafish embryos clear infection with Listeria innocua but not its more pathogenic relative Listeria monocytogenes. A comparison of macrophage behaviour in infected zebrafish revealed that macrophages that had internalized L. innocua lost motility, whereas those that internalized L. monocytogenes remained motile. This suggests a possible role for motile macrophages in spreading infection66. Furthermore, dynamic imaging of nascent granulomas formed in response to Mycobacterium marinum infection revealed greater recruitment of macrophages to granulomas and increased motility of macrophages within granulomas when compared to the response to a strain lacking the RD1 virulence determinant59. This allows arriving macrophages to find and phagocytose infected macrophages, contributing both to early increases in bacterial number and to dissemination59,67. also raises the possibility that the formation of a structure for T cell migration could be a limiting factor for T cell migration within infected tissues in other settings, such as L. major infection in the skin56. The dynamics of the CD8+ T cell response in the brain has also been investigated following intracerebral inoculation with LCMv22. As discussed previously, extravasation of neutrophils and monocytes is associated with vascular leakage and fatal seizures in this model. It has also been known for some time that CD8+ T cells are required for the development of seizures, but their extravasation or positioning was not associated with vascular leakage. Similar to what was observed in chronic T. gondii infection, CD8+ T cells in the brains of LCMvinfected mice made short antigen-dependent contacts, but not the prolonged interactions associated with killing of a target cell22,57. notably, however, marked recruitment of myelomonocytic cells did not occur until after the arrival of T cells in the brain, and depletion of CD8+ T cells resulted in reduced infiltration of monocytes and neutrophils and prevented the development of seizures22. Therefore, chemokines produced by CD8+ T cells or in response to CD8+ T cells might direct the recruitment of neutrophils and monocytes involved in the development of pathology, revealing a new therapeutic target. In the liver. Interactions between effector T cells and aggregates of macrophages are an important feature of mycobacterial infection, and imaging of the liver after infection of mice with BCG revealed key aspects of the dynamic nature of these structures32. Macrophages within BCG-induced granulomas were largely non-motile, but actively extended processes, suggestive of sampling of the local environment. By contrast, polyclonal T cells were highly motile but their migration was restricted within the granuloma by a macrophage-defined border. Although few T cells were observed entering or leaving mature granulomas, this restricted migration was unlikely to be due to a physical barrier, as in vitro-activated T cells could be recruited rapidly and efficiently to mature granulomas. Instead, the authors suggest that macrophages provide a scaffold over which T cells migrate, analogous to reticular fibres in lymph nodes32. Granulomas are diverse and dynamic structures, and there is a great deal more to be learnt from time-lapse imaging, including from studies in non-mammalian species. For example, imaging studies in a zebrafish embryo model of mycobacterial infection showed that nascent granulomas forming in the absence of T cells were highly dynamic structures and actually contributed to the growth and spread of the bacteria59. This difference could reflect either the lack of T cells or the use of a more virulent mycobacterial strain that can use the early granulomatous response to its own benefit. Dynamic imaging in zebrafish infection models is discussed further in BOX 2. Summary and future challenges The complexity of the interaction between pathogens and the host immune system can only begin to be properly understood when studied in the appropriate tissue environment. The studies discussed here have 362 | MAy 2010 | voLUMe 10 www.nature.com/reviews/immunol © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS used various imaging techniques to study this interaction in tissues in real time, revealing some previously unknown or under-appreciated facets of the host–pathogen interaction. Combining these initial observations with genetic manipulation of host or pathogen, as well as with other complimentary experimental approaches, should further our understanding of the delicate balance between host and pathogen. There are several exciting possibilities for future investigation. First, it is hoped that technological advances will allow intravital imaging of previously inaccessible tissue environments, enabling the use of more physiological infection models. Second, tools are being developed that will allow functional information to be derived directly from imaging studies. These include methods for delivering and regulating agents that interfere with biological processes while intravital imaging is taking place, pathogen strains that express fluorescent 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Ji, Y., McLandsborough, L., Kondagunta, A. & Cleary, P. P. C5a peptidase alters clearance and trafficking of group A streptococci by infected mice. Infect. Immun. 64, 503–510 (1996). Courret, N. et al. CD11c- and CD11b-expressing mouse leukocytes transport single Toxoplasma gondii tachyzoites to the brain. Blood 107, 309–316 (2006). Bierly, A. L., Shufesky, W. J., Sukhumavasi, W., Morelli, A. E. & Denkers, E. Y. Dendritic cells expressing plasmacytoid marker PDCA-1 are Trojan horses during Toxoplasma gondii infection. J. Immunol. 181, 8485–8491 (2008). Chtanova, T. et al. Dynamics of T cell, antigenpresenting cell, and pathogen interactions during recall responses in the lymph node. Immunity 31, 342–355 (2009). This paper shows that, following T. gondii infection, memory CD8+ T cells are recruited to the subcapsular sinus where they can become infected and might contribute to pathogen dissemination. Churchward, G. The two faces of Janus: virulence gene regulation by CovR/S in group A streptococci. Mol. Microbiol. 64, 34–41 (2007). Rimoldi, M. et al. Intestinal immune homeostasis is regulated by the crosstalk between epithelial cells and dendritic cells. Nature Immunol. 6, 507–514 (2005). Cahalan, M. D. & Parker, I. Choreography of cell motility and interaction dynamics imaged by twophoton microscopy in lymphoid organs. Annu. Rev. Immunol. 26, 585–626 (2008). Bajenoff, M. et al. Stromal cell networks regulate lymphocyte entry, migration, and territoriality in lymph nodes. Immunity 25, 989–1001 (2006). Katakai, T. et al. A novel reticular stromal structure in lymph node cortex: an immuno-platform for interactions among dendritic cells, T cells and B cells. Int. Immunol. 16, 1133–1142 (2004). Sixt, M. et al. The conduit system transports soluble antigens from the afferent lymph to resident dendritic cells in the T cell area of the lymph node. Immunity 22, 19–29 (2005). Rescigno, M. et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nature Immunol. 2, 361–367 (2001). Niess, J. H. et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science 307, 254–258 (2005). Auffray, C. et al. Monitoring of blood vessels and tissues by a population of monocytes with patrolling behavior. Science 317, 666–670 (2007). This paper describes the constitutive patrolling behaviour of monocytes in blood vessels, which is required for their rapid extravasation in infection. Chieppa, M., Rescigno, M., Huang, A. Y. & Germain, R. N. Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J. Exp. Med. 203, 2841–2852 (2006). reporters controlled by external triggers and fluorescent reporters for immune cell activation or cytokine production. Because many important questions related to interactions between clinically relevant human pathogens and the immune system cannot be adequately addressed in animal models, an important challenge will be to apply what we have learnt from rodent infection models to the study of host–pathogen interactions in humans. This could potentially be achieved using tissue explants or humanized mouse models, although a significant barrier to this approach is being able to identify and track specific human immune cell populations. nevertheless, the use of endogenous signals such as second harmonic generation and tissue autofluorescence (BOX 1), together with advances in our ability to genetically engineer human cells and tissues, might make in situ time-lapse imaging of pathogens in human tissues more accessible in the foreseeable future. 15. Ng, L. G. et al. Migratory dermal dendritic cells act as rapid sensors of protozoan parasites. PLoS Pathog. 4, e1000222 (2008). 16. Boes, M. et al. T-cell engagement of dendritic cells rapidly rearranges MHC class II transport. Nature 418, 983–988 (2002). 17. Nathan, C. Neutrophils and immunity: challenges and opportunities. Nature Rev. Immunol. 6, 173–182 (2006). 18. Lin, A., Loughman, J. A., Zinselmeyer, B. H., Miller, M. J. & Caparon, M. G. Streptolysin S inhibits neutrophil recruitment during the early stages of Streptococcus pyogenes infection. Infect. Immun. 77, 5190–5201 (2009). 19. Gao, J., Gusa, A. A., Scott, J. R. & Churchward, G. Binding of the global response regulator protein CovR to the sag promoter of Streptococcus pyogenes reveals a new mode of CovR–DNA interaction. J. Biol. Chem. 280, 38948–38956 (2005). 20. Miyoshi-Akiyama, T. et al. Cytocidal effect of Streptococcus pyogenes on mouse neutrophils in vivo and the critical role of streptolysin S. J. Infect. Dis. 192, 107–116 (2005). 21. Wedmore, C. V. & Williams, T. J. Control of vascular permeability by polymorphonuclear leukocytes in inflammation. Nature 289, 646–650 (1981). 22. Kim, J. V., Kang, S. S., Dustin, M. L. & McGavern, D. B. Myelomonocytic cell recruitment causes fatal CNS vascular injury during acute viral meningitis. Nature 457, 191–195 (2009). This study involves imaging of the dynamics of the immune response to LCMV in the central nervous system, and it shows that CD8+ T cells are required for the infiltration of myelomonocytic cells that subsequently result in vascular leakage and cause fatal seizures. 23. Chtanova, T. et al. Dynamics of neutrophil migration in lymph nodes during infection. Immunity 29, 487–496 (2008). 24. Peters, N. C. et al. In vivo imaging reveals an essential role for neutrophils in leishmaniasis transmitted by sand flies. Science 321, 970–974 (2008). This paper reveals the dynamics of the neutrophil response to L. major infection in the skin and describes how L. major could exploit this response to establish infection. 25. Peters, N. C. et al. Vector transmission of leishmania abrogates vaccine-induced protective immunity. PLoS Pathog. 5, e1000484 (2009). 26. Amino, R. et al. Host cell traversal is important for progression of the malaria parasite through the dermis to the liver. Cell Host Microbe 3, 88–96 (2008). 27. Amino, R. et al. Quantitative imaging of Plasmodium transmission from mosquito to mammal. Nature Med. 12, 220–224 (2006). 28. Vanderberg, J. P. & Frevert, U. Intravital microscopy demonstrating antibody-mediated immobilisation of Plasmodium berghei sporozoites injected into skin by mosquitoes. Int. J. Parasitol. 34, 991–996 (2004). nATURe RevIewS | Immunology 29. Frevert, U. et al. Intravital observation of Plasmodium berghei sporozoite infection of the liver. PLoS Biol. 3, e192 (2005). 30. Frevert, U., Usynin, I., Baer, K. & Klotz, C. Nomadic or sessile: can Kupffer cells function as portals for malaria sporozoites to the liver? Cell. Microbiol. 8, 1537–1546 (2006). 31. Baer, K. et al. Kupffer cells are obligatory for Plasmodium yoelii sporozoite infection of the liver. Cell. Microbiol. 9, 397–412 (2007). 32. Egen, J. G. et al. Macrophage and T cell dynamics during the development and disintegration of mycobacterial granulomas. Immunity 28, 271–284 (2008). This paper describes the migration of T cells and macrophages during the development of mycobacterial granulomas. 33. Baer, K., Klotz, C., Kappe, S. H., Schnieder, T. & Frevert, U. Release of hepatic Plasmodium yoelii merozoites into the pulmonary microvasculature. PLoS Pathog. 3, e171 (2007). 34. Sturm, A. et al. Manipulation of host hepatocytes by the malaria parasite for delivery into liver sinusoids. Science 313, 1287–1290 (2006). This study carried out imaging of the budding of merosomes from Plasmodium spp.-infected hepatocytes into liver sinusoids and reveals a mechanism through which the merosomes might avoid phagocytosis. 35. Tarun, A. S. et al. Quantitative isolation and in vivo imaging of malaria parasite liver stages. Int. J. Parasitol. 36, 1283–1293 (2006). 36. Phan, T. G., Green, J. A., Gray, E. E., Xu, Y. & Cyster, J. G. Immune complex relay by subcapsular sinus macrophages and noncognate B cells drives antibody affinity maturation. Nature Immunol. 10, 786–793 (2009). 37. Phan, T. G., Grigorova, I., Okada, T. & Cyster, J. G. Subcapsular encounter and complement-dependent transport of immune complexes by lymph node B cells. Nature Immunol. 8, 992–1000 (2007). 38. Carrasco, Y. R. & Batista, F. D. B cells acquire particulate antigen in a macrophage-rich area at the boundary between the follicle and the subcapsular sinus of the lymph node. Immunity 27, 160–171 (2007). 39. Junt, T. et al. Subcapsular sinus macrophages in lymph nodes clear lymph-borne viruses and present them to antiviral B cells. Nature 450, 110–114 (2007). This paper describes the role of subcapsular sinus macrophages in capturing viral particles and presenting them to migrating B cells. 40. Hickman, H. D. et al. Direct priming of antiviral CD8+ T cells in the peripheral interfollicular region of lymph nodes. Nature Immunol. 9, 155–165 (2008). 41. Bajenoff, M. et al. Natural killer cell behavior in lymph nodes revealed by static and real-time imaging. J. Exp. Med. 203, 619–631 (2006). 42. Sayles, P. C. & Johnson, L. L. Exacerbation of toxoplasmosis in neutrophil-depleted mice. Nature Immunol. 15, 249–258 (1996). voLUMe 10 | MAy 2010 | 363 © 2010 Macmillan Publishers Limited. All rights reserved REVIEWS 43. Egan, C. E., Sukhumavasi, W., Bierly, A. L. & Denkers, E. Y. Understanding the multiple functions of Gr-1+ cell subpopulations during microbial infection. Immunol. Res. 40, 35–48 (2008). 44. Fernandez, N. C. et al. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate antitumor immune responses in vivo. Nature Med. 5, 405–411 (1999). 45. Borg, C. et al. NK cell activation by dendritic cells (DCs) requires the formation of a synapse leading to IL-12 polarization in DCs. Blood 104, 3267–3275 (2004). 46. Brilot, F., Strowig, T., Roberts, S. M., Arrey, F. & Munz, C. NK cell survival mediated through the regulatory synapse with human DCs requires IL-15Rα. J. Clin. Invest. 117, 3316–3329 (2007). 47. Kang, S. J., Liang, H. E., Reizis, B. & Locksley, R. M. Regulation of hierarchical clustering and activation of innate immune cells by dendritic cells. Immunity 29, 819–833 (2008). 48. Beuneu, H. et al. Dynamic behavior of NK cells during activation in lymph nodes. Blood 114, 3227–3234 (2009). 49. Garrod, K. R., Wei, S. H., Parker, I. & Cahalan, M. D. Natural killer cells actively patrol peripheral lymph nodes forming stable conjugates to eliminate MHCmismatched targets. Proc. Natl Acad. Sci. USA 104, 12081–12086 (2007). 50. Cavanagh, L. L. & Weninger, W. Dendritic cell behaviour in vivo: lessons learned from intravital twophoton microscopy. Immunol. Cell Biol. 86, 428–438 (2008). 51. John, B. et al. Dynamic imaging of CD8+ T cells and dendritic cells during infection with Toxoplasma gondii. PLoS Pathog. 5, e1000505 (2009). 52. Millington, O. R., Di Lorenzo, C., Phillips, R. S., Garside, P. & Brewer, J. M. Suppression of adaptive immunity to heterologous antigens during Plasmodium infection through hemozoin-induced failure of dendritic cell function. J. Biol. 5, 5 (2006). 53. Millington, O. R. et al. Malaria impairs T cell clustering and immune priming despite normal signal 1 from dendritic cells. PLoS Pathog. 3, 1380–1387 (2007). 54. Tadokoro, C. E. et al. Regulatory T cells inhibit stable contacts between CD4+ T cells and dendritic cells in vivo. J. Exp. Med. 203, 505–511 (2006). 55. Tang, Q. et al. Visualizing regulatory T cell control of autoimmune responses in nonobese diabetic mice. Nature Immunol. 7, 83–92 (2006). 56. Filipe-Santos, O. et al. A dynamic map of antigen recognition by CD4 T cells at the site of Leishmania major infection. Cell Host Microbe 6, 23–33 (2009). This paper describes the dynamics of the CD4+ T cell response to L. major infection in the skin, revealing differences in the ability of infected cells to engage with CD4+ T cells. 57. Schaeffer, M. et al. Dynamic imaging of T cell-parasite interactions in the brains of mice chronically infected with Toxoplasma gondii. J. Immunol. 182, 6379–6393 (2009). This paper shows that CD8+ T cells in the brain interact with granuloma-like structures associated with parasites but ignore intact parasite-containing cysts. 58. Wilson, E. H. et al. Behavior of parasite-specific effector CD8+ T cells in the brain and visualization of a kinesis-associated system of reticular fibers. Immunity 30, 300–311 (2009). This paper shows that CD8+ T cells migrate along a reticular system of fibres formed in response to T. gondii infection in the brain. 59. Davis, J. M. & Ramakrishnan, L. The role of the granuloma in expansion and dissemination of early tuberculous infection. Cell 136, 37–49 (2009). This paper uses a zebrafish embryo infection model to visualize the formation of mycobacterial granulomas and describes a role for the granuloma in bacterial growth and spread. 60. Lindquist, R. L. et al. Visualizing dendritic cell networks in vivo. Nature Immunol. 5, 1243–1250 (2004). 61. Faust, N., Varas, F., Kelly, L. M., Heck, S. & Graf, T. Insertion of enhanced green fluorescent protein into the lysozyme gene creates mice with green fluorescent granulocytes and macrophages. Blood 96, 719–726 (2000). 62. Jung, S. et al. Analysis of fractalkine receptor CX3CR1 function by targeted deletion and green fluorescent protein reporter gene insertion. Mol. Cell. Biol. 20, 4106–4114 (2000). 63. Davis, J. M. et al. Real-time visualization of mycobacterium-macrophage interactions leading to initiation of granuloma formation in zebrafish embryos. Immunity 17, 693–702 (2002). 64. Herbomel, P., Thisse, B. & Thisse, C. Ontogeny and behaviour of early macrophages in the zebrafish embryo. Development 126, 3735–3745 (1999). 65. Prajsnar, T. K., Cunliffe, V. T., Foster, S. J. & Renshaw, S. A. A novel vertebrate model of Staphylococcus aureus infection reveals phagocytedependent resistance of zebrafish to non-host specialized pathogens. Cell. Microbiol. 10, 2312–2325 (2008). 66. Levraud, J. P. et al. Real-time observation of Listeria monocytogenes-phagocyte interactions in living zebrafish larvae. Infect. Immun. 77, 3651–3660 (2009). 67. Davis, J. M., Haake, D. A. & Ramakrishnan, L. Leptospira interrogans stably infects zebrafish embryos, altering phagocyte behavior and homing to specific tissues. PLoS Negl. Trop. Dis. 3, e463 (2009). 68. Halle, S. et al. Induced bronchus-associated lymphoid tissue serves as a general priming site for T cells and 364 | MAy 2010 | voLUMe 10 69. 70. 71. 72. 73. 74. 75. 76. is maintained by dendritic cells. J. Exp. Med. 206, 2593–2601 (2009). Ortolano, F. et al. Imaging T-cell movement in the brain during experimental cerebral malaria. Parasite Immunol. 31, 147–150 (2009). Aoshi, T. et al. Bacterial entry to the splenic white pulp initiates antigen presentation to CD8+ T cells. Immunity 29, 476–486 (2008). Graham, D. B. et al. ITAM signaling by Vav family Rho guanine nucleotide exchange factors regulates interstitial transit rates of neutrophils in vivo. PLoS ONE 4, e4652 (2009). Melican, K. et al. Bacterial infection-mediated mucosal signalling induces local renal ischaemia as a defence against sepsis. Cell. Microbiol. 10, 1987–1998 (2008). Laschke, M. W., Kerdudou, S., Herrmann, M. & Menger, M. D. Intravital fluorescence microscopy: a novel tool for the study of the interaction of Staphylococcus aureus with the microvascular endothelium in vivo. J. Infect. Dis. 191, 435–443 (2005). Norman, M. U. et al. Molecular mechanisms involved in vascular interactions of the Lyme disease pathogen in a living host. PLoS Pathog. 4, e1000169 (2008). Moriarty, T. J. et al. Real-time high resolution 3D imaging of the lyme disease spirochete adhering to and escaping from the vasculature of a living host. PLoS Pathog. 4, e1000090 (2008). Shin, S. C., Vanderberg, J. P. & Terzakis, J. A. Direct infection of hepatocytes by sporozoites of Plasmodium berghei. J. Protozool. 29, 448–54 (1982). Acknowledgements We thank J. Halkias for helpful comments. This work was supported by US National Institutes of Health grants AI065537 and AI065831 (E.A.R.). J.L.C. is a Sir Henry Wellcome Postdoctoral Fellow (Wellcome Trust grant: WT085494MA). Competing interests statement The authors declare no competing financial interests. DATABASES UniProtKB: http://www.uniprot.org CD11c | CD169 | CX3CR1 FURTHER INFORMATION Ellen A. Robey’s homepage: http://mcb.berkeley.edu/labs/robey/ SUPPLEMENTARY INFORMATION See online article: S1 (movie) | S2 (movie) | S3 (movie) | S4 (movie) | S5 (movie) | S6 (movie) | S7 (movie) | S8 (movie) | S9 (movie) | S10 (movie) | S11 (movie) | S12 (movie) | S13 (movie) All lInks ARE ActIvE In thE onlInE PDf www.nature.com/reviews/immunol © 2010 Macmillan Publishers Limited. All rights reserved