* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 17 - Angelfire
Gynecomastia wikipedia , lookup
Metabolic syndrome wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Hypothyroidism wikipedia , lookup
Hypothalamus wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Pituitary apoplexy wikipedia , lookup
Hyperthyroidism wikipedia , lookup
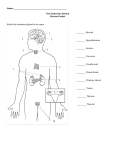
Chapter 17 Endocrine Pathophysiology ●Key Points of Normal Endocrine Physiology -Delivery of secretions-Endocrine vs. Exocrine Glands -Figure 17.1, p. 447 -Endocrine system: consists of ductless glands whose secretions (hormones) are delivered to their sites of action by ducts. -Exocrine system: secretions are delivered to their sites of action by ducts. -Neuroendocrine Control -Figure 17.2, p. 448 -Hypothalamus- complex process -Process as follows: hypothalamus, releasing hormone, anterior pituitary, tropic hormone, target gland, hormone, target tissue, response. -Tissue Specificity -Vary: can either have hormones bind to their surface receptors, or intracellular receptors that form complexes that enter the nucleus -Target tissues alter their activity in response to a particular hormone. -Increased specificity- only responds to a particular hormone -(sex hormone) -“Dose-Related” response -more hormone binding leads to more target tissue response, & vice versa -Hormone clearance from blood -Figure 17.6, p. 451 -With greater binding frequency there is increased cellular response, and vice versa. The frequency of receptor binding is in turn dependent on the amount of hormone delivered by blood. -Inactivation of hormones usually occurs at 2 sites: 1) Target Tissues: enzymes degrade hormones and convert them to nonfunctional forms. 2) Liver: hormones reaching the liver are chemically converted to inactive forms by hepatic enzymes systems, a process related to the liver’s detox functions. -Hormones are also cleared from the blood by the kidney. They are excreted in urine. -Constantly dynamic in kidney and liver ●Endocrine Dysfunction -Two primary types of problem- excessive or inadequate target tissue response -Exaggerated target tissue responses: hypersecretion of hormone is most often at fault. When target tissue responses are deficient, either endocrine hyposecretion is the cause or there is a defect in the tissues response to normal levels of hormone. -Type II diabetes: look at tissue response -Hypothalamus and pituitary: negative feedback -Endocrine Hypofunction -absent/inadequate development (agenesis) -abnormal hormone production -also infarction, infection, tumor, atrophy, autoimmune mechanisms, chronic inflammation, surgery for hypersecretion -Absent or Inadequate Production -can have increased hormone levels because no feedback from tissue -Ex: Type II diabetes -Hormone resistance: insensitivity of a target tissue to its hormone. Other genetic defects, immune system, or fatigue factors may be the cause -Endocrine Hyperfunction -Hypersecretion -Hard medically to turn it down (Thyroid Problems) -Circulating hormone is present at levels that are inappropriately high. May arise when an endocrine gland is exposed to unusually high levels of its tropic hormone. Defective feedback control may be a factor in endocrine hypersecretion. Tumors of endocrine glands may produce hyperfunction states if the neoplastic tissue retains the ability to secrete functional hormone. ●Thyroid Problems -Principle effects of Thyroid Hormone -Table 17.1, p. 456 -increased aerobic energy -glucose/lipid protein metabolism -promoting protein, carbohydrate, and lipid utilization -Etiology of Thyroid Hypofunction -Figure 17.15, p. 459 -small size from surgery or radiation therapy, producing decreased amount/form of hormone -Bacterial or Viral infections, trauma, thyroiditis -autoimmune diseases (destruction) (Hashimoto’s Thyroiditis) -pregnancy and puberty can affect the thyroid. -Clinical effects of Thyroid Hypofunction in Adults -Table 17.2, p. 457 -gradual onset -weakness, fatigue, cold intolerance, lassitude, weight gain, decreased ventilation, constipation, bradycardia, hypotension, anemia, dry skin/hair, memory loss, drowsiness, apathy, water retention, non-pitting edema (myxedema), husky voice, atherosclerosis, decreased Vitamin A synthesis. -Clinical Effects of Thyroid Hypofunction in Infants and Children -Table 17.3, p. 457 -Cretin: a child who has thyroid hypofunction (normal growth and tissue differentiation are impaired) Called Cretinism -Obesity is typical, thick tongue, tooth and hair development is faulty, brain development suffers and mental retardation, emotional derangements -Myxedema, sexual immaturity, delayed skeletal maturation, short stature, increased subcutaneous tissue, slow growth, goiter. -Therapy for Hypothyroid -Provide thyroid hormone -Clinical Effects of Thyroid Hyperfunction -Table 17.4, p. 460 -hyperthyroidism: exaggerated target tissue responses -Muscle wasting, increased activity, heat intolerance, weight loss, diarrhea, vomiting, nausea, insomnia, hyperventilation, heart failure, CNS increases, nervousness, tachycardia, hypertension, rapid speech, emotional instability, irritability, tremor of limbs, exophthalmos, toxic goiter, cardiac dysrhythmias, vasodilation, -Graves’ Disease -occurs mostly in young females -enlarged thyroid disease. (2-3x than normal) -overreacting to Thyroid Stimulating Hormone (excessive thyroid) -result is a toxic goiter condition in spite of normal or very low TSH levels. -toxic goiter: initially undersecreting goiter develops regions of tissue that hypersecrete and don’t respond to lowered TSH levels. -Weight loss, hyperactivity and other symptoms occur. -Thyroid Storm -excessive released in plasma -massive increase in the level of thyroid hormones -dramatic increase in system that exacerbates the symptoms of a preexisting hyperthyroid state. -abrupt rise in body temp: hyperpyrexia (causes delirium and convulsions.) -Cardiac Arrhythmia, hypovolemia, cardiovascular shock, death -Therapy for Hyperthyroid -can’t take it out, so reduce size of tissue, radioactive iodine -direct radiation, partial thyroidectomy/surgical removal (becomes hypothyroid, parts inflame and cause parathyroid problems and calcium is affected) -can use drugs that suppress T3 and T4 synthesis. ●Diabetes Mellitus- Focus on Endocrine Function of Pancreas -Insulin- beta islet cells -Glucoagon- alpha islet cells -responds to low glucose level -most common endocrine disorder- is life threatening ●Type I DM (Insulin Dependent Diabetes Mellitus- IDDM, Juvenile Onset DM) -Only 10% of all diabetics -Sudden auto-immune destruction of beta cells (beta cell infection; possibly from environmental chemicals or therapeutic drugs) -sudden loss of weight (body can’t use it), breath smells, they get very sick, very quickly. -Evidence of a genetic predisposition -Glucose disorder and effects -Diabetic Keto-acidosis -Life-threatening (toxic to brain tissue) -Hypoglycemic Coma- result of brain glucose deprivation -caused by inadequate dietary intake, high glucose utilization (either by exercise or from an accidental excessive insulin dose) -Figure 17.19, p. 465 -Therapy for Type I DM -close regulation of Insulin- insulin therapy is always required. The aim is restoration of glucose metabolism, so that its dietary intake must be closely regulated and matched to insulin dose. -Challenges for close regulation of glucose -Long-term effects of Hyperglycemia -lack of insulin secretion is an increase in blood glucose, called hyperglycemia -vascular problems (atherosclerotic) -arterial insufficiency (ulcers, stroke) -decrease in healing- gangrene, kidney damage ●Type II DM (Type II DM, Non-Insulin Dependent DM- NIDDM, Adult Onset DM) -Insulin resistance (inability of cells to take up and metabolize glucose) -90% of diabetics, slow onset, tissue insensitivity and beta-cell hypersecretion -late middle age, normally has it for 10 years and doesn’t know it -are usually being treated for the effects of the disease and not the disease itself) -Normal amounts, less sensitive tissues (beta cells slowly lose their capacity to produce insulin, but target tissues also show reduced sensitivity to it) -probably genetic -Association with obesity and sedentary lifestyle -both increase the risk for developing Type II DM -people who are obese have fewer insulin receptors. -Native Americans- gain weight in times of plenty -Control of Type II DM -Hypoglycemic Medications -Mechanism of Action of Non-Insulin Hypoglycemics -stimulate islet cells, delay carbs in gut, etc (?) -Diet Control -loss of 5% of body weight increases benefits (15% is ideal) -Exercise Increase -Effects of Hypoglycemia -too much insulin, too little glucose -more threatening than hyperglycemia (because it’s long term) -Treatment of Hypoglycemia -oral glucose ●Adrenal Glands -The adrenal glands produce hormones that enable us to better cope with the changing environment. It is involved in the maintenance of body fluid balance and blood glucose level, as well as various cardiovascular responses. -stress response: increase protein synthesis -General Adaptation Syndrome -Figure 17.27, p. 474 -Surge in cortisol from stressors (trauma, intense exercise, severe disease/infection, temp extremes, pain, emotional distress, severe hemorrhage. -Effect is to supply cells with increased cellular fuels (glucose, lipid), increased protein synthesis components (AA) and increased oxygen as a result of higher resp rates, and to increase blood flow to deliver all of them more efficiently. -Has an alarm phase, resistance phase, and an exhaustion phase -Adrenal Hormone Stimulus -Table 17.10, p. 473 -Adrenal Hypersecretion- Cushing’s Syndrome -glucocorticoid hypersecretion -obese, moon face, chronic protein catabolism produces muscle weakness, bone loss, bruising and striae, hypertension and hypokalemia, insulin insensitivity and impaired glucose tolerance. Can produce menstrual dysfunctions and some male-pattern hair growth and acne. -Table 17.11, p. 475 (photos too) -cause? Hypersecretion and adrenal tumors, elevated plasma, excessive ACTH output of a pituitary adenoma or a hypothalamic tumor. -Role of steroid therapy for other illnesses and Cushing-like Response -Adrenal Hyposecretion- Addison’s Disease -have less steroids than they need (inadequate corticosteroids) -may be due to destruction of the adrenal cortex or to suppression of ACTH by high therapeutic doses of glucocorticoids. -President Kennedy- rare- caused by a congenital enzyme deficiency -other causes: in most cases, destruction of the gland occurs by a poorly understood autoimmune mechanism, but infection, tumor invasion, or infarction -slowly developing weakness and fatigue, appetite and weight loss, and characteristic pigmentation excess -Addisonian Crisis -highly vulnerable to stress -nausea, hyponatremia, hypovolemia, circulatory shock, fever, hyperkalemia, hypotension, and dehydration. ●Parathyroid Disorders -Calcium Homeostasis -Figure 17.29, p. 476 -renal phosphate loss, calcium retention -Hyperparathyroid Problems -usually the result of a benign or malignant tumor or of parathyroid hyperplasia -more often in females than males and primarily produce loss of bone tissue -resulting bone weakness predisposes to bone pain, deformity, and fracture -hypercalcemia- produces a range of muscular and neurologic defects and kidney stone formation. -Hypoparathyroid Problems -autoimmune distruction- involved in a lack of PTH output. -genetic condition in which the kidney is insensitive to PTH produces low calcium levels and is known as pseudohypoparathyroidism. ●Pituitary Gland -Principal hormones of pituitary gland and effects -Table 17.12, p. 478 -Pituitary Hypersecretion -may be caused by a tropic-hormone-secreting adenoma -if in childhood, prior to closure of epiphyseal plates, rapid overall body growth is promoted by exaggerated stimulus to growth. Results in giantism -when it occurs after adolescence, acromegaly develops -although long bone length is fixed, bones enlarge by thickening- excessive growth of soft tissue- produces a characteristic enlarging and coarsening of the features. Internal organs (liver and kidneys are also affected) -Pituitary Hyposecretion -may be the result of infection, primary or metastatic tumor damage, infarction, or other injuries. In tumors, various consequences of brain compression r invasion of the brain may be superimposed on endocrine hypofunction (headache, visual disturbances) -congenital or hereditary defects may produce hyposecretion of only a single anterior pituitary hormone. -Diabetes Insipidus -Syndrome of Inappropriate Anti-Diuretic Hormone Secretion (SIADH) -lose more than 20L/day of fluid -some end up water intoxicated ●Key Concepts 1) Endocrine disease is most often the result of excessive or inadequate hormone secretion, due to an imbalance in the gland’s controlling inputs or to damage to the gland itself. 2) Endocrine hyposecretion may be the result of a metabolic defect, gland agenesis, atrophy of a developed gland, or damage to an otherwise normal gland by infection, infarction, autoimmune mechanisms, or tumor growth. 3) In response to endocrine hyposecretion, negative feedback reflexes produce increased levels of tropic hormones or hypothalamic releasing hormones, whose suppression may be monitored to confirm restoration of normal function. 4) Hormone resistance involves a reduction of hormone receptors, which produces target tissue insensitivity and hyposecretion effects. 5) Endocrine hypersecretion is the result of excessive secretion of tropic hormones, defective feedback control mechanisms, or endocrine gland tumors 6) Thyroid hypofunction produces a systemic decline in the metabolic rate, causing cold intolerance, weight gain, and sluggish muscular and neurologic activity. 7) Chronically low plasma levels of thyroxine promote increased secretion of TSH, which induces the condition of thyroid hyperplasia known as goiter 8) Thyroid hyperfunction produces a systemic elevation of the metabolic rate, causing heat intolerance, neurologic excitability, insomnia, weight loss, cardiac effects, and exophthalmos 9) Diabetes mellitus exists in two forms: IDDM, the true islet hypofunction disease, and NIDDM, which involves defective secretion and insulin resistance. 10) A variety of chronic effects in DM involve small and large blood vessels and the nervous system, producing numerous and serious long-term consequences for the person with diabetes 11) A range of adaptive responses to stress are mediated by the adrenal cortex and medulla, grouped under the title general adaptation syndrome 12) Adrenocorticotropic hypersecretion may involve glucocorticoids, producing Cushing’s syndrome, aldosterone, to yield hyperaldosteronism, or androgens in women, causing adrenal virilism. 13) The principal adrenocortical hyposecretion state involves a deficit of the corticosteroids, producing Addison’s disease, which may compromise the GAS response 14) Hyperparathyroidism, which is usually caused by a parathyroid tumor, produces high levels of bone resorption, to the degree of compromising skeletal integrity 15) The numerous hormones of the adenohypophysis may be individually hypersecreted by an adenoma of a specific pituitary cell type, limiting effects to the target tissue regulated by each hormone. 16) Hypersecretion of growth hormone prior to closure of the epiphyseal plates can so stimulate growth that body height might attain 8-9 ft, while hypersecretion after closure results in the enlargement and thickening of various tissues without any increase in height. 17) Hyposecretion of adenohypophyseal hormones is usually due to tissue damage that affects all cell types to produce more widespread and variable systemic hypofunction effects. 18) In the neurohypophysis, disturbances of oxytocin secretion are unknown but ADH secretion may be excessive, causing SIADH, or inadequate, causing diabetes insipidus.