* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download L04 Pathophysiology Inflammastion
Adaptive immune system wikipedia , lookup
Immune system wikipedia , lookup
Periodontal disease wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Atherosclerosis wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
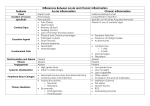
L04 Pathophysiology/inflammation : Done by : Marwa Al-gharabat Chronic inflammation: Definition: is inflammation of prolonged duration (weeks or months) in which inflammation, tissue injury, and attempts at repair coexist, in varying combinations. The key sentences in the definition “at the same time we have tissue injury without healing attempt at repair ,and the repair lead to consequence in varying combination “ . varying combination mean that →for example “ we have 80% healing and 20% injury OR 10% healing and 90% injury “ The healing it’s self can be replacement with the same tissue or with different type of tissue which lead to fibrosis or angiogenesis or infiltration with (monocyte ,…… etc ) in varying combination “in different percentage “ depending on injury it’s self and other tissue. Causing of chronic inflammation : 1-Persistent infections by microorganisms that are difficult to eradicate: An example of viral infection that is likely to be a chronic inflammation →hepatitis type C , or type B . but more likely in type C .( now we have 6 type of viral hepatitis , 5 type type was established and one type had been just discovered year a go ) 2-Immune-mediated inflammatory diseases: and there is a large number of examples : auto immune disease ,inflammatory bowel disease ,Paget disease . 1 3-Prolonged exposure to potentially toxic agents, either exogenous or endogenous : Example of endogenous → urea and nitrogen waste product . Example of prolonged exposure to a exogenous toxic agent is cigarette smoking that result in inflammation of the respiratory tract → structural changes →lead to varying condition include COPD “chronic obstructive pulmonary tract “ Lung cancer is a result from inflammation that occur from cigarette smoking which lead eventually transformation of cells ,and cells become malignant cell . Consequences of defective or excessive inflammation : •Defective inflammation results in: - increased susceptibility to infections: the immune system can become weak due to condition disease like (HIV,AIDS )or chronic depilating disease like CKD Immune system will become weak because production not only RBCs but leukocyte will be effected eventually as a result from some medication like (immune repressive medication ) Defective inflammation whatever the cause is expected to lead to ↑ susceptibility to infection and to - delay the wound healing , for example : diabetic patient have long standing disease and it’s uncontrolled ,there coagulation cascade is closely related to inflammatory response so if we have : Weak inflammatory response → weak and not effective coagulation → pain sensation can be effected too ) →) مثال مريض السكري ممكن ينجرح من دون ما يشعر انو انجرحdiabetic foot →sometime lead to amputation . 2 Excessive inflammation is: Most of them under allergic and inflammatory condition . in new born most of them has some condition that indicate excessive inflammation such as eczema “ atopic dermatitis “ we have 3 conditions that are closely related and they share similar pathophysiolog : 1-topic dermatitis 2-allergic rhinitis (seasonal allergy ) 3-asthma Some baby start with eczema and then he will have seasonal allergy then asthma مش شرط نفس الترتيب MORPHOLOGIC FEATURES : If we talk about biopsy of the inflamed tissue ,what is the changes that observed under microscope ? “ morphologic changes - Infiltration with mononuclear cells, which include macrophages, lymphocytes, and plasma cells: Plasma cell is a mature B lymphocyte , the difference between them that plasma cell can produce anti-body . We have many type of T lymphocyte , in asthma we have 2 type : * TH l and TH ll . -Tissue destruction, induced by the persistent offending agent or by the inflammatory cells :the leukocyte them self can be damaged by different mechanism : 1-cell death induced by cytokines released by leukocyte 2-non-specific damage that happen as a result of oxidative stress 3 *in leukocyte in order to fight the microbes “ we have more than way if killing “ ,by free oxygen or nitrogen radicals , thes free radicals are very damaging to the surrounding macromolecule and cells , where ever we have electrons rich site it ‘s exposed to attach by these radicals so protein ,cytoskeleton ,nucleus all of these will be effected -Attempts at healing by connective tissue replacement of damaged tissue, accomplished by proliferation of small blood vessels (angiogenesis) and, in particular, fibrosis Role of Macrophages •The macrophage is the dominant cellular player in chronic inflammation (predominates within 48 hrs). . In acute inflammation the dominant players cell is neutrophils , if it was an inflammatory allergic reaction (mast cell ,acenocell , play a significant role in addition to neutrophils ) In chronic inflammation we are talking mostly about macrophages (the dominant player ) but also neutrophils •Macrophages are one component of the mononuclear phagocyte system. Phagocytosis →engulfment of cellular debris , exogenous or endogenous potential threat to the body and microbes ,then they lysed or destroyed inside the macrophages to prevent the free radicals from getting out to nucleophilic center in the surrounding tissue This is a typical scenario, some infection does not go through this scenario such as TB ; in TB after they engulfed by macrophages they can not be destroyed . Another example , in CVD if cholesterol (LDL) ↑ in blood the body try to get rid off it , the only way physiologically to remove it would be by binding of LDL particles to LDL receptor . 4 If there was : down regulation or deficiency of LDL receptor or ↑ in LDL particles more than the receptor → excess amount LDL cholesterol now the body try to get rid off it by decomposition in subendothelial layer followed by oxidation , in addition to cholesterol we have triglyceride but the nucleus of cholesterol can not be destroyed by the body ,it can be modified , the body convert it to another thing unlike triglyceride . Net effect that we will have oxidized lipid and free radicals that damage the surrounding tissue , recruitment for the macrophages , macrophages engulf the oxidized lipid but it can not get rid off the cholesterol in this condition foam cell form →formation of atherosclerosis region •The half-life of blood monocytes is about 1 day, whereas the life span of tissue macrophages is several months or years Unlike the neutrophils , when the neutrophilis get out from the blood life spam become shorter ,but when the macrophages leave the blood →it’s life spam will ↑, why ? Due to properties which is that macrophages can differentiate into other type of cells, For example osteoclast in bone that is responsible of bone absorption ,these are macrophages. In inflammatory condition →↑the risk of tuberosis , why ? Due to activation of osteoclast in condition of inflammation (macrophages ) النهم باالصل They will be affected by several type of inflammatory mediator , so as : Look at figure in slide 34. •Macrophages may be activated by a variety of stimuli: - microbial products that engage TLRs and other cellular receptors TLRs this is a big family or receptor they are involved in several condition 5 - cytokines (e.g., IFN-γ)→interferons ᵧ secreted by sensitized T lymphocytes and by natural killer cells. *The products of activated macrophages serve to: Macrophages can be activated by several cytokines or microbial product that would activate certain receptors on the macrophages →activation of macrophages →the effect is : - eliminate injurious agents such as microbes - initiate the process of repair - responsible for much of the tissue injury in chronic inflammation, excessive activation →damage for tissue Look at figure in slide 36 . IL-4 and IFN-ᵧ are signifecant . Other cells in chronic inflammation •lymphocytes of different types (T and B cells). •Plasma cells. •Eosinophils are abundant in immune reactions mediated by IgE and in parasitic infections. IgE “ immune globulin “ involved in mostly allergic reaction and parasitic reaction “ •Mast cells. IgE → activate several type of leukocyte “ eosinophilis mostly “ , basophil and mast cell. if eosinophilis release the IgE then what would be the control mechanism to stop the production of IgE ?? ** eosinophilis do not produce the IgE ,it produced by plasma cell *** as macrophages activated by cytokines they can by them self produce cytokines that affect other leukocyte , for example activated macrophages can release IL-1 and INF ᵨ and also it can be activated by other type of cytokines such as IL-1 and INF . 6 **Mediators of inflammation •Mediators are generated either from cells or from plasma proteins. Plasma protein not plasma cell , what is the plasma ? Plasma = blood – cells and platelets , it’s contain protein and electrolyte ,some of the plasma protein is a inflammatory mediator. Inflammatory mediator are released from: →WBCs “leukocyte “ . → plasma , produced by: -non-leukocyte cell e.x : adipose tissue release adipokines which release into plasma →reach to another site → shifting the balance to the proinflammatory side . OR : -Plasma protein that is anti-inflammatory . •Active mediators are produced in response to various stimuli •One mediator can stimulate the release of other mediators IFN-ᵧ activate macrophages then it produce another cytokines such as INF,IL-1 and other . •Mediators vary in their range of cellular targets ,some of them are specific and some of them have wide spectrum of target . •Once activated and released from the cell, most of these mediators are short-lived, to prevent excessive tissue damage . 7 Prostaglandins (PGE2)produced by cyclooxiginaze pathway Two enzyme are involved in expressed inflammation : -COX2 →↑prostaglandins -INOS→ inducible nitric oxide synthesis →↑ NO *inflammation could be localized and it could be/ systemic → systemic effect : •Fever •Acute-phase proteins synthesis •Leukocytosis Leukopenia →decrease at WBCs numbers Leukocytosis → increase at WBCs numbers Cuz WBCs mostly neutrophilis type ,so when we say leukopenia most of the time mean ↓at neutrophilis Neutrophilia :↑ in eutrophilis *leukopenia most common in cancer patient with chemotherapy treatment , because it one of the common side effect of chemotherapy •Miscellaneous ALL of these effects are tested in the lab , if they were ↑ so there is an inflammation . But they are not specific for a particular disease , for example if C reactive protein was ↑ so there is an inflammation due to infection . 8 If the inflammation was localized , there will be no systemic manifestation , for example : In oscteoarthritis ; the inflammation is in a certain joint so if we take blood sample ,the acute phase reactant for example will not be elevated /no fever /because it’s localized inflammation . But this condition will be associated with viral infection or bacterial infection and these infection are associated with fever . Good luck 9