* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Hormone synthesis and degradation
Survey
Document related concepts
Transcript
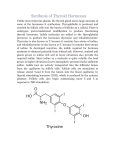
Hormone synthesis and degradation Chemistry of hormones • Steroids • Small molecules - NO • Amino acids derivates Receptor inside the cell – Thyroid hormones – Catecholamines • Proteins and peptides • FA derivates - eicosanoids Surface recceptors Steroid hormones • They are produced in cytoplasm from the cholesterol, beginning and end phases are located in the mitochondria • They can not be stored (they are produced de novo after signal) • Transport proteins bind them in the plasma SHBG, CBG, Albumin • Cytosolic receptors • After the receptor binding – Binding of hormone – receptor comlex to DNA – transcription (mRNA production) Steroid hormones Steroid synthesis • Steroid hormones are synthesized from cholesterol. • Cholesterol is mostly derived from plasma, but a small portion is synthesized in situ from acetyl-CoA. • Upon stimulation (e.g. by ACTH), free cholesterol is transported into the mitochondria, where a cytochrome P450 side chain cleavage enzyme (P450scc) converts cholesterol to pregnenolone. Side chain cleavage (removal of the six-carbon fragment) gives the 21-carbon steroid. • An ACTH-dependent steroidogenic acute regulatory (StAR) protein is essential for the transport of cholesterol to P450scc in the inner mitochondrial membrane. Steroid synthesis • All mammalian steroid hormones are formed from cholesterol via pregnenolone through a series of reactions that occur in either the mitochondria or endoplasmic reticulum of the producing cell. • Hydroxylases that require molecular oxygen and NADPH are essential, and dehydrogenases, an isomerase, and a lyase reaction are also necessary for certain steps. Steroid hormone synthesis • C21: – progesterone: directly from pregnenolone – cortisol: from progesterone, hydroxylation at 11, 17 a 21 – aldosterone: from progesterone, 11 and 21 hydroxylation, 18 oxidation to aldehyde • C19: from progesterone or pregnenolone: during 2C shortage at C17 you gain oxogroup, and subsequently OH → testosterone • C18: estrogen: aromatase (cleaves C18) Adrenal steroids A schematic representation of the pathways involved in the synthesis of the three major classes of adrenal steroids. The modifications at each step are shaded. Steroids Regulation of steroid synthesis • 3 regulatory steps: – Cholesterol release from internalized LDL – StAR protein = cholesterol transporter across the inner mitochondrial membrane – SCC = mitochondrial side chain cleavage enzyme • Signal: pituitary hormones (ACTH, LH, FSH) or angiotensine Steroid hormone degradation • Steran core cannot be cleaved in body • In the liver: hydroxylation and conjugation with glucuronides or sulphates • Urinary excretion of their metabolites can be used for the diagnosis. • Small part is excretes inchanged in the urine: UFC (urine free cortisol) Chemistry of hormones • Steroids • Small molecules - NO • Amino acids derivates Receptor inside the cell – Thyroid hormones – Catecholamines • Proteins and peptides • FA derivates - eicosanoids Surface recceptors Nitric oxide NO: produced by NO-synthase NH2 NH NH CH2 CH2 + NADPH + H+ CH2 CH2 HC NH3+ COOArginin NH2 O NH CH2 NADP+ + NO CH2 CH2 CH2 HC NH3+ COOCitrullin Nitric oxide • NO-synthase (NOS) – In neurons: NOS-I: neurotransmission – In macrophages: NOS-II: kills bacteria – Endothelial: NOS-III: vasodilation: difusion of NO toward the smooth muscle, activation of guanylatecyclase → cGMP → relaxation of the smooth muscle cells of the media → vasodilation • Clinical correlation: – Nitrates in the treatment of angina pectoris – Refractory hypotension during septic shock Nitric oxide • Interaction of an agonist (eg acetylcholine) with a receptor leads to intracellular release of Ca2+ via inositol trisphosphate generated by the phosphoinositide pathway, resulting in activation of NO synthase. Nitric oxide • The NO subsequently diffuses into adjacent smooth muscle, where it leads to activation of guanylate cyclase, formation of cGMP, stimulation of cGMP-protein kinases, and subsequent relaxation. • The vasodilator nitroglycerin is shown entering the smooth muscle cell, where its metabolism also leads to formation of NO. Chemistry of hormones • Steroids • Small molecules - NO • Amino acids derivates Receptor inside the cell – Thyroid hormones – Catecholamines • Proteins and peptides • FA derivates - eicosanoids Surface recceptors Thyroid hormones Thyroid hormones • The formation of triiodothyronine (T3) and thyroxine (T4) has many specific steps: • 1) Requires a rare element (iodine) for bioactivation. • 2) Hormones are synthesized as part of a very large precursor molecule (thyroglobulin) • 3) They are stored in an extracellular reservoir (colloid) • 4) There is peripheral conversion of T4 to T3, which is a much more active hormone. Thyroid hormones • In most parts of the world, iodine is a scarce component of soil, and for that reason there is little in food. • A complex mechanism has evolved to acquire and retain this crucial element and to convert it into a form suitable for incorporation into organic compounds. Thyroid hormones synthesis – key steps • 1) Secondary active transport of iodide into colloid • 2) Peroxidase iodidases Tyr residues of thyroglobulin • 3) Endocytosis and breakdown of thyroglobulin (Tgb) provide monoiodotyrosine (MIT) + diiodotyrosine (DIT) to condense to T4 and T3 • 4) Secretion of T3 and T4 is stimulated by TSH • 5) In plasma, T4 and T3 are bound to proteins: – – Albumin TBG (Thyronine binding globulin ) Iodide metabolism in the follicle • Iodide enters the thyroid through a transporter. • Thyroid hormone synthesis occurs in the follicular space through a series of reactions. • Thyroid hormones, stored in the colloid, are released from thyroglobulin by hydrolysis inside the thyroid cell. Hormony štítné žlázy Thyroglobulin (Tgb) • Thyroglobulin is the precursor of T4 and T3. It is a large iodinated, glycosylated protein. • Tgb contains many tyrosine residues, each of which is a potential site of iodination. • About 70% of the iodide in Tgb exists in the inactive precursors, monoiodotyrosine (MIT) and diiodotyrosine (DIT), while 30% is in the iodothyronyl residues - T4 and T3. Iodination of Tgb Thyreoglobulin CO C CH H2 NH HO I HO O I Trijodthyronin (T3) Tyr I HO I Thyreoglobulin CO C CH H2 NH MIT I HO I O I I Thyroxin (T4) I HO I DIT Thyreoglobulin CO C CH H2 NH H C C COOH H2 NH2 H C C COOH H2 NH2 Thyroglobulin (Tgb) • When iodine supplies are sufficient, the T4:T3 ratio is ~ 7:1. • In iodine deficiency, this ratio decreases, as does the DIT:MIT ratio. • Tgb provides the conformation required for tyrosyl coupling and iodide organification necessary in the formation of the diaminoacid thyroid hormones. Thyroglobulin (Tgb) • Thyroglobulin is synthesized in the basal portion of the cell and moves to the lumen, where it is a storage form of T3 and T4 in the colloid (several weeks' supply of these hormones exist in the normal thyroid). • Within minutes after stimulation of the thyroid by TSH, colloid reenters the cell and there is a marked increase of phagolysosome activity. • Various acid proteases and peptidases hydrolyze the thyroglobulin into its constituent amino acids, including T4 and T3, which are discharged from the basal portion of the cell. Iodide metabolism • The thyroid is able to concentrate I– against a strong electrochemical gradient. This is an energydependent process and is linked to the Na+/K+ ATPase-dependent thyroidal I– transporter. • The ratio of iodide in thyroid to iodide in serum (T:S ratio) is a reflection of the activity of this transporter. • This activity is primarily controlled by TSH and ranges from 500:1 in chronical stimulation with TSH to 5:1 or less when there´s no TSH. • The T:S ratio in humans on a normal iodine diet is about 25:1. Iodide metabolism • The thyroid is the only tissue that can oxidize I– to a higher valence state, an obligatory step in I– organification and thyroid hormone biosynthesis. • This step involves a peroxidase and occurs at the luminal surface of the follicular cell. • Thyroperoxidase requires H2O2 (is produced by an NADPH-dependent enzyme). Iodide metabolism • A number of compounds inhibit I– oxidation and therefore its subsequent incorporation into MIT and DIT. • The most important of these are the thiourea drugs. They are used as antithyroid drugs because of their ability to inhibit thyroid hormone biosynthesis at this step. Iodide metabolism • Once iodination occurs, the iodine does not readily leave the thyroid. Free tyrosine can be iodinated, but it can not be incorporated into proteins (no tRNA recognizes iodinated tyrosine). • The coupling of two DIT molecules to form T4 (or of an MIT and DIT to form T3) occurs within the thyroglobulin molecule. • A separate coupling enzyme has not been found, it is assumed that the same thyroperoxidase catalyzes this reaction. • The formed thyroid hormones remain as integral parts of thyroglobulin until the latter is degraded, as described before. Iodide metabolism • A deiodinase removes I– from the inactive MIT and DIT molecules in the thyroid. This mechanism provides a substantial amount of the I– used in T3 and T4 biosynthesis. • A peripheral deiodinase in target tissues such as pituitary, kidney, and liver selectively removes I– from the 5' position of T4 to make T3, which is a much more active molecule. • In this sense, T4 can be thought of as a prohormone, though it does have some intrinsic activity. Chemistry of hormones • Steroids • Small molecules - NO • Amino acids derivates Receptor inside the cell – Thyroid hormones – Catecholamines • Proteins and peptides • FA derivates - eicosanoids Surface recceptors Catecholamine synthesis • Substrate = Phe or Tyr • Synthesis located in: adrenal medulla (A), neural tissue (NA, DA) • Produced in the cytoplasm of the cells • Keeping in preformed vesicles • Free transport in plasma • Surface receptors: – After receptor binding – activation of G-protein • Products: – Epinephrine - adrenaline (hormone) – dopamine, norepinephrine - noradrenalin (neurotransmiters) Catecholamines are made from tyrosine • The major product of the adrenal medulla is epinephrine. This compound constitutes about 80% of the catecholamines in the medulla, and it is not made in extramedullary tissue. • In contrast, most of the norepinephrine present in organs innervated by sympathetic nerves is made in situ (about 80% of the total), and most of the rest is made in other nerve endings and reaches the target sites via the circulation. • Epinephrine and norepinephrine may be produced and stored also in other chromaffin tissues. Catecholamines are made from tyrosine • The conversion of tyrosine to epinephrine requires four sequential steps: • 1) ring hydroxylation • 2) decarboxylation • 3) side chain hydroxylation to form norepinephrine • 4) N-methylation to form epinephrine Catecholamines are made from tyrosine • Tyrosine hydroxylase is rate-limiting step for catecholamine synthesis. • It converts L-tyrosine to Ldihydroxyphenylalanine (L-dopa). • As the rate-limiting enzyme, tyrosine hydroxylase is regulated in a variety of ways. • The most important mechanism involves feedback inhibition by the catecholamines. Catecholamines are made from tyrosine • Dopa decarboxylase is present in all tissues. • This enzyme transforms L-dopa to 3,4dihydroxyphenylethylamine (dopamine). • Compounds that resemble L-dopa, such as αmethyldopa, are competitive inhibitors of this reaction – α-methyldopa is effective in treating some kinds of hypertension. Catecholamines are made from tyrosine • Dopamine-β-hydroxylase catalyzes the conversion of dopamine to norepinephrine. Catecholamines are made from tyrosine • Phenylethanolamine-N-methyltransferase (PNMT) catalyzes the production of epinephrine. • PNMT catalyzes the N-methylation of norepinephrine to form epinephrine in the adrenal medulla. • The synthesis of PNMT is induced by glucocorticoid hormones that reach the medulla via the intra-adrenal portal system. • This special system provides for a 100-fold steroid concentration gradient over systemic arterial blood, and this high intra-adrenal concentration appears to be necessary for the induction of PNMT. Catecholamin synthesis Tyrosine hydroxylase H C C COOH2 NH3+ 1. Phenylalanin H C C COOH2 NH3+ HO 2. HO Tyrosin 3,4 DihydrOxyPhenylAlanin (DOPA) DOPA decarboxylase H H2 C C HO HO Adrenalin H H2 C C 5. HO OH NH CH3 HO N-methyltransferase H C C COOH2 NH3+ HO OH NH3+ 4. 3. HO HO Dopamine βhydroxylase Noradrenalin Dopamin H2 C C + CO2 H2 NH3+ Catecholamines are made from tyrosine • Catecholamines cannot cross the blood-brain barrier – in the brain they must be synthesized locally. • In certain central nervous system diseases (eg, Parkinson's disease), there is a local deficiency of dopamine synthesis. • L-Dopa, the precursor of dopamine, readily crosses the blood-brain barrier and so is an important agent in the treatment of Parkinson's disease. Catecholamine breakdown Two key enzymes: MAO = monoaminooxidase COMT = catechol-o-methyl transferase MAO HO H C 77 COO78 OH CH3O COMT Inhibitors of MAO (IMAO) = antidepresive drugs Chemistry of hormones • Steroids • Small molecules - NO • Amino acids derivates Receptor inside the cell – Thyroid hormones – Catecholamines • Proteins and peptides • FA derivates - eicosanoids Surface recceptors Protein and peptide hormones • Neurotransmiters a neuromodulators: neuropeptides, opioids • Hypothalamic releasing hormones and pituitary peptides • Insulin and glucagone • Growth factors: IGF, CSF, EPO • Intestinal hormones … and many others General steps of peptide synthesis and action • • • • • • • • Expression of “pre-pro” protein Transport to ER Splitting the signaling sequence – we gain „pro-peptid“ Final posttranslational modifications in Golghi (there can be cleavage to definitive peptides) – proinsulin → insulin – POMC - proopiomelanocortine → MSH, ACTH and β-endorfine Their granules are stored in GA Free transport in plasma Surface receptors After receptor binding – Activation of membrane enzyme (insulin) – Activation of G protein Cellular mechanisms for peptide synthesis and release • Proteins synthesised by ribosomes are threaded through the membrane of the rough ER, from where they are conveyed in transport vesicles to the GA. • Here, they are sorted and packaged into secretory vesicles. Cellular mechanisms for peptide synthesis and release • Processing (cleavage, glycosylation, amidation, sulfation, etc.) occurs within the transport and secretory vesicles, and the products are released from the cell by exocytosis. Cellular mechanisms for peptide synthesis and release • Constitutive secretion (plasma proteins and clotting factors by liver) occurs continuously and only little material is stored in secretory vesicles. • Regulated secretion (cytokines or neuropeptides) occurs in response to increased intracellular Ca2+ or other intracellular signals, and material is typically stored in some amounts in secretory vesicles awaiting release. Degradation of peptide hormones • Lyzosomal degradation after endocytosis of complex hormonereceptor • Chemical modification (liver): rearrangement of S-S bridges, cleavage • Renal excretion of small peptides Chemistry of hormones • Steroids • Small molecules - NO • Amino acids derivates Receptor inside the cell – Thyroid hormones – Catecholamines • Proteins and peptides • FA derivates - eicosanoids Surface recceptors Eicosanoids • Derivates of arachidonic acid (20C:∆5,8,11,14). • Paracrine action, low plasma concentration, short halflife, no storage • Many functions: – Immunity/inflamation – Blood clotting – Regulation of the microcirculation… Eicosanoids • General steps of synthesis: – Release of arachidonic acid from membrane PL (enzyme PLA2) • After cleavage of PIP2 by PLCγ • This step is inhibited by glucocortikoids. – Cyclooxygenase (COX) produces prostaglandins and tromboxanes. • Acetylsalicylic acid and non-steroid antiinflammatory drugs (NSAID) inhibit COX. – Lipoxygenase → leukotrienes Prostaglandins 5 8 1 COO20 11 14 Kyselina arachidonová Arachidonate COX Inhibitors: - ASA (Aspirin) - paracetamole COX 1-3 O COO- O OOH Prostaglandin G2 Prostaglandin G2 (PGG2) Thromboxanes Contain oxane ring Synthetized from prostaglandines Role in blood clotting COO- O O OH Thromboxane A2 Leukotriens • Lipoxygenase: adds hydroperoxy (-OOH) group to C2, 12 or 15 of arachidonic acid • HPETE: hydroperoxyeikosatetrenoic acid • Conjugation with Cys or GSH • Antileukotrienes – antagonists of leukotriens receptors (zafirlukast, montelukast) in the treatment of bronchial astma