* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Circulatory System
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Artificial heart valve wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
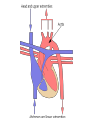
The Circulatory System Interesting Facts •The heart beat is strong enough to squirt blood 30 feet •The longer a boy’s ring finger is, the less likely they are to have a heart attack (according to one study) •The human heart beats ~35 million times per year •The heart pumps ~1,000,000 barrels of blood in a lifetime •Most heart attacks occur between 8-9 a.m. Interesting Facts •The blue whale has the largest heart – it weighs ~ one ton •The hummingbird has a heart that beats 1000 times per minute •Your entire volume of blood goes through your entire body once every minute •Humans have ~60,000 miles of blood vessels in their bodies (more than twice the circumference of the earth!) •Your heart beats 100,000 times and pumps ~2000 gallons of blood every day •Pig and baboon hearts have been transplanted into humans Cardiovascular System •Heart, vessels, blood •Function: transport gases, nutrients, wastes, hormones The Heart •Size of a fist; less than a pound •In thorax; flanked by lungs; rests on diaphram •Top: base •Bottom: apex •Double-layered sac covering the heart •Outer layer anchors heart in chest •Inner layer (epicardium) attached to heart wall •Lubricating fluid in pericardial space (between layers) reduces friction Pericardium Pericarditis Decrease in fluid causes layers to cling & rub against each other resulting in pain & decreased efficiency of heart Pericardial Tamponade •Bleeding into pericardial space after chest trauma •Excess blood restricts expansion of heart during pumping •Causes shock or death if not corrected Heart Wall 3 layers: •Epicardium: outer wall joined with pericardium •Myocardium: the actual cardiac muscle that contracts •Endocardium: lines heart chambers & vessels Heart Chambers Four chambers: •2 atria: top of heart – receive blood from veins •2 ventricles: bottom of heart – pump blood through arteries Heart Chambers Heart sounds (Luppdupp) from valves closing •Septum: divides left from right heart •Valves: keep blood flowing in one direction •Four valves: • 2 AV valves, • 2 semilunar valves Atrioventricular Valves AV valves: between atria and ventricles •Bicuspid (mitral) valve: on the left •Tricuspid valve: on the right •When valves are open blood drains from atria into ventricle •When ventricle contract, valve flaps are forced shut, blocking blood from reentering atria Semilunar Valves •Located in arteries leaving ventricles •Pulmonic valve: at base of pulmonary artery •Aortic valve: at base of aorta •When ventricles contract, valves are forced open & let blood flow •When ventricle relaxes, backflow of blood fills flaps of valve & forces them to shut •Arteries: carry blood away from the heart •Veins: carry blood to the heart •Capillaries: connect arteries to veins & exchange gases with tissues Blood Vessels Arteries •Carry blood at high pressure •Very thick, stretchy walls that expand in size •Most carry oxygenated blood (red) •Damaged arteries spurt in time to heart beat Arteries •Aorta: largest vessel (diameter of a garden hose) – receives blood from left ventricle •Arteriole: smaller vessels connecting arteries to capillaries •Carry blood at low pressure •Have valves to prevent backflow of blood against gravity •Most carry deoxygenated blood (purple) •Damaged veins ooze blood Veins •Vena Cava: dump all blood from the body into the right atria • superior vena cava: receives blood from upper body • inferior vena cava: receives blood from lower body •Venules: smaller vessels connecting veins to capillaries Veins Capillaries •Connect arteries and veins •Walls are one cell thick •Allow exchange of gases through thin walls • Drop off oxygen delivered from heart by arteries • Pick up CO2 and send it to the heart thru veins How Blood Travels thru Vessels heart artery arteriole capillary venule vein heart •Narrowing of vessel lumen due to plaque/fat formation on inside of walls •Causes: diet high in fat, cholesterol, salt; inactive lifestyle; smoking •Risks: high BP, enlarged heart, embolus blocking circulation; stroke Atherosclerosis Coronary Artery Disease •When Atherosclerosis affects the arteries that supply the heart muscle •Symptoms: short of breath after simple exertion, angina (chest pain) •Risk: MI, cardiac arrest, death How is CAD treated? •Medication •Angioplasty (balloon surgery) – balloon is inserted and inflated in blocked vessel to compress fatty mass against the artery wall How is CAD Treated? •Stent – wire mesh inserted into the artery to expand its lumen •Coronary Artery Bypass – arteries are removed from leg and grafted into the heart to restore circulation Vessel Disorders Varicose Veins: twisted, dilated veins resulting from pooling of blood due to long periods of standing, obesity, or inactivity Vessel Disorders Thrombophlebitis: inflammation of a vessel due to clot formation & poor circulation. Clot can become an embolus if freed. •Weaking in the wall of a vessel, causing it to balloon outwards. •Rupture of the site causes Aneurysm • Stroke (if in the brain) • Death (in a large artery – aorta). •Coronary arteries exit the aorta & supply oxygen/blood to heart muscle (myocardium) •Coronary veins pick up & return deoxygenated blood from myocardium Cardiac Circulation Defects in Coronary Circulation •Angina Pectoris: impaired circulation to myocardium causes oxygen deprivation & pain •Myocardial infarction: “heart attack” – blockage of circulation to section of myocardium causes the muscle to infarct (die) Pulmonary Circulation •Right ventricle pumps deoxygenated blood through pulmonary artery to the lungs •The blood picks up O2 from the lungs and dumps CO2 into the lungs •Oxygenated blood is returned to the left atrium thru the pulmonary vein Systemic Circulation •Oxygenated blood is pumped from left ventricle thru aorta to the body •Blood dumps oxygen into tissues and picks up CO2 •Deoxygenated blood travels from body to vena cava to the right atrium The Circulation Play the Game Number the parts 1 – 17 (just write the correct order on a piece of paper). Pass your paper to a classmate when you finish. We will grade them as a class. Congestive Heart Failure •Heart is ‘worn out’ from hypertension, multiple MI, atherosclerosis, or age •Heart pumps too weakly to meet tissue needs •If one side is weaker than the other, blood will back up in system Congestive Heart Failure •Left ventricle is failing: • Pulmonary congestion • Pulmonary edema (blood in lungs) causes suffocation •Right ventricle is failing: • Peripheral congestion • Edema in distal body parts (ankles, feet) Pulmonary Edema Pulmonary edema (A); normal lung (B) Peripheral Edema Swelling of feet and ankles due to CHF Conduction System of the Heart Heart is under two types of control: •Autonomic Nervous system • Sympathetic: speeds up contractions • Parasympathetic: the “brakes” that slows down contractions •Intrinsic Conduction System • Also called “nodal system” • Heart determines its own rate of contractions Intrinsic Conduction System •Nodes are heart tissue that stimulate heart muscle to depolarize (contract) •Depolarization moves from base to apex •Different areas of the heart have different nodes, each with a different rate •Node rate gets slower as it moves downwards •Faster nodes will override slower nodes Nodes (you need to know these) 3 Stages: •SA node fires, atria contract (depolarize) •Impulse travels to AV node, then travels thru bundle of His, bundle branches, & Purkinje fibers – ventricles contract (depolarize) •Contraction of ventricles has ‘wringing’ action, pushing blood upward and out through large arteries •Heart muscle repolarizes Parts of the Conduction System SA node: •“The Heart’s Pacemaker” •In atria •Normally sets the pace of 60 – 70 •SA can increase rate when stimulated by drugs, fever, or sympathetic NS (exercise, stress, emotion) AV Node: •Between atria & ventricles •Special tissues transmit signal from SA to AV node •Intrinsic rate: 40 - 60 Bundle of His: •Transmits impulse to ventricles •Rate: 30 – 40 beats/min Bundle Branches: •Within ventricular muscles •Rate: 20 – 30 beats/min Purkinje fibers: •Terminal end of branches Parts of the Conduction System What if Damage Occurs? •If SA node is damaged or its signal is blocked, the AV node takes over setting the pace (40-60/min) •If AV node is next damaged, the bundles set the rate (20 – 40/min) What is a Pacemaker? If heart is unable to generate impulse, or pace is too slow, mechanical pacemaker is surgically implanted to provide artificial impulses Electrocardiogram (ECG/EKG) •Electrical impulses in heart are measured with ECG •Electrical activity is translated into waves Electrocardiogram (ECG/EKG) •P Wave: atria depolarize •QRS complex: ventricles depolarize •T wave: repolarization •Heart Monitor hooked up with pads on chest •Abnormalities in ECG used to diagnose heart damage •Diagnostic signs: changes in shape of wave, distance between waves, lack of waves… Abnormalities in ECG Irregular Heart Rhythms •Tachycardia: heart is beating too fast •Bradycardia: heart is beating too slow •Heart Block: no connection between atria & ventricles – ventricles beat at their own rate •Ventricular Fibrillation: heart is ‘shivering’ – no contractions or pulse (cardiac arrest) •Asystole: dead heart – no electrical activity Comparing Rates •Normal Sinus Rhythm •Sinus Bradycardia •Sinus Tachycardia •Elevated ST segment (sign of a MI) •Ventricular Tachycardia •Heart Block •PVC (premature ventricular fibrillation) •Ventricular Fibrillation •Asystole Cardiac Cycle Cardiac Cycle: The events within one heartbeat. Three main stages: •Mid-to-late diastole: SL valves are closed, AV open; atria contract; blood is forced into ventricles •Ventricular systole: ventricular pressure forces AV closed; SL forced open; blood rushes out of ventricles; atria relax & refill •Early diastole: SL shut; AV open; ventricles relax and refill passively Heart Sounds •Cardiac cycle heard with a stethoscope •Two sounds: “lub dup” (pause) “lub dup” (pause) ….. • Lub = closing of AV valves (ventricular systole) • Dup = Closing of semilunar valves (between ventricular systole & diastole) •Murmurs: abnormal heart sounds that usually indicate valve problems Valve Disorders •Leaky Valves: caused by incompetent or deformed valves that force the heart to repump blood because of backflow Stenosis Valves are stiff and do not open completely. Heart has to pump harder Murmur: stenosis •The most common valve disorder (5-10% of people) •Mitral valve opens (prolapses) into atrium when shutting & allows blood backflow Mitral Valve Prolapse Cardiac Output •Cardiac Output: the amount of blood pumped by each side of the heart per minute •Cardiac output = heart rate X stroke volume •Stroke volume = the amount of blood pumped with each contraction What is the cardiac output if…. HR = 75 bpm; SV = 70 ml/beat? This is the normal cardiac output for a resting adult. How is the output affected with exercise? Do you think it increases or decreases? What affects Stroke Volume?(you don’t have to write this down) Increase in Stroke volume: •Increased venous blood return • exercise (muscles force blood into heart) • Slow hr (more time to fill ventricles) Decrease in stroke volume •Decreased venous return • Hemorrhage (less blood volume) • Tachycardia (not enough time to fill) What affects Heart Rate?(you don’t have to write this either) Increase: •Decline in SV (heart compensates by hr) •Babies and kids •Females •During exercise •Sympathetic NS Decrease: •Parasympathetic NS •Getting older •Males •Being fit (heart is more efficient) •Cold temperatures Taken to assess overall health status •Arterial pulse •Blood Pressure •Respiratory Rate •Temperature •Alternating expansion and recoil of arteries with each heart beat •Measured in beats per minute •Normal resting pulse: 60 – 100 bpm •Taken at pulse points: place where pulse is easily palpated (felt) Arterial Pulse Pulse Points Can also be used as pressure points to stop bleeding Blood Pressure •Pressure of the blood against artery walls •Measured as systolic/diastolic (ex. 120/80) • Systolic: pressure at peak of contraction • Diastolic: pressure during ventricular relaxation •Can be taken by: • Auscultation (listening for pulse) • Palpation (feeling for pulse) •Normal: 100 + age / 60-90 •Cardiac Output (blood pumped per min) •Peripheral Resistance • friction inside vessel that hampers flow of blood • Usually results from narrowing of arteries What Determines the BP? What affects BP Increases BP: •Atherosclerosis •Thick blood •Drugs/nicotine •Obesity Decreases BP: •Shock/blood loss •MI •Drugs •Physical fitness Problems with BP •Hypotension (low BP): • Systolic < 90mm/Hg • Cause: MI; warning sign of shock; athletes •Hypertension (high BP) • • • • • Systolic >140; Diastolic >90 Heart is forced to work hard for extended time Vessels damaged due to higher pressure Causes: obesity, diet, exercise, smoking, genes Risks: heart attack, stroke