* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dendritic cells at the end of the Millennium
Survey
Document related concepts
Duffy antigen system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
DNA vaccination wikipedia , lookup
Immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Major histocompatibility complex wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adaptive immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Transcript
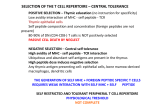
Immunology and Cell Biology (1999) 77, 404–410 Special Feature Dendritic cells at the end of the Millennium M R E S C I G N O, 1 F G R A N U C C I 2 A N D P R I C C I A R D I - C A S TAG N O L I 1 1 Department of Biotechnology and Bioscience, University of Milano-Bicocca and 2CNR Cellular and Molecular Pharmacology Center, Milan, Italy Summary We have recently proposed a dual role for dendritic cells (DC) in the amplification of innate immune responses and in the activation of adaptive immune responses. The DC are localized along the major routes of entry of micro-organisms, where they perform a sentinel function for incoming pathogens. Soon after interaction with appropriate stimuli, DC undergo a coordinated process of maturation and respond to danger signals by reprogramming their functions. The DC first regulate leucocyte recruitment at the site of inflammation, through the production of chemokines, inflammatory cytokines and interferons, and then they acquire migratory properties and undergo a rapid switch in chemokine receptor expression. This allows them to leave the inflamed tissue and to reach the lymph node T cell area. During this migration, DC complete their maturation process and acquire the ability to prime T cell responses. Thus, DC bridge innate and adaptive immunity. Key words: antigen presentation, chemokine, dendritic cell, dendritic cell maturation, innate response. Introduction During recent decades, studies of the immune response have concentrated on adaptive responses, particularly the mechanisms allowing the generation of a repertoire of antigenspecific receptors. Less effort has been made to understand how the immune system, when generating an innate response, is able to recognise micro-organism diversity and eventually direct the most appropriate type of adaptive response. The discovery of a new class of receptors (Toll-like receptors), which are involved in the recognition of characteristic patterns of groups of micro-organisms,1 has lead to a reevaluation of the role of the innate immune system as a discriminating system. Indeed, the induction of different types of effector adaptive responses seems to be directed by the innate system after recognition of particular groups of microorganisms (Fig. 1). Links between adaptive and innate immunity have been suspected and recently we have proposed that dendritic cells (DC) are the cells bridging the two arms of the immune system (Fig. 2). In fact, as well as their potent T cell stimulation, a salient feature of DC function is their so-called ‘maturation’ in response to stimuli that typically signal the presence of infection. Dendritic cells are distributed in most tissues and, in particular, in tissues that interface with the external environment, where micro-organisms can enter. The DC in peripheral tissues are immature, but capable of active antigen uptake through regulated endocytosis and phagocytosis. After exposure to micro-organisms, the maturing DC produce chemokines, cytokines and IFN-α/β, thus indicating a role for DC in cell recruitment and in amplifying innate responses. Only hours after micro-organism exposure, DC undergo a process of maturation involving the translocation of MHC class II molecules from intracellular compartments to the cell surface and the neo-biosynthesis of class I molecules.2,3 Matured DC also express high levels of costimulatory and adhesion molecules that favour T cell stimulation. In addition, mature DC up-regulate particular chemokine receptors, such as CCR7, that are believed to direct DC migration to lymphoid organs. The divergent effect of maturation signals on the expression of different chemokine receptors suggests a ‘weigh anchor: hoist the sail’ model for the trafficking of DC. Evidence of the in vivo relevance of these in vitro findings has recently been shown (C Reis e Sousa, pers. comm., 1999). Indeed, microbial stimuli have been reported as activating DC in vivo, causing accelerated migration to the T cell areas of lymphoid tissues, increased presentation of antigen and up-regulation of costimulatory molecules. The present review aims to illustrate the re-programming of DC activity in the early and later hours following exposure to micro-organisms or their products. To investigate DC maturation and the signals inducing appropriate DC priming, it is important to generate a homogeneous DC population and to maintain the cells in their immature stage. In our laboratory, we have established culture conditions for generating long-term, growth factordependent immature myeloid DC from either mouse spleen or bone marrow.2 These cells possess all of the properties of immature DC, but can be induced to full and appropriate maturation with LPS, lipotechoic acid (LTA) or the uptake of bacteria. The antigen uptake function is regulated during DC maturation Correspondence: P Ricciardi-Castagnoli, Department of Biotechnology and Bioscience, University of Milano-Bicocca, Milan, Italy. Email: <[email protected]> Received 21 June 1999; accepted 21 June 1999. When DC were first described,4 an extensive study of their properties was hampered by their paucity in tissues and by the difficulty of obtaining homogeneous immature DC populations in vitro that were free of contaminating Dendritic cells 405 Figure 1 The dendritic cell (DC) maturation process after encountering different groups of micro-organisms. TLR, Toll-like receptor. Figure 2 Dendritic cells (DC) as a bridge between adaptive and innate immune responses. macrophages. Thus, because antigen uptake is a property of immature DC, the phagocytic capacity of DC has long been denied.5 Not only are DC better phagocytic cells when immature, but, most remarkably, DC readily increase their antigenuptake capacity 1–2 h after activation. They then progressively reduce this capacity during the late stages of maturation (F Granucci et al., unpubl. data, 1999). Thus, DC control the extent of antigen internalization and limit bacterial ingestion by down-regulating phagocytosis. Three major pathways of antigen uptake have been described in DC: (i) phagocytosis; (ii) receptor-mediated endocytosis; and (iii) macropinocytosis.6 Conventional phagocytosis is the main entry for microbes, including bacteria.7 The DC can engulf the bacteria by actively surrounding them with pseudopodia. This process is either started by phagocytosis-promoting receptors of the Fc type or it is dependent on complementary signals in the case of complement-type receptors. The movement of the pseudopodia in activated DC involves actin-binding proteins and it can be blocked by the drug cytochalasin D, which stops the polymerization of actin.2 In addition to the conventional zipper-type phagocytosis, DC have been found to also use coiling phagocytosis for the uptake of bacteria.8 Phagocytosis of bacteria may take place either via direct interaction between microbial adhesins and phagocytic receptors (nonopsonic uptake) or indirectly via opsonins (for example, antibody or complement). These act as bridging molecules between the microbial surface and opsonin receptors of the phagocytes (opsonic uptake). Dendritic cells express a number of receptors that mediate endocytosis. These include Fc receptors (FcR), the Mac-1 (CD11b/CD18, αMβ2 integrin) molecule, CD14, DEC-205 and mannose receptors and the new family of ‘danger’ receptors called TLR (toll-like receptors; Fig. 3). The Mac-1 molecule is the CR3 complement receptor used for the phagocytosis of complement-coated bacteria, but it can also mediate adhesion and chemotaxis.9 It is stored in intracellular vesicles, which are rapidly mobilized to the cell surface in response to chemoattractants.10 The mannose receptor is a 175 kDa C-type lectin, which is expressed predominantly on macrophages and dendritic cells, including immature DC. It has a high affinity for carbohydrates, being involved in the internalization and presentation of mannosylated proteins.11 CD14 has long been described as an LPS receptor, but, lacking an intracellular transducing cytoplasmic tail, it could not be considered as the only mediator of LPS-induced activation of DC. Very recently, the transducing receptor for LPS has been identified in TLR 2 and 4.12,13 The TLR family of proteins have been described as key players in triggering innate defences against bacterial and fungal invaders.14 The engagement of TLR 4 induces the nuclear translocation of the nuclear factor (NF)-κΒ transcription factor14 via activation of MyD88 and interleukin-1 receptor-associated kinase (IRAK) and analogously, LPS-induced activation of DC is mediated by NF-κΒ.15 406 M Rescigno et al. Figure 3 Key molecules in early and late dendritic cell (DC) functions. MARCO/R, MARCO receptor; TLR, Toll-like receptor; ICAM, intracellular adhesion molecule; LFA, leukocyte function-associated antigen. Thus, receptors involved in endocytosis can be divided into two classes by their capacity to bind pathogen-associated molecular patterns (PAMP) either directly or indirectly by binding complexes of PAMP and their receptors (Fig. 3). Macropinocytosis is a process by which large pinocytic vesicles are generated, which sample extracellular fluids and solutes. ‘Weigh anchor: hoist the sail’ Immature DC originate in the bone marrow and migrate to peripheral non-lymphoid tissues through the blood. Although immature blood DC have been identified in humans, the nature of circulating DC remains unknown. It has been proposed that blood DC may represent a reservoir of DC tissue precursors that can extravasate to repopulate the pool of tissue DC. Nevertheless, they can also represent a set of circulating APC that continuously sense the endothelium and are strongly recruited at inflammation sites.16 Moreover, regarding the origin of tissue DC from circulating precursors, it has been observed that non-proliferating blood monocytes can differentiate into DC after two days culture in vitro with endothelial cells. These newly matured DC are able to reverse transmigrate across the endothelium, similarly to when DC enter the lymphatics. Cells that differentiate into macrophages do not have this migratory capability.17 Thus, the endothelium per se can play a fundamental role in driving the differentiation of macrophage and DC precursors into one lineage or another. Immature blood DC have a proven ability to interact continuously with the capillary dermal endothelium. The extravasation of leucocytes from the vasculature to the tissues has been described as a multistep mechanism involving selectins, chemoattractants and integrins.18 The initial adhesive step is generally mediated by selectins and α4 integrins. Immature blood DC uniformly express a glycosylated form of P-selectin glycoprotein ligand (PSGL)-1, able to bind P- and E-selectins. Under flow conditions in vitro, DC constitutively tether and roll on E- and P-selectins. In vivo, DC continuously interact with non-inflamed dermal endothelium and are able to extravasate during an inflammatory process.16 The extravasation phenomenon is regulated by chemokines produced by endothelial cells and surface integrins like intracellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1. Tissue-resident immature DC constantly monitor the environment for pathogens. Their migratory ability allows them to move, inside the tissue, toward inflammatory sites and from the site of inflammation to draining lymph node (through the lymphatic system), where they inform helper and cytotoxic T cells of the incoming danger. Inside lymph nodes, DC home in on the T cell-rich areas. Chemokines are not only involved in controlling the extravasation processes, but also in regulating DC movements inside non-lymphoid tissues and toward lymphoid tissues. Chemokines are produced by leucocytes and by endothelial and epithelial cells upon interaction with inflammatory stimuli.19 The specific effect of chemokines on target cell types is mediated by a family of G-protein-coupled seven trans-membrane receptors. Mouse and human DC express receptors for a number of inflammatory chemokines (Fig. 4). Because the migratory function of DC is tightly regulated, the expression of chemokine receptors also undergoes strict modulation during the inflammatory process and after the receptors have reached their final destination in the draining lymph nodes. Human, monocyte-derived immature DC express chemokine receptors, such as CCR1, CCR2, CCR5 and CXCR1, and respond to inflammatory chemokines, such as macrophage inflammatory protein (MIP)-1α, regulated upon activation, normal T cell expressed and presumably secreted (RANTES) and monocyte chemoattractant protein (MCP)-1.20,21 Thus, they are presumably attracted at the inflammatory site via a gradient of chemokines that are able to act on chemokine receptors expressed on their surface at the immature stage (Fig. 4). Following activation with inflammatory stimuli, such as LPS or TNF-α, DC down-regulate the expression of CXCR1, CCR1 and CCR520,21 and lose their ability to migrate in response to CCR1 and CCR5 ligands (MIP-1α, RANTES and MIP-1β) according to the model of ‘weigh anchor: hoist the sail’.20 Dendritic cells 407 Figure 4 (a) Chemokines produced by dendritic cells (DC). (b) Chemokine receptors expressed by DC. TARC, thymus and activation-regulated chemokine; MDC, macrophage-derived chemokine; RANTES, regulated upon activation, normal T cell expressed and presumably secreted; MIP, macrophage inflammatory protein; IP, IFN-γ inducible protein; CCR, C-C chemokine receptor; CXCR, CXC chemokine receptor. The precise kinetics of chemokine receptor regulation at early time points after LPS activation has been examined in murine proliferating DC.22 It has been shown that CCR1 expression and function are both first up-regulated between 30 min and 1 h after LPS stimulation and then progressively down-modulated from 2 h after LPS interaction.22 These kinetics correlate well with the spontaneous migration of proliferating mouse DC that is observed after LPS activation. The DC initially down-regulate their intrinsic migration function, with a maximum effect 2 h after stimulation, and then progressively increase it with a peak at 4–6 h after LPS treatment (F Granucci et al. unpubl. data, 1999). In contrast, after activation, human monocyte-derived DC strongly up-regulate the expression of CCR7, a chemokine receptor that responds to chemokines such as secondary lymphoid-tissue chemokine (SLC) and EBI1 ligand chemokine (ELC), which are expressed, respectively, by lymphatic endothelial cells and by mature DC in the T cell area of lymphoid organs.20 Slowly, activated DC acquire the ability to respond to ELC with a maximum effect 24–48 h after the activation stimulus. Moreover, by confocal microscopy, class II positive cells have been shown within lymphatic channels expressing SLC in the mouse dermis and SLC has been described as a potent chemoattractant for migrating maturing skin DC.23 Thus, the change in chemokine receptor expression represents one of the mechanisms for regulating the trafficking of DC inside the inflamed tissue and movement to lymphoid organs after antigen capture. The expression in immature DC (and up-regulation soon after activation) of receptors for inflammatory chemokines may represent a system to recruit and maintain DC at inflammatory sites. Here, DC remain to perform antigen uptake and to contribute to increase the inflammatory process in order to recruit new leucocytes. Finally, after losing the expression or the function of some chemokine receptors, DC can leave the inflammatory site and reach the draining lymph nodes through the afferent lymphatics. Expression of the CCR7 receptor allows them to be kept in the T cell area of the lymph node. The inflammatory process can be sustained by DC, because they are able to produce chemokines, such as MIP1α and MIP-2, which are well-known leucocyte attractants. In particular, it has been shown that proliferating mouse DC strongly up-regulate the mRNA for MIP-1α and MIP-2, beginning 1 h after LPS activation.22 It has been proposed that the chemokines produced so early during the process of maturation act as an autocrine loop to down-modulate the function of receptors, such as CCR1, via a desensitization process.22 This would allow DC to arrest at the site of inflammation, where they can recall new DC and neutrophils, attracted by MIP-1α and MIP-2 (Fig. 4). Immature DC also express RANTES, but its mRNA is down-regulated immediately after LPS activation and remains low during the entire period (2–3 h) in which DC are supposed to persist at the inflammatory site. This chemokine is finally strongly upregulated 24 h after LPS treatment, when DC have reached the lymphoid organs. Because RANTES, like other chemokines produced by mature DC (IFN-γ inducible protein (IP)-10 and MCP-1), is known to be active on T cells, these observations are consistent with the idea that, at the level of lymphoid organs, mature DC produce chemokines to attract T cells for antigen presentation and to activate the immune response.22 In fact, Langerhans’ cells that migrate to draining lymph nodes from inflamed skin up-regulate the expression of macrophage-derived chemokine (MDC; a chemoattractant for primed T lymphocytes) and are, indeed, able to attract activated T cells.24 It has been hypothesized that in an initial phase, maturing DC and naïve T cells are recalled in the T cell area of lymph nodes by chemokines such as SLC and ELC, so that DC can prime rare antigen-specific naïve T cells. Subsequently activated, dividing T cells are more efficiently attracted and kept in the T cell area by newly arriving DC-producing chemokines, such as MDC.24 Molecular checkpoints in MHC class II antigen presentation Professional APC are characterized by their ability to process and present antigens on MHC class II molecules. Newly synthesized class II α and β chain assemble in the endoplasmic reticulum (ER) with a third polypeptide, invariant chain (Ii chain), that renders MHC molecules inaccessible to peptides in the ER.25 Two pathways of antigen processing have been described, one involving assembled MHC-Ii chain molecules and the other based on Ii-chain-free MHC II dimers recycled from the plasma membrane. New MHC class II molecules are stored in a special compartment designated MHC II enriched compartment (MIIC). The MIIC were first described in B cells26 and then in DC.27 They contain late endosomal and lysosomal markers as well as HLA-DM or H-2M molecules, which enhance binding of peptides to MHC molecules. In the MIIC, MHC class II molecules are 408 M Rescigno et al. Figure 5 Scheme of the molecular events induced after bacterial or bacterial product activation of dendritic cells (DC). NIK, NF-κB-inducing kinase; TAP, transporter associated with antigen processing; CIIV, class II vesicles; MIIC, MHC II enriched compartments. continuously degraded and replaced by newly formed MHC II-Ii chain assembled molecules. The basal level of neobiosynthesis of MHC II molecules is indeed sustained in immature mouse DC.3 Depending on the maturation stages of DC, MHC II positive vesicles, distinct from late endosomes or lysosomes, have also been described and have been named class II vesicles (CIIV). In these structures, MHC class II molecules are free of the invariant chain. Interestingly, the dynamics of these vacuoles are closely related to DC maturation and are under the strict control of Ii-chain cleavage. Indeed, immature cells contain only MIIC compartments, in which MHC molecules are assembled with Ii chain. During maturation, there is a clear intermediate stage of the cells, which is characterized by the appearance of CIIV structures of Ii chain-free MHC II. The degradation of the Ii chain is catalysed by cathepsin S, whose activity is under the control of its inhibitor, cystatin C, whose level and localization are regulated during DC maturation.28 Eventually, CIIV fuse to the plasma membrane for exposure of MHC-peptide complexes at the cell surface, giving rise to the typical phenotype of mature DC. Being targeted to the plasma membrane, MHC II molecules are no longer subject to lysosomal degradation and their half-life is increased.3,29,30 Simultaneously, maturing DC progressively reduce neobiosynthesis and mRNA transcription of MHC II to a complete shut-off (F Granucci et al, unpubl. data, 1999). Against all odds: MHC class I presentation of exogenous antigens The MHC I molecules are expressed ubiquitously and their major role is to display a spectrum of peptides representing the intracellular protein composition, so as to allow continuous monitoring of the state of the cell by cytotoxic T cells (for microbial infection as well as malignant transformation).31 The nature of the pathway of MHC class I peptide loading has long been known to exclude the possibility that non- endogenously produced proteins could be presented on these molecules. Indeed, newly formed MHC I–β2-microglobulin (β2-m) molecules assemble in the ER with at least three proteins that ensure their stability in the absence of highaffinity peptide: calnexin, calreticulin and ERp57. This stable complex binds to another protein, tapasin, in order to associate with the transporter associated with antigen presentation (TAP). The TAP protein is responsible for the transport, and probably for the loading, of cytosolic peptides generated by the activity of the proteasome on to newly formed MHC I molecules. Thus, only those peptides that reach the endoplasmic reticulum can associate with MHC I molecules. After the binding of high-affinity peptides, the accessory molecules are released and MHC I–peptide complexes are exported to the cell surface. Although a recycling mechanism of MHC I molecules from the plasma membrane to endocytic vesicles has been described for macrophages,32 no such mechanism has been observed in DC. However, it has been recently shown that DC have the capacity to present exogenously introduced antigens on MHC I molecules3,33–35 via a mechanism that is proteasome and TAP dependent (Fig. 5). The nature of the antigen is critical for this exogenous antigen presentation on MHC I molecules. Indeed, soluble proteins are poorly presented, whereas antigens introduced via receptor-mediated endocytosis and phagocytosis are presented very efficiently.3,33–35 This is of major interest, because DC can prime CTL not only to viral antigens, but also to bacterial, tumoral and other antigens that can be internalized through mechanisms that are symptomatic of environmental ‘danger’. Interestingly, MHC I biosynthesis is highly up-regulated by bacteria and bacterial products,3,29 reaching a peak at 18 h when DC have acquired full T cell stimulatory capacity (Fig. 5). Moreover, only in the presence of bacteria, the half-life of MHC I molecules changes from 3 to 9 h, allowing presentation of bacterial proteins for longer periods, thus increasing the chance of meeting antigen-specific CTL. Dendritic cells 409 Figure 6 Time frame of the coordinated process of dendritic cell (DC) maturation. Soon after interaction with appropriate stimuli, DC respond to danger signals by stimulating a controlled and effective immune response. Dendritic cells first regulate leukocyte recruitment at the site of inflammation, through the production of chemokines and inflammatory cytokines, and then they acquire migratory properties and undergo a rapid switch in chemokine receptors. This allows them to leave the inflamed tissue and to reach the lymph node T cell area. MIP, macrophage inflammatory protein; RANTES, regulated upon activation, normal T cell expressed and presumably secreted; MCP, monocyte chemoattractant protein; SLC, secondary lymphoid-tissue chemokine; ELC, EBI1 ligand chemokine. Interestingly, concerning the classical MHC I pathway of antigen presentation when a cell is infected with a virus and the proteins are produced endogenously, the same set of virus proteins is processed differently if fibroblasts or DC are analysed.36 This agrees with the fact that LPS-activated DC up-regulate the PA28 proteasome subunit responsible for a change in the repertoire of peptides generated in the same cell (F Granucci et al, unpubl. data, 1999). Concluding remarks Dendritic cells are characterized by dual roles: amplification of innate immune responses and activation of the adaptive immune responses. The DC fulfil these tasks by taking up incoming pathogens and by undergoing a coordinated process of maturation after interaction with appropriate stimuli. The DC have the ability to sense the external environment and to respond to danger signals by stimulating a controlled and effective immune response. In this respect, DC could be considered as the conductors of the immune system. The initial production of inflammatory cytokines and chemokines regulates leucocyte recruitment at the site of inflammation. On down-regulation of some chemokine receptors and up-regulation of others, such as CCR7, DC can leave the inflamed tissue and reach the lymph node T cell area. Here, DC complete their maturation process and acquire the ability to prime T cell responses (Fig. 6). The nature of the original stimuli is likely to determine the type of DC maturation and cytokine milieu, which may result in different types of T cell responses. Acknowledgements We thank Elena Bottani for carefully editing the manuscript and generating the figures. This work was partially supported by CNR Finalised Project of Biotechnology, AIRC (Italian Association Against Cancer) and Biopolo. References 1 Medzhitov R, Janeway CAJ. Innate immunity: The virtues of a nonclonal system of recognition. Cell 1997; 91: 295–8. 2 Winzler C, Rovere P, Rescigno M et al. Maturation stages of mouse dendritic cells in growth factor-dependent long-term cultures. J. Exp. Med. 1997; 185: 317–28. 3 Rescigno M, Citterio S, Thèry C et al. Bacterial-induced neobiosynthesis, stabilization and surface expression of functional class I molecules in mouse dendritic cells. Proc. Natl Acad. Sci. USA 1998; 95: 5229–34. 4 Steinman RM, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J. Exp. Med. 1973; 137: 1142–62. 5 Austyn JM. New insights into the mobilization and phagocytic activity of dendritic cells. J. Exp. Med. 1996; 183: 1287–92. 6 Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature 1998; 392: 245–52. 7 Rescigno M, Granucci F, Citterio S, Foti M, Ricciardi-Castagnoli P. Coordinated events during bacteria-induced DC maturation. Immunol. Today 1999; 20: 200–3. 8 Rescigno M, Rittig M, Citterio S et al. Interaction of dendritic cells with bacteria. In: Lotze MT, Thomson AW (eds). Dendritic Cell: Biology and Clinical Applications. San Diego: Academic Press, 1999; 403–19. 410 M Rescigno et al. 9 Anderson DC, Miller LJ, Schmalstieg FC, Rothlein R, Springer TA. Contributions of the Mac-1 glycoprotein family to adherence-dependent granulocyte functions: Structure–function assessments employing subunit-specific monoclonal antibodies. J. Immunol. 1986; 137: 15–27. 10 Miller LJ, Bainton DF, Borregaard N, Springer TA. Stimulated mobilization of monocyte Mac-1 and p150,95 adhesion proteins from an intracellular vesicular compartment to the cell surface. J. Clin. Invest. 1987; 80: 535–44. 11 Tan MC, Mommaas AM, Drijfhout JW et al. Mannose receptormediated uptake of antigens strongly enhances HLA class IIrestricted antigen presentation by cultured dendritic cells. Eur. J. Immunol. 1997; 27: 2426–35. 12 Poltorak A, He X, Smirnova I et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: Mutations in Tlr4 gene. Science 1998; 282: 2085–8. 13 Yang RB, Mark MR, Gray A et al. Toll-like receptor-2 mediates lipopolysaccharide-induced cellular signalling. Nature 1998; 395: 284–8. 14 Medzhitov R, Preston HP, Janeway CJ. A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature 1997; 388: 394–7. 15 Rescigno M, Martino M, Sutherland CL, Gold MR, RicciardiCastagnoli P. Dendritic cell survival and maturation are regulated by different signalling pathways. J. Exp. Med. 1998; 188: 2175–80. 16 Robert C, Fuhlbrigge RC, Kieffer JD et al. Interaction of dendritic cell with skin endothelium: A new perspective on immunosurveillance. J. Exp. Med. 1999; 189: 627–35. 17 Springer TA. Trafficking signals for lymphocytes recirculation and leukocyte emigration: The multistep mechanism. Cell 1994; 76: 301–14. 18 Randolph GJ, Beaulieu S, Lebecque S, Steinman RM, Muller WA. Differentiation of monocytes into dendritic cells in a model of transendothelial trafficking. Science 1998; 282: 480–3. 19 Baggiolini M. Chemokines and leukocyte traffic. Nature 1998; 392: 565–8. 20 Sozzani S, Allavena P, D’Amico G et al. Differential regulation of chemokine receptors during dendritic cell maturation: A model for their trafficking properties. J. Immunol. 1998; 161: 1083–6. 21 Sallusto F, Schaerli P, Loetscher P et al. Rapid and coordinated switch in chemokine receptor expression during dendritic cell maturation. Eur. J. Immunol. 1998; 28: 2760–9. 22 Foti M, Granucci F, Aggujaro D et al. Upon dendritic cell activation chemokines and chemokine receptor expression are rapidly regulated for recruitment and maintenance of dendritic cells at the inflammatory site. Int. Immunol. 1999; 11: 101–8. 23 Saeki H, Moore AM, Brown MJ, Hwang ST. Secondary lymphoid-tissue chemokine (SLC) and CC chemokine receptor 7 (CCR7) participate in the emigration pathway of mature dendritic cells from the skin to regional lymph nodes. J. Immunol. 1999; 162: 2472–5. 24 Tang HL, Cyster JG. Chemokine up-regulation and activated T cell attraction by maturing dendritic cells. Science 1999; 284: 819–22. 25 Mellman I, Turley SJ, Steinman RM. Antigen processing for amateurs and professionals. Trends Cell. Biol. 1998; 8: 231–7. 26 Peters PJ, Raposo G, Neefjes JJ et al. Major histocompatibility complex class II compartments in human B lymphoblastoid cells are distinct from early endosomes. J. Exp. Med. 1995; 182: 325–34. 27 Sallusto F, Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulation by tumor necrosis factor alpha. J. Exp. Med. 1994; 179: 1109–18. 28 Pierre P, Mellman I. Development regulation of invariant chain proteolysis controls MHC class II trafficking in mouse dendritic cells. Cell 1998; 93: 1135–45. 29 Cella M, Engering A, Pinet V, Pieters J, Lanzavecchia A. Inflammatory stimuli induce accumulation of MHC class II complexes on dendritic cells. Nature 1997; 388: 782–7. 30 Pierre P, Turley SJ, Gatti E et al. Developmental regulation of MHC class II transport in mouse dendritic cells. Nature 1997; 388: 787–92. 31 Pamer E, Cresswell P. Mechanisms of MHC class I-restricted antigen processing. Annu. Rev. Immunol. 1998; 16: 323–58. 32 Rock KL. A new foreign policy: MHC class I molecules monitor the outside world. Immunol. Today 1996; 17: 131–7. 33 Bachmann MF, Lutz MB, Layton GT et al. Dendritic cells process exogenous viral proteins and virus-like particles for class I presentation to CD8+ cytotoxic T lymphocytes. Eur. J. Immunol. 1996; 26: 2595–600. 34 Regnault A, Lankar D, Lacabanne V et al. Fc gamma receptormediated induction of dendritic cell maturation and major histocompatibility complex I-restricted antigen presentation after immune complex internalization. J. Exp. Med. 1999; 189: 371–80. 35 Rovere P, Valinoto C, Bondanza A et al. Bystander apoptosis triggers dendritic cell maturation and antigen-presenting function. J. Immunol. 1998; 161: 4467–71. 36 Butz EA, Bevan MJ. Differential presentation of the same MHC class I epitopes by fibroblasts and dendritic cells. J. Immunol. 1998; 160: 2139–44.