* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Blood Composition
Immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Atherosclerosis wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
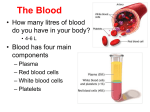
Chapter 43 The Immune System Overview: Reconnaissance, Recognition, and Response • An animal must defend itself from the many dangerous pathogens it may encounter – Pathogens are infectious agents that cause disease • Two major kinds of defense have evolved: immunity = defenses to avoid infection, disease, or other unwanted biological invasion – innate immunity – acquired immunity • Innate immunity is present before any exposure to pathogens and is effective from the time of birth • It involves nonspecific responses to pathogens • Innate immunity consists of external barriers plus internal cellular and chemical defenses • Key internal defenses are macrophages and other phagocytic cells 3 µm • Acquired immunity, or adaptive immunity, develops after exposure to pathogens such as microbes, toxins, or other foreign substances • It involves a very specific response to pathogens • Recognition is by white blood cells called lymphocytes • Some lymphocytes produce antibodies; others destroy infected cells, cancer cells, or foreign tissue INNATE IMMUNITY Rapid responses to a broad range of microbes External defenses Skin Mucous membranes Secretions Invading microbes (pathogens) ACQUIRED IMMUNITY Slower responses to specific microbes Internal defenses Phagocytic cells Antimicrobial proteins Inflammatory response Natural killer cells Humoral response (antibodies) Cell-mediated response (cytotoxic lymphocytes) Blood Composition and Function • Blood consists of several kinds of cells suspended in a liquid matrix called plasma • The cellular elements occupy about 45% of the volume of blood Plasma • Blood plasma is about 90% water • Among its solutes are inorganic salts in the form of dissolved ions, sometimes called electrolytes • Another important class of solutes is the plasma proteins, which influence blood pH, osmotic pressure, and viscosity • Various plasma proteins function in lipid transport, immunity, and blood clotting Plasma Lymph Serum55% Constituent Major functions Water Solvent for carrying other substances Ions (blood electrolytes) Sodium Potassium Calcium Magnesium Chloride Bicarbonate Plasma proteins Albumin Fibrinogen Immunoglobulins (antibodies) Osmotic balance, pH buffering, and regulation of membrane permeability Osmotic balance, pH buffering Clotting Defense Substances transported by blood Nutrients (such as glucose, fatty acids, vitamins) Waste products of metabolism Respiratory gases (O2 and CO2) Hormones Cellular elements 45% Cell type Number Functions per µL (mm3) of blood Erythrocytes (red blood cells) Hematocrit Separated blood elements 5–6 million Leukocytes 5,000–10,000 (white blood cells) Transport oxygen and help transport carbon dioxide Defense and immunity Lymphocyte Basophil Eosinophil Neutrophil Platelets Monocyte 250,000– 400,000 Blood clotting Cellular Elements • Suspended in blood plasma are two types of cells: – Red blood cells (erythrocytes) transport oxygen – White blood cells (leukocytes) function in defense • Platelets, a third cellular element, are fragments of cells that are involved in clotting Erythrocytes • Red blood cells, or erythrocytes, are by far the most numerous blood cells • They transport oxygen throughout the body Leukocytes • There are five major types of white blood cells, or leukocytes: monocytes, neutrophils, basophils, eosinophils, and lymphocytes • They function in defense by phagocytizing bacteria and debris or by producing antibodies Platelets • Platelets function in blood clotting platelets fibrin red blood cell white blood cell Stem Cells and the Replacement of Cellular Elements • The cellular elements of blood wear out and are replaced constantly throughout a person’s life Pluripotent stem cells (in bone marrow) Myeloid stem cells Lymphoid stem cells Erythrocytes, leukocytes, and platelets all develop from a common source, pluripotent stem cells in the red marrow of bones Basophils B cells T cells Lymphocytes Eosinophils Neutrophils Erythrocytes Platelets Monocytes Lymphocyte Development • Lymphocytes arise from stem cells in bone marrow • Newly formed lymphocytes are alike but later develop into B cells or T cells, depending on where they mature LE 43-10 Bone marrow Lymphoid stem cell B cell Thymus T cell Blood, lymph, and lymphoid tissues (lymph nodes, spleen, and others) Blood Clotting • When the endothelium of a blood vessel is damaged, the clotting mechanism begins • A cascade of complex reactions converts fibrinogen to fibrin, forming a clot blood vessel clot LE 42-17 Endothelium of vessel is damaged, exposing connective tissue; platelets adhere Platelets form a plug Seal is reinforced by a clot of fibrin Collagen fibers Platelet plug Fibrin clot Platelet releases chemicals that make nearby platelets sticky Clotting factors from: Platelets Damaged cells Plasma (factors include calcium, vitamin K) Prothrombin Thrombin Fibrinogen Fibrin 5 µm Red blood cell