* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Interferons
Immune system wikipedia , lookup
12-Hydroxyeicosatetraenoic acid wikipedia , lookup
Adaptive immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
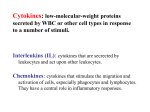
In The Name Of God The Most Compassionate The Most Merciful Cytokines and Growth Factors By Ali Jahanian Najafabadi Email: [email protected] Introduction • • • • A diverse group of regulatory proteins or glycoproteins Produced in minute quantities by the body Act as chemical communicators Intracellular signal transduction The major proteins/protein families that constitute the cytokine group of regulatory molecules Introduction • Mostly produced by, or act upon leukocytes IgG FcR Opsonized antigen IgER Hyper sensitivity IgER Parasitic worms Kupffer cells, microglia, and alveolar macrophages Introduction • Mostly produced by leukocytes Play a central role in: Regulating both immune and inflammatory function Processes such as haematopoiesis (the production of blood cells from haematopoietic stem cells in the adult bone marrow) Wound healing Introduction • Nomenclature: Cytokines: Firstly introduced in the mid 1970s for the polypeptide growth factors controlling the differentiation and regulation of cells of the immune system Additional classification: Lymphokines (cytokines such as IL-2 and IFN-γ, produced by lymphocytes) Monokines (cytokines such as TNF-α, produced by monocytes) On the basis of the specific biological activity by which the cytokine was first discovered TNF exhibited cytotoxic effects on some cancer cell lines CSFs promoted the growth in vitro of various leukocytes in clumps or colonies). Introduction • Nomenclature: Primary sequence analysis of cytokines coupled to determination of secondary and tertiary structure one of six families: Many are known by more than one name: IL-1: lymphocyte activating factor (LAF), endogenous pyrogen, catabolin and mononuclear cell factor Introduction • The effects of recombinant DNA technology and monoclonal antibody technology on the understanding of cytokine biology: Genetic engineering allowed production of large quantities of most cytokines. These could be used for structural and functional studies of the cytokine itself, and its receptor Analysis of cytokine genes established the exact evolutionary relationships between these molecules Detection of cytokine mRNA and cytokine receptor mRNA allowed identification of the full range of sources and target cells of individual cytokines Hybridoma technology facilitated development of immunoassays capable of detecting and quantifying cytokines Inhibition of cytokine activity in vivo by administration of monoclonal antibodies (and, more recently, by gene knockout studies) continues to elucidate the physiological and pathophysiological effect of various cytokines. Introduction • The following generalizations may be made with regard to most cytokines: Very potent regulatory molecules, nanomolar to picomolar concentrations Produced by a variety of cell types, which may be leukocytes or nonleukocytes: e.g. IL-1: leukocytes, non-leukocytes (such as smooth muscle cells, vascular endothelial cells, fibroblasts cells and collagen fibre, astrocytes and chondrocytes Many cell types can produce more than one cytokine: Lymphocytes: wide range of interleukins, CSFs, TNF, IFN-αs and IFN-γ Fibroblasts can produce IL-1, -6, -8, and -11, CSFs, IFN-β and TNF Introduction • The following generalizations may be made with regard to most cytokines: Most cytokines are pleiotropic, i.e. can affect a variety of cell types: IFN-γ stimulates activation and growth of T- and B lymphocytes, macrophages, NK cells, fibroblasts endothelial cells It also displays weak anti-proliferative activity with some cell types. Introduction • The following generalizations may be made with regard to most cytokines: Many cytokines play a regulatory role in processes other than immunity and inflammation: EPO Most cytokines are inducible, and are secreted by their producer cell: IL1IL2 potent cytokine inducers : infectious agents, tissue injury and toxic stimuli some cytokines appear to be expressed constitutively: EPO, CSFs Many cytokines exhibit redundancy: i.e. two or more cytokines can induce a similar biological effect: TNF-α and -β Introduction • The following generalizations may be made with regard to most cytokines: Cascade induction Introduction • Not all polypeptide regulatory factors are classified as cytokines: – Classical polypeptide hormones are not considered members of the cytokine family: Insulin, FSH and GH • • • • • Hormones Secreted by one types of specialized cells Unique action Restricted target cells and a limited spectrum of actions (excp insulin) Act at a distant site • • • • Cytokines Made by more than one type of cells Overlap actions (redundancy) Multiple target cells, multiple actions Short action radius EPO is produced in the kidney and liver and acts in an endocrine manner, promoting production of red blood cells in the bone marrow. EPO could thus also be considered to be a true hormone. Introduction • Autocrine,Paracrine and Endocrine Introduction • Cytokine receptors Introduction • Cytokine receptors Based upon amino acid sequence homology, receptors are usually classified as belonging to one of 5 known superfamilies: Immunoglobulin superfamily receptors Class I cytokine receptor family (also known as the hematopoietin receptor family) Class II cytokine receptor family (also known as the interferon receptor family) TNF receptor family Chemokine receptor family Introduction • Cytokine receptors Based upon amino acid sequence homology, receptors are usually classified as belonging to one of 5 known superfamilies: Immunoglobulin superfamily receptors Introduction • Cytokine receptors Based upon amino acid sequence homology, receptors are usually classified as belonging to one of 5 known superfamilies: Class I cytokine receptor family (also known as the hematopoietin receptor family) Introduction • Cytokine receptors Based upon amino acid sequence homology, receptors are usually classified as belonging to one of 5 known superfamilies: Class II cytokine receptor family (also known as the interferon receptor family) Introduction • Cytokine receptors Based upon amino acid sequence homology, receptors are usually classified as belonging to one of 5 known superfamilies: TNF receptor family Introduction • Cytokine receptors Based upon amino acid sequence homology, receptors are usually classified as belonging to one of 5 known superfamilies: Chemokine receptor family Introduction • Cytokine receptors Introduction • Cytokine receptors Individual members of any one superfamily characteristically display 20–50 per cent homology In some cases a single receptor may contain domains characteristic of two or more superfamilies. e.g. IL-6: both the haematopoietic and immunoglobulin superfamilies Some cytokine receptors are composed of a single transmembrane polypeptide (e.g. receptors for IL-8, -9 and -10). Many contain two polypeptide components (including the IL-3, -4, and -5 receptors), and a few contain three or more polypeptide components (e.g. the IL-2 receptor contains three polypeptide chains) In some instances a single cytokine may be capable of initiating signal transduction by binding two or more distinct receptors (e.g. IL-1 has two distinct receptors (types I and II), both of which are transmembrane glycoproteins). Introduction • Cytokine receptors – In many cases where a receptor consists of multiple polypeptides, one of those polypeptides (which will be unique to that receptor) will interact directly with the ligand. The additional polypeptide(s), responsible for initiation of signal transduction, may be shared by a number of receptors. Leukaemia inhibitory factor (LIF) Introduction • Cytokines as biopharmaceuticals As coordinators of the immune and inflammatory response EPO in anemic person Growth factors and wound healing Neurotrophic factors in the abatement of certain neurodegenerative diseases Defeating certain viral pathogens: Cowpox: IL1 binding protein EBV: IL10 homologous protein Overproduction of certain cytokines Pro-inflammatory cytokines: IL6, IL8 and TNF: septic shock and rheumatoid arthritis Administration of mABs or soluble receptors The Interferons The Interferons The first family of cytokines to be discovered History: In 1957, researchers observed that susceptible animal cells, if they were exposed to a colonizing virus, immediately became resistant to attack by other viruses. This resistance was induced by a substance secreted by virally infected cells which was named interferon It has been shown that most species actually produce a whole range of interferons. Humans produce at least three distinct classes, IFN-α, IFN-β and IFN-γ. The Interferons • Biological Effects Induction of cellular resistance to viral attack Regulation of most aspects of immune function Regulation of growth and differentiation of many cell types Sustenance of early phases of pregnancy in some animal species No one interferon will display all of these biological activities Effects are initiated by the binding of the interferon to its specific cell surface receptor present in the plasma membrane of sensitive cells The Interferons • IFN-α and INF-β Significant amino acid sequence homology (30 per cent) Bind to the same receptor Induce similar biological activities Acid stable IFN-α and IFN-β are sometimes collectively referred to as type I interferons, or acid-stable interferons. IFN-γ Type II interferon The Interferons • Producer cells The Interferons • Medical conditions in which IFNs could be used: Augmentation of the immune response against infectious agents (viral, bacterial, protozoal, etc.) Treatment of some autoimmune conditions Treatment of certain cancer types The Interferons • The biochemistry of interferon-α In human, 24 related genes or pseudo-genes, code for the production of at least 16 distinct mature IFN-αs 15 type I: 166 aa, 1 type II: 172 aa 23 aa Signal peptide Predicted mass of 19-20 kD, but observed up to 27 kD (why?): 70% aa homology, Rich in leucine and glutamic acid Conserved cysteines (usually at positions 1, 29, 99 and 139), two disulfide bonds Each have an identifying name: In most cases the names were assigned by placing a letter after the ‘α’ (i.e. IFN-αA, IFN-αB, etc.) Some exceptions exist which contain a number or a number and letter, e.g. IFN-α7, IFN-α8, IFN-α2B. To ensure total confusion, several are known by two different names, e.g. IFN-α7 is also known as IFN-αJ1 The Interferons • The biochemistry of interferon-β Normally produced by fibroblasts The first interferon to be purified. In human, a single IFN-β molecule 166 aa 30 per cent sequence homology to IFN-αs A single disulfide bond Glycoprotein of molecular mass in excess of 20 kDa: N-gly, Asn 80 The Interferons • The biochemistry of interferon-γ “Immune” interferon Initially purified from human peripheral blood lymphocytes Is produced predominantly by lymphocytes IL-2 and -12, can induce IFN-γ production under certain circumstances 143 aa No significant sequence homology to type I family Predicted mass of 17 kD, but observed three bands: 16-17, 20 and 25 (Why?): N-gly, Asn 25, 97 Its biologically active form appears to be a homodimer in which the two subunits are associated in an antiparallel manner The Interferons • The interferon receptors: type I IFN receptors Two type I interferon receptor polypeptides Belonging to the class II cytokine receptor family Both are transmembrane N-linked glycoproteins α/β: capable of binding all type I interferons αβ: specific for IFN-α-B (a specific member of the IFN-α family) Present on most cell types The Interferons • The interferon receptors: type II IFN receptors The IFN-γ receptor More limited cellular distribution a transmembrane glycoprotein of molecular mass 50 kDa Function as a homodimer The extracellular IFN-γ binding region consists of approximately 200 amino acid residues AF-1 (accessory factor 1, a transmembrane glycoprotein) associates with the extracellular region of the receptor The Interferons • The interferon receptors: type II IFN receptors Cell types which display an IFN-γ receptor on their surface The Interferons • Interferon signal transduction The intracellular events triggered upon binding of type I or II interferons to their respective receptors are quite similar The JAK–STAT pathway signal transducers and activators of transcription (STAT1-STAT6) Janus kinases: Janus, a Roman god with two faces: two potential active sites The Interferons • The JAK–STAT pathway Ligands which, upon binding to their cell surface receptors, are known to promote activation of one or more STATs. (The STATs activated are also shown.) The Interferons • The JAK–STAT pathway The Interferons • The biological effects of interferons: Type I IFNs: Antiviral activity Anti tumor effects Anti-proliferative effect by increasing NK and T-cytotoxic cell activity The Interferons • The biological effects of interferons: Type I IFNs: Antiviral activity 2–5 oligoadenylate synthetase (2,5-An synthetase) and the eIF-2α protein kinase. (A) The OAS/RNase L system, an innate immunity pathway that acts against viral infections. Silverman R H J. Virol. 2007;81:12720-12729 The Interferons • The biological effects of interferons: IFN-γ: Weak antiviral and anti-proliferative activity Potentates the IFN-α/β activities Regulating most aspects of the immune and inflammatory responses main macrophage-activating factor Destruction of invading microorganisms; Destruction of intracellular pathogens; Tumour cell cytotoxicity; Increased major histocompatibility complex (MHC) antigen expression, leading to enhanced activation of lymphocytes via antigen presentation The Interferons • The biological effects of interferons: IFN-γ: Binding to its receptor on Neutrofils increasing in expression of a surface protein capable of binding to Fc portion of IgG Direct modulation of immune responses by affecting growth, differentiation and function of both T- and B-cells The Interferons • Interferon Biotechnology The antiviral and anti-proliferative activity of interferons, as well as their ability to modulate the immune and inflammatory response renders obvious their potential medical application Large-scale purification from sources such as blood was non-viable. Interferons exhibit species preference and, in some cases, strict species specificity. Transfused blood supplies: only 1% pure Mammalian cell culture: cancer cell lines; the namalwa cell line (8000 L) +sendai virus Recombinant DNA technology E. coli Fungi Yeast Some mammalian cell lines, such as CHO cell lines and monkey kidney cell lines The Interferons • Interferon Biotechnology The Interferons • Medical uses of interferon-α Anti cancer agent Breast cancer Certain lymphomas (malignant tumour of the lymph nodes) Multiple myeloma (malignant disease of the bone marrow) Delay recurrence of tumour growth after surgery in osteogenic sarcoma (cancer of connective tissue involved in bone formation) Approved indications of different INF-αs: rhIFN-α2a and -α2b (Intron A): Hairy cell leukemia More than 16 medical conditions The Interferons • Medical uses of interferon-α Antiviral agent: Mostly approved for viral hepatitis PEGylated interferons PEG IntronA (Pegylated rhIFN-α2b): HCV Viraferon Peg (Pegylated rhIFN-α2b): HCV PEGasys (Pegylated rhIFN-α2a): HCV Synthetic Interferon: Infergen (interferon alfacon-1 or consensus interferon): The most frequently occurring amino acid residue in each corresponding position of the native interferons Cloning and expression of the synthesized coding sequenceby E. coli Approved for Hepatitis C When compared on a mass basis, the synthetic interferon displays higher antiviral, antiproliferative and cytokine-inducing activity than do native type I interferons. The Interferons • Medical uses of interferon-β Relapsing–remitting multiple sclerosis (MS) Betaferon (rIFN-β-1b, mutated form: C17S): E. coli Betaseron (rIFN-β-1b, mutated form: C17S): E. coli Avonex (rhIFN-β-1a): CHO Rebif (rhIFN-β-1a): CHO Cinnovex (Iran, (rhIFN-β-1a)) Mechanism of action: Perhaps by inhibiting the production of IFN-γ and TNF-α and hence mediating downregulation of the pro-inflammatory responses against the myelin sheath The Interferons • Medical uses of interferon-γ Chronic granulomatous disease (CGD) Phagocytic cells are poorly capable/incapable of ingesting or destroying infectious agents such as bacteria or protozoa Healthy phagocytes produce highly reactive oxidative substances, such as hydrogen peroxide and hypochlorous acid, via a multicomponent NADPH oxidase system, which are lethal to pathogens CGD: a genetic defect in any component of this oxidase system NADPH oxidase system The Interferons • Medical uses of interferon-γ The recombinant human IFN-γ produced in E. coli: termed IFN-γ1b (Actimmune) A potent activator of phagocytes Potentiates their ability to generate toxic oxidative products As long as the genetic defect has not totally inactivated a component of the system, it promotes increased synthesis of these oxidative substances Promotes increased expression of IgG Fc receptors on the surface of phagocytes Destroy opsonized infectious agents via phagocytes The Interferons Increased expression of IgG Fc receptors on phagocytes results in enhanced phagocytosis. These receptors will retain opsonized (i.e. antibody-coated) infectious agents at their surface by binding the Fc portion of the antibody. This facilitates subsequent phagocytosis The Interferons • Interferon toxicity Like most drugs, administration of interferons can elicit a number of unwanted side effects In some instances the severity of such effects can limit the maximum recommended therapeutic dose to a level below that which might have maximum therapeutic effect The common adverse effect between the different IFNs is Flu-like symptoms Fever Headache Chills The Interleukins The Interleukins • General aspects The interleukins represent another large family of cytokines at least 36 different constituent members Most of these polypeptide regulatory factors are glycosylated (a notable exception being IL-1) and display a molecular mass ranging from 15 to 30 kDa (IL-9: heavily glycosylated, 40 kD) Most of the interleukins are produced by a number of different cell types IL-1 17 different cell types, IL-8 at least 10 different cell types IL-2, IL-9 and IL-13 produced only by T- lymphocytes The Interleukins • General aspects Most cells capable of synthesizing one interleukin are capable of synthesizing several, and many prominent producers of interleukins are non-immune system cells In most instances, induction or repression of any one interleukin is prompted by numerous regulators (mostly additional cytokines) IL-1 promotes increased synthesis and release of IL-2 from activated Tlymphocytes It is highly unlikely that cells capable of synthesizing multiple interleukins concurrently synthesize them all at high levels The Interleukins • General aspects Nearly all of the interleukins are soluble molecules (one form of IL-1 is cell associated) Their biological response is induced by binding to specific receptors on the surface of target cells Most interleukins exhibit paracrine activity Some display autocrine activity : IL-2 Some interleukins display more systematic endocrine effects: IL-1 The Interleukins Signal Transduction: Tyrosine phosphorylation Serine and threonine residues of specific intracellular substrates are also phosphorylated Promoting an increase in intracellular calcium concentration Inducing hydrolysis of phosphatidylethanolamine with release of diacyl glycerol The Interleukins • General aspects Many cell types are capable of producing a whole range of interleukins T-lymphocytes are capable of producing all the interleukins, with the possible exception of IL-7 and IL-15. Many cell types producing multiple interleukins can also produce additional cytokines For example, both macrophages and fibroblasts are capable of producing several interleukins, CSFs and PDGF. The Interleukins • Biological effects Interleukins regulate a variety of physiological and pathological conditions, including: Normal and malignant cell growth; All aspects of the immune response; Regulation of inflammation. 6 interleukin-based products have gained approval for general medical use Proleukin: an IL-2 Neumega: an IL-11 Kineret: anti IL-1 Ustekinumab: anti IL-12 and IL23 Reslizumab: Anti IL-5 Secukinumab: anti IL-17A Ontak: DT-IL2 immunotoxin The Interleukins • Interleukin-2 known as T-cell growth factor The first T-cell growth factor to be identified It is produced exclusively by T-lymphocytes (especially T-helper cells), in response to activation by antigen and mitogens A single-chain glycoprotein containing 133 amino acids The mature molecule displays a molecular mass ranging from 15 to 20 kDa The carbohydrate moiety is not required for biological activity O-gly to 3rd Thr The Interleukins • Interleukin-2 Receptor The high-affinity receptor complex consists of three membrane-spanning polypeptide chains (α, β and γ) The α chain binds IL-2 with low affinity The γ subunit does not interact directly with IL-2: γc (common): IL-4, 7, 9, 13 and 15 αγ or βγ can bind IL-2 with intermediate affinity The heterotrimeric αβγ complex represents the cytokine’s true high-affinity receptor Prolonged elevated levels of IL-2 promote the shedding of the IL-2 receptor α subunit from the cell surface The Interleukins • Interleukin-2 Receptor The IL-2 receptor is associated with a number of cell types, mainly cells playing a central role in the immune response Binding of IL-2 to its receptor induces growth and differentiation of these cells Lymphokine Activated Killer The Interleukins • Interleukin-2 Receptor Quiescent T-lymphocytes are stimulated largely by direct binding to an antigen fragment presented on the surface of a macrophage in the context of MHC complex: This results in the induction of expression of at least 70 genes whose products are collectively important in immune stimulation The Interleukins • Interleukin-2 Receptor Several cytoplasmic proteins capable of inducing T-cell growth (i.e. several cellular protooncogenes, including C-fos and C-myc). Various cytokines, most notably IL-2. Cytokine receptors, most notably the IL-2 receptor α subunit. (The T-lymphocytes appear to constitutively express the β and γ IL-2 receptor polypeptides. Induction of the α gene leads to formation of a high-affinity αβγ receptor complex, thereby rendering the activated T cell highly sensitive to IL-2) The Interleukins • Interleukin-2 Biological Activities IL-2 acts as a critical autocrine growth factor for T-cells, and the magnitude of the T-cell response is largely dependent upon the level of IL-2 produced IL-2 serves as a growth factor for activated B-lymphocytes. In addition to promoting proliferation of these cells, IL-2 (as well as some other interleukins) stimulates enhanced antibody production and secretion humoral immune response IL-2 promotes the growth and differentiation of NK cells: lymphokine activated killer (LAK) cells (with an enhanced ability to kill tumour cells or virally infected cells directly). NK cells express the β and γ IL-2 receptor subunits only: elevated concentrations of IL-2 is required The Interleukins • Interleukin-2 Clinical Applications Cancers T-cell and other forms of immunodeficiency Infectious diseases The Interleukins • Interleukin-2 production Sources of production Jurkat leukemia cell line Proleukin: E. coli Non-gly Lacks N-terminal Ala C125S The Interleukins Whatever the exact nature of tumour escape, it has been demonstrated, both in vitro and in vivo, that immunostimulation can lead to enhanced tumor detection and destruction. • Interleukin-2 and cancer treatment Cancer Specific antigens: Novel surface antigens not expressed by normal cells Greatly elevated levels of certain antigens present normally on the cell at extremely low levels. so low that they have escaped immunological tolerance In this regard, both a humoral and cell-mediated response can be induced, although the T-cell response appears to be the most significant The Interleukins Whatever the exact nature of tumour escape, it has been demonstrated, both in vitro and in vivo, that immunostimulation can lead to enhanced tumour detection and destruction. • Interleukin-2 and cancer treatment Some transformed cells obviously display characteristics that allow them to evade this immune surveillance: Most transformed cells do not express class II MHC molecules and express lower than normal levels of class I MHC molecules Some tumor-specific surface antigens resemble normal surface antigens or were expressed previously during the neonatal period and considered as “self” Some tumors secrete cytokines and additional regulatory molecules that can suppress local immunological activity: TGF-β The glycocalyx The Interleukins • Interleukin-2 and infectious diseases Numerous pathogens exist for which no effective treatment could be find Most of these pathogens are non-bacterial (e.g. viral, fungal and parasitic, including protozoal) capable of survival within macrophages: Mycobacteria (e.g. M. tuberculosis and M. leprae) Listeria monocytogenes (causes listeriosis which is characterized by flu-like symptoms, but can cause swelling of the brain and induce abortions) Legionella pneumophila (the bacterium that causes legionnaire’s disease) The immunological response raised against intracellular pathogens is largely a T-cell response. IL-2’s ability to stimulate T-cells may render it useful in the treatment of a wide range of such conditions The Interleukins • Inhibition of interleukin-2 activity A variety of medical conditions exist that are caused or exacerbated by the immune system itself: Autoimmune diseases Tissue/organ transplantation The Interleukins • Inhibition of interleukin-2 activity Selective immunosupression by preventing the synthesis or functioning of IL2: Cyclosporin A, one of the foremost immunosuppressive agents currently in use, functions by preventing IL-2 synthesis Administration of soluble forms of the IL-2 receptor Administration of monoclonal antibodies capable of binding the IL-2 receptor (without signal transduction activity) Administration of IL-2 variants that retain the ability to bind the receptor, but which fail to initiate signal transduction Administration of IL-2 coupled to bacterial or other toxins: Immunotoxins The Interleukins • Immunotoxins • Ontak (denileukin diftitox) The Interleukins • Immunotoxins The Interleukins • Interleukin-1 It is also known as lymphocyte-activating factor (LAF), endogenous pyrogen and catabolin Two distinct forms: IL-1α (membrane anchored) and IL-1β (soluble) 20% amino acid homology, different genes, but bind the same receptor Different cell types produce the different IL-1s in varying ratios • Fibroblasts and endothelial cells: similar ratios • IL-1β is produced in larger quantities than IL-1α in monocytes • Activated macrophages appear to represent the major cellular source for IL-1 The Interleukins • Interleukin-1 Two distinct receptors: Type I: fibroblasts, keratinocytes, hepatocytes and endothelial cells Type II: B-lymphocytes, bone marrow cells and polymorphonuclear leukocytes Both IL-1s could bind both receptor types The Interleukins • Interleukin-1 Biological Effects It is a pro-inflammatory cytokine: major biological function of IL-1 It plays a role in activating B-lymphocytes It acts as a co-stimulator of haematopoietic cell growth/differentiation Along with IL-6, it induces synthesis of acute-phase proteins in hepatocytes • These various biological activities depends largely upon the quantities of IL-1 produced in any given situation At low concentrations: paracrine, induction of local inflammation. At elevated concentrations: endocrine, inducing systematic effects, such as the hepatic synthesis of acute-phase proteins, induction of fever (hence the name, endogenous pyrogen) and general body wasting, such as that associated with some cancers The Interleukins • IL-1-like protein or IL-1 receptor antagonist (IL-1Rα) This molecule appears to be capable of binding to the IL-1 receptors without triggering an intracellular response Clinical application: Because of the IL-1 role in mediating acute/chronic inflammation, (downward) modulation of IL-1 levels may prove effective in ameliorating the clinical severity of these conditions anti-IL-1 antibodies soluble forms of the IL-1 receptor Native IL-1 receptor antagonist The Interleukins • IL-1-like protein or IL-1 receptor antagonist (IL-1Rα) Kineret: an approved product based on the latter strategy. Indicated in the treatment of rheumatoid arthritis rhIL-1 receptor antagonist 17.3 kD, E. coli, Non-gly, add. Met. The Interleukins • IL-11 Produced largely by IL-1-activated bone marrow stromal cells and fibroblasts functions as a haematopoietic growth factor It stimulates: Thrombopoiesis (the production of platelets formed by the shedding of fragments of cytoplasm from large bone marrow cells called megakaryocytes Growth/differentiation of bone marrow cells, derived from stem cells that have become committed to differentiate into macrophages The Interleukins The rationale for assessing IL-11 as a potential therapeutic agent relates mainly to its ability to induce platelet synthesis Neumega is the tradename given to the IL-11-based product approved for the prevention of thrombocytopenia Growth Factors: Haematopoietic growth factors 86 Oprelvekin Trade name: Neumega™ Approval Date: 1997 Description:The protein has a molecular mass of approximately 19kD, and is non-glycosylated. The polypeptide is 177 amino acids in length and differs from the 178 amino acid length of native IL-11 only in lacking the amino-terminal proline residue. This alteration has not resulted in measurable differences in bioactivity either in vitro or in vivo Production system: E. coli Dosage form: Single-use vials containing 5 mg of oprelvekin Therapeutic Indications: Is indicated for the prevention of severe thrombocytopenia and the reduction of the need for platelet transfusions following myelo-suppressive chemotherapy in adult patients with nonmyeloid malignancies who are at high risk of severe thrombocytopenia The Tumor Necrosis Factors The Interleukins • Tumour necrosis factor (TNF) Two types: α and β Bind to same receptor Induce very similar biological activities Display limited sequece homology Chromosome 6, adjacent, 1100bp distance The Interleukins • Tumour necrosis factor (TNF) TNF-α : macrophage cytotoxic factor, macrophage cytotoxin and necrosin As some of these names suggest, activated macrophages appear to represent the most significant cellular source of TNF-α Producer cells do not store TNF-α, but synthesize it de novo following activation Macrophages appear to express TNF-α mRNA constitutively, which is translated only upon their activation Monomeric TNF is biologically inactive; the active form is a homotrimer in which the three monomers associate non-covalently The Interleukins • Tumour necrosis factor (TNF) TNF-α: mostly studied, simply as TNF Sources of TNF-α: Inducers of TNF-α: The Interleukins • Biological Activities of TNF- α Activation of certain elements of both non-specific and specific immunity, in particular in response to Gram-negative bacteria Induction/regulation of inflammation Selective cytotoxic activity against a range of tumor cells Mediation of various pathological conditions, including septic shock, cachexia and anorexia The extent of the activity depends on the released amount: Low amount: locally, affecting WBCs and ECs High amount: Endocrine, is largely detrimental The Interleukins • TNF receptors 2 types: Type I; 55kDa (TNF-R55): more distributed, almost all cells Type II; 75 kDa (TNF-R75): restricted, most prominent on hematopoietic cells Both binds to both TNF types TNF-R55 and TNF-R75 Trimerisation following binding of the ligand to the receptor The Interleukins • Clinical Applications of TNF- α The initial interest in utilizing TNF as a general anti-cancer agent has diminished, largely due to the realization that: • Many tumours are not susceptible to destruction mediated by TNF (indeed, some tumours produce TNF as an autocrine growth factor) • Tumour cell necrosis is not TNF’s major biological activity • Severe side effects usually accompany systemic administration of therapeutically relevant doses of this cytokine Beromun™ (tasonermin): TNF-α-1a Soft Tissue Sarcoma (STS) in the limbs to prevent or delay amputation; Used in addition to melphalan The Interleukins • Clinical Applications of TNF- α Most clinical interest in TNF centers around neutralizing its biological effects in situations where overexpression of TNF induces negative clinical effects TNF has been firmly implicated in mediating many of the adverse effects associated with dozens of diseases The Interleukins • Clinical Applications of TNF- α Enbrel: an engineered hybrid protein consisting of the extracellular domain of the TNF p75 receptor fused directly to the Fc (constant) region of human IgG Enbrel functions as a competitive inhibitor of TNF, a major pro-inflammatory cytokine Binding of TNF to Enbrel prevents it from binding to its true cell surface receptors The antibody Fc component of the hybrid protein confers an extended serum half-life on the product, increasing it by fivefold relative to the soluble TNF receptor portion alone 96 Tumor Necrosis Factors TNF dependent drugs Etanercept Trade name: Enbrel™ Approval Date: 1998 Description: Enbrel (etanercept) is a dimeric fusion protein consisting of the extracellular ligand-binding portion of the human 75 kilodalton (p75) tumor necrosis factor receptor (TNFR) linked to the Fc portion of human IgG1. It consists of 934 amino acids and has an apparent molecular weight of approximately 150 kilodaltons Production system: E. coli Therapeutic Indications: Enbrel is indicated for reducing signs and symptoms, inducing major clinical response, inhibiting the progression of structural damage, and improving physical function in patients with moderately to severely active rheumatoid arthritis (RA). Enbrel can be initiated in combination with methotrexate (MTX) or used alone