* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A - Personal.psu.edu
Major urinary proteins wikipedia , lookup
Complement system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Molecular mimicry wikipedia , lookup
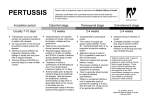
Common cold wikipedia , lookup
Urinary tract infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
DNA vaccination wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Hepatitis B wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Infection control wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Social immunity wikipedia , lookup
Vaccination wikipedia , lookup
Immunocontraception wikipedia , lookup
Neonatal infection wikipedia , lookup
Innate immune system wikipedia , lookup
Herd immunity wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
ABSTRACT Whooping cough can be caused by one of two bacterial pathogens, Bordetella pertussis or B. parapertussis. These two pathogens are very closely related and occupy the same host population, despite the fact that they are both highly infectious and cause acute, immunizing diseases. Since immunized hosts cannot be re-infected, at least for a period of time, it would be expected that cross reacting immunity would lead to immune-mediated competition that would displace one of these organisms from human populations. However, this is not what is observed with the bordetellae; both organisms are endemic in human populations, and occasionally can even be found in the same host at the same time. These observations, and the fact that B. pertussis immunization provides very little protection against B. parapertussis infection and disease, suggest there is imperfect cross immunity between these organisms. Since B. parapertussis appears to have emerged as a human pathogen more recently than B. pertussis, we hypothesize that B. parapertussis avoids B. pertussis-induced immunity both by altering or losing cross-reacting antigens and by manipulating host immunity. B. parapertussis is not well-studied, but appears to be increasing in incidence in human populations. Here we propose four aims to explore the biology of these competing organisms that has resulted in the emergence of B. parapertussis in B. pertussis-immune populations. Aim 1 will examine the mechanisms of immune clearance of B. parapertussis, as we have previously done with B. pertussis and B. bronchiseptica. Aim 2 will then quantify the levels and define the mechanisms of cross protection between B. pertussis and B. parapertussis. Aim 3 will examine the role of O-antigen as a decoy and/or shielding antigen protecting B. parapertussis from B. pertussisinduced immunity. This aim will also study the role of O-antigen as a protective antigen. These experiments will provide an understanding of the biology of B. parapertussis that will guide the health care response to this increasingly important pathogen. A. SCIENTIFIC AIMS The two human pathogens that cause the childhood disease, whooping cough, (Bordetella pertussis and B. parapertussis) have evolved from the animal commensal B. bronchiseptica. The specific aims outlined below target the ability of the two human pathogens to coexist in the same populations despite causing acute, immunizing infections. We hypothesize that the persistence of these closely related bacteria in the same host population requires mechanisms by which they may avoid reciprocal immunity. Despite being considered one of the etiological agents of whooping cough, B. parapertussis remains relatively unstudied compared to its sister subspecies, B. pertussis. Our recent work has begun to dissect the mechanisms of clearance of B. parapertussis. However, the ability of this bacterium to infect an immune host has not been well-characterized in experimental models. Additionally, B. parapertussis appears to have emerged as a human pathogen some time after B. pertussis, suggesting B. parapertussis invaded a population in which B. pertussis was already endemic. To do this, it is likely that this newly emerged subspecies was able to efficiently avoid immunity induced by B. pertussis. We have identified three specific aims that will use an experimental model to investigate the coexistence of these two respiratory pathogens and potential methods of curbing epidemics of B. parapertussis infections. Aim 1: Analyze the mechanisms of clearance of B. parapertussis from the respiratory tracts of immune hosts. This aim will determine the immune factors that are responsible for the elimination of this pathogen from mice that have been either vaccinated with whole-cell bacteria or previously infected with B. parapertussis. Aim 2: Examine the levels of reciprocal immunity between B. parapertussis and B. pertussis. This aim will focus in part on the ability of the human-specific bordetellae to colonize the respiratory tracts of hosts that have been previously infected or vaccinated with its sister subspecies. Additionally, the ability of B. pertussis and B. parapertussis to induce cellular and humoral immune responses to one another will be tested. 1 Aim 3: Uncover the mechanisms by which the human-specific bordetellae avoid immunity induced by each other. Focusing on key differences between the subspecies (such as the expression of O-antigen by B. parapertussis and the expression of pertussis toxin by B. pertussis), we will determine the virulence factors that aid the evasion of reciprocal immune responses and the protective antigens of B. parapertussis. B. BACKGROUND AND SIGNIFICANCE: The Bordetella genus. Members of the Bordetella genus are small, Gram-negative coccobacilli that colonize the respiratory tracts of their hosts, adhering to ciliated epithelia and spreading via respiratory droplets. B. pertussis is highly infectious in humans and is endemic throughout much of the world (1-2). This pathogen has received a great deal of attention from the scientific community due to its ramifications on human health. The disease caused by B. pertussis, whooping cough, is an acute, severe coughing illness that can progress to become spasmodic. Extreme cases may lead to regurgitation, convulsions, collapse, coma, and death (3). A closely related member of the Bordetella genus, B. parapertussis, causes a “whooping cough-like” disease, which is nearly indistinguishable from that caused by B. pertussis except for an acute lymphocytosis observed only in the latter (4). Disease caused by B. parapertussis is generally considered somewhat milder and shorter in duration compared to that caused by B. pertussis (5), but a large percentage of infections do results in symptoms of whooping cough (6). While cases of whooping cough may be attributed to either of the human-specific bordetellae, the similarities between the two bacteria make it difficult to pinpoint one or the other as the causative agent in a clinical situation. Recent estimates place the global burden of whooping cough at about 50 million cases per year and approximately 300,000 deaths (7). Despite vaccination programs, B. pertussis exists as an endemic pathogen, causing periodic epidemics (8). In fact, this bacterium has been increasing in prevalence in recent years in vaccinated populations (910). The epidemiology of B. parapertussis is not as well studied as that of B. pertussis and it is unclear what percentage of the estimated 50 million cases is caused by B. parapertussis. The relative frequency of B. parapertussis isolation from individuals diagnosed with whooping cough has been shown to vary widely depending on the population sampled (6). Separate studies have suggested that cases of whooping cough caused by this bacterium make up anywhere from below one percent to greater than 95 percent of all cases in populations around the world (6). The difficulties in differentiating between disease caused by B. parapertussis and that caused by B. pertussis greatly hinder the ability of epidemiologists to make a good estimate of relative ratios of each pathogen. Evolution of the bordetellae. The three classical bordetellae (B. pertussis, B. parapertussis, and B. bronchiseptica) have recently been reclassified as subspecies based on multi-locus enzyme electrophoresis and insertion sequence typing. B. bronchiseptica is a respiratory pathogen of a large number of mammalian species including dogs, pigs, rabbits, rats, and rhesus monkeys (11). This bacterium is rarely isolated from human hosts and most human cases of B. bronchiseptica infections are the result of an immunodeficiency (12). All three of the classical bordetellae are very closely related and share a number of virulence factors. In fact, B. parapertussis and B. pertussis are more similar to B. bronchiseptica than they are to each other. Based on genomic analyses, it is thought that both human-specific pathogens evolved independently from a B. bronchiseptica-like progenitor (13). B. pertussis was likely the first of the two currently-known human-specific bordetellae to emerge as a human pathogen. It is thought that B. parapertussis evolved to infect humans much more recently as isolates from anywhere in the world over the past 50 years are indistinguishable by a variety of genetic criteria (14). The current evolutionary and immunological theories suggest 2 that B. parapertussis invaded a human population in which B. pertussis was already endemic, and consequently, had a certain degree of immunity to B. parapertussis due to the antigens shared between it and B. pertussis. Thus, we have hypothesized that it is likely that B. parapertussis utilizes some mechanism to avoid immunity induced by B. pertussis. Past studies involving infection-induced immunity suggest that these two pathogens do confer protective immunity against one another (15); however, studies involving the B. pertussis vaccines have indicated otherwise. In experimental models, B. pertussis-specific vaccines protect much more efficiently against B. pertussis than they do against B. parapertussis (16-19). Currently, there is a lack of understanding of reciprocal immune responses between the two causative agents of whooping cough. Despite all the similarities between B. parapertussis and B. pertussis, immune responses that are specific to one of these pathogens may not necessarily protect against the other. Mouse model of Bordetella infections. Mouse models of infection have been used extensively for infections by the three classical bordetellae (20-24). B. bronchiseptica and B. parapertussis have very low infectious doses (< 100 CFU) (25) and B. pertussis is able to successfully establish infections of murine hosts with a slightly higher infectious dose (~103 CFU) (26). As B. parapertussis and B. pertussis are human-specific pathogens in nature (3), it has been questioned whether the mouse model is suitable to examine the interactions of these bacteria with their hosts. An inoculation strategy consisting of 5 x 105 CFU in 50 microliters of PBS pipetted onto the external nares of a lightly sedated mouse efficiently distributes bacteria throughout the respiratory tract (27). Both the colonization of the respiratory organs and clearance of the human-specific bordetellae from the respiratory tract in humans are mimicked in the experimental mouse model using this inoculum (28). Bacteria grow to high numbers during the first week and persist throughout the respiratory tracts of mice for 28 days or more (29). This delay in bacterial clearance is similar to time courses observed in humans (30). Similarly, the immune response induced by this inoculum is similar to that induced in human hosts upon infections by B. parapertussis or B. pertussis (31). Like humans, mice develop protective cellular and humoral immunity to both of these bacteria upon infection that ultimately result in the elimination of the bacteria from the respiratory tract (32). Thus, the ability of B. parapertussis and B. pertussis to colonize the respiratory tract and the immune response that mediates clearance of these pathogens are similar in both human and mouse hosts making the experimental mouse model suitable to study interactions of the human-specific bordetellae with its host. Immunity to the bordetellae. A great deal has been published on the mechanisms of protective immunity to the bordetellae, but our understanding remains rudimentary. Furthermore, knowledge of the mechanisms of protective immunity to B. parapertussis is greatly lacking compared to B. pertussis and B. bronchiseptica. Our lab has elucidated the mechanisms of clearance of B. bronchiseptica from the respiratory tract. Infected B cell-deficient mice are unable to reduce bacterial numbers, but these mice clear the infection from the lower respiratory tract within approximately three days upon an adoptive transfer of B. bronchiseptica-specific serum antibodies indicating that these antibodies are essential to the elimination of this bacterium (29). We have also shown that TLR4, neutrophils, complement component C3, complement receptor 3, and Fcγ receptors are required for this antibody-mediated clearance (33). The present model for the clearance of B. bronchiseptica from the lower respiratory tract involves the following: TLR4 is necessary for efficient neutrophil recruitment to the lungs early during an infection (34). These neutrophils are the phagocytic cells that are responsible for eliminating the bacteria from the respiratory tract, but in order to do so, the bacteria must be opsonized by complement component C3b and antibodies. Neutrophils then bind and phagocytose the coated bacteria via complement receptor 3 and Fcγ receptors. With this knowledge, we will be able to compare and contrast the mechanisms of clearance of this bacterium with those of the human-specific bordetellae. We have shown that B. pertussis and B. parapertussis are also eliminated from the respiratory tract via an antibody-dependent route (29,35-36). That being said, the antibody-mediated clearance of these two pathogens is 3 delayed in comparison to that of B. bronchiseptica (29,35-36). By understanding the immune factors that mediate the elimination of B. bronchiseptica from the respiratory tract, we have been able to hypothesize about the ways by which the human-specific bordetellae inhibit antibody-mediated clearance. Neutrophils are essential to the antibody-mediated clearance of B. bronchiseptica (33) and the pertussis toxin of B. pertussis inhibits neutrophil migration to the lungs (37). Thus, we hypothesized that B. pertussis avoids rapid antibody-mediated clearance by inhibiting the recruitment of neutrophils to the site of infection. This does indeed appear to be the case. B. pertussis is normally eliminated from the lower respiratory tract within approximately 14 days upon an adoptive transfer of serum antibodies (35). However, an infection by a B. pertussis strain lacking pertussis toxin is accompanied by higher numbers of neutrophils in the lungs in the first few days post-inoculation compared to a wild type strain and is rapidly cleared from the respiratory tract by antibodies (35). In addition, antibodies did not rapidly clear the pertussis toxin-deficient strain when neutrophils were depleted via an intraperitoneal injection of anti-Ly-6G antibodies suggesting that the recruited neutrophils mediate bacterial clearance (35). By inhibiting the influx of neutrophils to the site of infection, pertussis toxin allows B. pertussis to persist in a host in which high titers of Bordetella-specific antibodies are present. This also supports the theory that pertussis toxin enables B. pertussis to re-infect immune hosts, allowing its persistence in the human population. Although B. parapertussis does not express a functional pertussis toxin (38), this bacterium is also able to avoid rapid antibody-mediated clearance from the respiratory tract (36). Since the vast majority of experimental studies have focused on B. bronchiseptica and B. pertussis, there is relatively little known about immunity to B. parapertussis. Our recent work has begun to focus on this pathogen and has showed that neutrophils, CD4+ T cells, and complement are required for the antibody-mediated clearance of B. parapertussis (36). These essential immune factors are similar to those necessary for antibody-mediated clearance of B. bronchiseptica with the exception of T cells. It appears that neutrophils phagocytose and kill B. parapertussis that is coated by complement and antibodies, but this does not occur until T cell responses are generated. CD4+ T cells play a yet unidentified role in the elimination of B. parapertussis from the respiratory tract, but one hypothesis is that they provide essential pro-inflammatory stimuli upon an infection. The LPS of B. parapertussis does not efficiently stimulate TLR4 signaling and little cellular influx is observed early in an infection by this pathogen (34). We have hypothesized that T cells are necessary for signaling to recruit sufficient amounts of neutrophils to eliminate B. parapertussis from the lower respiratory tract of its host. There is little known about the ability of B. parapertussis to persist in a host that is “immune” or the mechanisms by which it does so. Immunity to B. pertussis wanes over time allowing the re-infection of previously vaccinated or infected hosts (39), but it is unclear if this is also the case for B. parapertussis. The ability of B. parapertussis to colonize immune hosts has not been well-studied, but clinical studies suggest that this subspecies is capable of infecting individuals that have previously been vaccinated or infected (40). Despite the similarities between the human-specific bordetellae, it does not appear that the current B. pertussis vaccines confer efficient protection against its sister subspecies. It has been estimated that B. pertussis vaccines are 72 to 93% effective in preventing B. pertussis disease, but are only approximately 31% effective against B. parapertussis (19). Vaccine studies in an experimental model support the idea that B. pertussis vaccine-induced immunity does not efficiently protect against B. parapertussis infections (16-19). Thus, infections of B. pertussis-immune hosts by B. parapertussis may occur even prior to immunity waning in these individuals. In view of the fact that B. parapertussis causes a disease that is nearly indistinguishable compared to that caused by B. pertussis, there is a great lack of knowledge regarding protective immune responses to this bacterium. Epidemiology of B. parapertussis. In comparison to B. pertussis, very little is known about the prevalence of B. parapertussis in the human population. It has been diagnosed as the causative agent of whooping cough anywhere from less than 1 percent to 4 greater than 95 percent of cases (6). This bacterium has also been found to be present at levels greater than 1 percent in randomly sampled populations (41). Though many countries do not report a high number of cases of B. parapertussis, that does not necessarily mean that this bacterium is not abundant in the human population. Many cases of whooping cough may be diagnosed as B. pertussis infection. Medical personnel do not take the time and effort to differentiate between the two human-specific bordetellae. Additionally, a large number of B. parapertussis infections go unreported. Recent estimates involving B. pertussis infections place the percentage of infections that are reported is very low. Seroprevalence data has suggested that B. pertussis may infect as much as six percent of the population every year despite the rate of diagnosis of B. pertussis infections being only 0.01 percent (42). The percentage of B. parapertussis infections that are actually reported may even be lower as disease caused by this bacterium is generally thought to be milder (5). Therefore, the actual prevalence of B. parapertussis may be much higher than it is thought. Thus, the actual rate of B. parapertussis infections could approach the same level, but many may go undiagnosed. There have only been a few studies involving the surveillance of B. parapertussis abundance in a population over time, but they show that the prevalence of this pathogen may be on the rise. This increase in the numbers of cases of whooping cough attributed to B. parapertussis may be due to more careful diagnoses of patients; or it may signify a selective pressure provided by B. pertussis vaccines for strains that are antigenically distinct from the vaccine strains. In support of this, B. pertussis strains were of a particular antigenic type prior to the vaccine era, but new B. pertussis strains have emerged since the introduction of vaccines. These strains, like B. parapertussis have increased in prevalence over the years since vaccines were established (43). This raises the possibility that B. parapertussis could ultimately displace B. pertussis as the predominant etiological agent of whooping cough. The continued selective pressure of a vaccine that is specific for B. pertussis but ineffective against B. parapertusssis could eventually lead to the latter becoming increasingly abundant. That being said, B. parapertussis vaccines have been used in the past in order to curb epidemics by this pathogen (44). The addition of protective B. parapertussis antigen(s) to current B. pertussis vaccines would limit the threat of epidemics by both pathogens. B. parapertussis paradox. Epidemiological theory holds that if two closely related, immunizing pathogens occupy the same host population, the more virulent of the two will displace the other assuming it is not so virulent as to cause violent and unstable epidemics (45). This is consistent with the known biology of B. bronchiseptica, which is endemic in many different mammalian species but usually only infects humans with little immunity to B. pertussis (12). The existence of B. parapertussis creates a paradox to the theory that B. bronchiseptica was replaced by more virulent, cross-reactive strains in the human population. B. parapertussis and B. pertussis are closely related; thus, if they induce crossprotective immunity, competition should cause the exclusion of one of them. Disease caused by B. pertussis is generally thought to be a little more severe and longer-lasting than that caused by B. parapertussis (5). Because of this, it could be assumed that B. pertussis would be transmitted at a higher rate, immunize a higher proportion of the population, and eliminate B. parapertussis from the human population. Yet B. parapertussis likely invaded a human population in which B. pertussis was already endemic, and the two strains appear to be coexisting quite stably. Phylogenetic analysis shows that B. parapertussis adapted to humans relatively recently, consistent with the nearly clonal identity between B. parapertussis isolates from anywhere in the world over the past 50 years (14). Since estimates place the adaptation of B. pertussis to humans before that of B. parapertussis, the latter invaded a human population in which a degree of immunity to B. pertussis had already existed. Thus, B. parapertussis likely utilizes some mechanism to avoid immune-mediated cross protection. There is substantial epidemiological evidence that this is indeed the case, at least in terms of vaccine induced immunity (16,18,46), and experimental studies have supported this hypothesis (17,19). Despite the abundance of similarities between the two human pathogens, B. pertussis does not appear to induce efficient immune responses to B. parapertussis. 5 Although closely related, there are a few striking differences among the classical bordetellae. B. parapertussis expresses an O-antigen that is the dominant surface antigen of the bacterium and could shield other surface antigens from immune recognition. This may explain the low levels of B. parapertussis-specific antibodies produced upon infection or vaccination with B. perussis (15). In addition, B. parapertussis has mutations in the gene for pertussis toxin, causing a lack of expression of this virulence factor. Given that pertussis toxin is crucial for an efficient infection process by B. pertussis (35,37), the forfeit of this potent weapon by B. parapertussis is somewhat confusing. Our evolutionary model provides a potential explanation: In adapting to a human population in which B. pertussis was endemic, selection would greatly favor strains with minimal cross-reactivity with the prevalent B. pertussis strains. Consistent with this, there are substantial changes in some of the commonly expressed antigens when comparing the two subspecies (47). We hypothesize that immunity to B. pertussis in the human population provided selective pressure for the loss of pertussis toxin expression by B. parapertussis, as well as the maintenance of O-antigen by this subspecies. The model above leads to several predictions regarding the effects of B. pertussis-induced immunity on B. parapertussis infections. These predictions will be tested in Aims 2 and 3 below. We plan to use our experimental mouse model and bacterial mutants to test two hypotheses involving evolution of the human-specific bordetellae: (i) B. parapertussis retains the expression of O-antigen in order to shield B. pertussis cross-reacting surface antigens and (ii) expression of pertussis toxin by B. parapertussis would subject it to increased levels of B. pertussis-induced immunity. These studies may provide insight to the independent evolution of two closely related organisms to utilize the same host population. In depth studies of B. parapertussis and its mechanisms of avoiding host immune responses will give us valuable information regarding the evolution of this genus and the ability of a bacterial species to evolve to avoid adaptive immune responses. Questions, Significance, and Approach. A few recent clinical and laboratory studies have focused on reciprocal protection, either infection- or vaccineinduced, between the two human-specific bordetellae (15,19). The incidence of B. parapertussis in highly vaccinated populations may be on the rise (48), and this will likely be compounded by the introduction of acellular B. pertussis vaccines, which have been shown to be less effective against B. parapertussis than whole-cell vaccines (16). Together these observations suggest that current vaccination programs and the ability of B. parapertussis to avoid immunity induced by its sister subspecies may allow B. parapertussis to continue increasing in prevalence over the years and possibly to gradually replace B. pertussis in the human population. The characterization of protective immunity against B. parapertussis, as well as mechanisms by which this bacterium avoids host immune responses, will significantly advance the understanding of the unique evolutionary pathway that B. parapertussis has used to coexist with B. pertussis. This understanding will provide a basis for more informed and effective strategies to control the spread of B. parapertussis. Additionally, this study will provide key information as to what protective antigens of B. parapertussis could be added to vaccination protocols. C. PRELIMINARY STUDIES: C1. Elimination of B. parapertussis from the murine respiratory tract. 1. Neutrophils, CD4+ T cells, and complement are required for the antibody-mediated clearance of B. parapertussis from the lower respiratory tract. We have previously published an analysis of the role of antibodies, including showing that they are required for clearance of all three classical bordetellae (29) and are effective in clearing all three from the lower respiratory tract, although the timeline differs strikingly (29,35-36). Adoptively transferred antibodies completely eliminate B. 6 bronchiseptica within three days of inoculation (29). Although antibodies have no effect on the numbers of B. pertussis or B. parapertussis in this time frame, they are very effective in clearing these organisms between days 7 and 14 post inoculation (35-36). The lack of early effect led us to conclude that the human adapted pathogens have mechanisms to avoid rapid antibody-mediated clearance that B. bronchiseptica is lacking. Our work has elucidated a more detailed mechanism of antibody-mediated clearance of B. bronchiseptica that requires complement, Fc receptors, TLR4 signaling, and neutrophils (33). We have also shown that B. pertussis inhibits the process of antibodymediated clearance by preventing neutrophil recruitment to the lungs via pertussis toxin (35). We therefore set about to determine the mechanism by which antibodies clear B. parapertussis, under the presumption that upon a comparison with B. bronchiseptica, we will be able to speculate how B. parapertussis avoids rapid antibody-mediated clearance, as we have done successfully with B. pertussis. Using specific immuno-deficient mouse strains and mice depleted of individual immune factors, we have determined that complement, CD4+ T cells, and neutrophils are required for the antibody-mediated clearance of B. parapertussis (36). This suggests a model in which bacteria are coated by C3b and antibodies and subsequently phagocytosed by neutrophils after T cell responses have been induced. This leaves the role of T cells in bacterial clearance uncharacterized, but additional work is in progress to determine the function of T cells in the antibodymediated clearance of B. parapertussis. 2. B. parapertussis may avoid rapid antibody-mediated clearance from the respiratory tract by not inducing leukocytosis to the lungs. B. pertussis appears to avoid rapid antibody-mediated clearance via the expression of pertussis toxin. This toxin inhibits the downstream effects of G-protein coupled receptors including many chemokine receptors (49). A strain of B. pertussis lacking pertussis toxin induced a higher level of neutrophil infiltration to the lungs compared to a wild type strain and was rapidly cleared upon adoptive transfer of serum antibodies (35). Upon the depletion of neutrophils, the clearance of the strain lacking pertussis toxin was not observed indicating that the increased neutrophil migration to the lungs in the absence of pertussis toxin correlated with the increased rate of clearance (35). Interestingly, B. parapertussis does not express this toxin but still is not cleared until day 14 upon an adoptive transfer of serum antibodies. In our early studies with B. parapertussis, we have observed that the lungs of B. parapertussis-infected mice do not appear to be inflamed to a significant degree despite being colonized by millions of bacteria. Additionally, its LPS does not efficiently stimulate TLR4 signaling; approximately 100-fold as much B. parapertussis LPS, compared to B. bronchiseptica LPS, is required to stimulate similar amounts of cytokine production by RAW cells in vitro (34). Additionally, there is a large TLR4-dependent peak in cellular influx that is mostly comprised of neutrophils early in a B. bronchiseptica infection that is absent in B. parapertussis infections (34). Since B. pertussis avoids rapid antibody-mediated clearance by inhibiting the migration of neutrophils to the lungs, we hypothesized that the same may be true of B. parapertussis. However, we believe that B. parapertussis does not inhibit cellular infiltration via toxins, but simply does not induce high levels of cellular responses to the lungs during the first week of an infection. 3. Summary. We have characterized the antibody-mediated clearance of B. parapertussis from the murine lung. In doing so, we have found that the mechanism of bacterial elimination is similar to that of B. bronchiseptica with the exceptions of the delayed clearance and the requirement of CD4+ T cells. In comparison to the elimination of B. pertussis from the lower respiratory tract, both T cells and neutrophils are necessary for protection against the human-specific bordetellae, but the role of T cells is as of yet unidentified. We have hypothesized that T cells are responsible for efficient induction of neutrophil responses to B. parapertussis. They may provide pro-inflammatory signals such as IFN or 7 other chemokines that allow for a higher level of neutrophil migration. In addition, T cells may produce cytokines that activate the neutrophils in the lungs to phagocytose and kill B. parapertussis. In support of this model, vaccinated or previously infected mice (in which both strong cellular and humoral responses to B. parapertussis are present) clear an infection much more quickly relative to those given an adoptive transfer of B. parapertussis-specific antibodies. Therefore, it is likely that some T cell function aids the rapid clearance of B. parapertussis from the lungs, either by facilitating neutrophil activation or recruitment to the site of infection. C2. PRELIMINARY DATA IN SUPPORT OF SPECIFIC AIM 1: Analyze the mechanisms of clearance of B. parapertussis from the respiratory tracts of immune hosts. 1. Antibodies and αβ T cells are essential to protection against B. parapertussis infection of naive hosts. B. parapertussis causes an acute infection of the respiratory tract in humans. The time course of infection is similar in the murine model except for the fact that the nasal cavity is persistently colonized for the life of the animal (29). The lower respiratory tract, however, is nearly cleared of bacteria within 28 days (29,36). Adaptive immune responses are essential to the elimination of the bacteria (36,50), and although multiple studies have shown that adaptive immunity is important to the control of B. parapertussis, the immune responses that mediate the elimination of this pathogen have gone relatively uncharacterized. Our recent studies have shown that both antibodies and αβ T cells are required for the efficient reduction of bacterial numbers in the lower respiratory tract. Interestingly, IgA, the predominant antibody isotype of mucosal surfaces, is not required for the elimination of this extracellular mucosal pathogen (36). 8 2. B. parapertussis infections are cleared rapidly from convalescent or vaccinated mice. 7 Log CFU 6 5 Our work has indicated that T cells, neutrophils, and complement are 4 required for the function of antibodies against B. parapertussis (36). 3 Although essential to clearing the infection, antibodies alone are not 2 sufficient to clear this pathogen from the lungs (36). The fact that T 1 cells are necessary for antibody function suggested that a more complete 0 immunization, relative to the adoptive transfer model, may allow for faster clearance of B. parapertussis. Upon testing the effects of infection-induced immunity on an infection, we have determined that this is true for B. parapertussis. An infection was cleared from the lower respiratory tract within approximately three days from convalescent animals. Similarly, B. parapertussis was rapidly eliminated from the lower respiratory tract of mice vaccinated with heat-killed B. parapertussis (Fig. 1). These data suggest that inducing both T cell responses and Bordetella-specific antibodies allows for rapid control of this bacterium. This leaves the role of T cells in mediating rapid antibody-mediated clearance to be uncovered. Naïve Convalescent Vaccinated Fig. 1: C57BL/6 mice (naïve, convalescent 28 days post-primary infection, or vaccinated with 2 doses of 108 heat-killed B. parapertussis at days 0 and 14) were inoculated with 5 x 105 CFU of B. parapertussis and bacteria in the lungs were quantified 3 days later. 3. αβ T cells and IFN-γ mediate efficient recruitment of leukocytes to B. parapertussis-infected lungs. 8 #of cells x 10^5 Log CFU 7 We have begun to look more in depth at the protective roles of T cells Naïve serum during infections by B. parapertussis. T cells are an important source of 6 Immune serum cytokine production in many infection models, and this may be a key 5 function of these cells in the clearance of this pathogen. We have 4 hypothesized that the role of T cells in the clearance of B. parapertussis 3 from the respiratory tract is the production of IFN, which has previously 2 been implicated as being crucial to protection against B. pertussis (51). 1 We have shown that T cells are essential to the function of B. 0 parapertussis-specific antibodies (36). Our preliminary data also shows C57 IFNg-/that this IFNis essential to the antibody-mediated clearance of B. parapertussisWhile wild type mice reduced bacterial numbers to nearly Fig. 2: C57BL/6 and IFN-/- mice were undetectable levels in the lungs by 14 days post-inoculation upon an adoptive -/inoculated with 5 x 105 CFU of B. transfer of serum antibodies, similarly treated IFNγ mice were unable to parapertussis and given an i.p. injection decrease the bacterial load in the lungs (Fig. 2). As a pro-inflammatory of 200 L of naïve serum or cytokine, the role of IFN in the antibody-mediated clearance of this convalescent serum from B. bacterium could involve the activation or recruitment of neutrophils, which parapertussis-infected mice. Bacteria in the lungs were quantified 14 days are essential to clearance (36), to the site of infection. Since B. parapertussis later. does not efficiently stimulate TLR4-mediated cytokine production (34), other signals may be required for sufficient neutrophil responses to the lungs. Therefore, we quantified the numbers of neutrophils at a time when bacterial numbers were similar in wild type, T cell-deficient, and IFNγ-deficient mice but begin to decline in wild type mouse strains soon thereafter. Both T cell-deficient (1 x 105) and IFNγ-deficient (0.2 x 105) mice appeared to be defective in recruiting neutrophils to the lungs compared to wild type mice (4 x 105) (Fig. 3) suggesting that the role of T cells in the antibody-mediated clearance of 6 B. parapertussis is to facilitate the migration of neutrophils to the lungs 5 via an IFN-dependent mechanism. 4. Summary. 4 3 2 While T cells are important in the clearance of B. parapertussis from naive animals (36), examining the role of these cells in bacterial 1 clearance from convalescent mice and vaccinated hosts is important to 0 understand the ability of this pathogen to infect immune hosts. In C57 TCRa -/IFNg -/addition to T cells, we plan to dissect the entire mechanism of clearance of B. parapertussis from "immune" hosts. This will be of Fig. 3: C57BL/6, TCR-/-, and IFN-/importance given that most of the world's population has been exposed to and mice were inoculated with 5 x 105 CFU infected by either B. parapertussis or B. pertussis (52) but are still capable of of B. parapertussis. Numbers of being re-infected by B. parapertussis (53). Aim 1 of this proposal will neutrophils in the lungs were quantified 7 days later. examine the mechanisms by which B. parapertussis is cleared from convalescent and vaccinated hosts and the roles of specific immune factors. In doing so, we hope to identify the immune responses that confer protection against B. parapertussis and ways by which this bacterium could subvert them, allowing the re-infection of hosts. C3. PRELIMINARY DATA IN SUPPORT OF SPECIFIC AIM 2: Examine the levels of reciprocal immunity between B. parapertussis and B. pertussis. 1. Infections and vaccinations with B. parapertussis and B. pertussis confer strong autologous protection. 9 Both of the human-specific bordetellae cause acute, immunizing infections in humans. B. parapertussis and B. pertussis induce strong cellular and humoral immune responses that are closely mimicked by the murine model. Additionally, the durations of infections by both subspecies are similar in naïve humans and mice. Upon analyzing the ability of the human-specific bordetellae to colonize convalescent or vaccinated hosts, it was observed that infections by B. parapertussis were cleared within approximately three days from the lungs of convalescent mice, and B. pertussis infections also conferred effective autologous immunity (Fig. 4). Similarly, vaccinations consisting of heatkilled B. parapertussis or B. pertussis efficiently protected against infections by themselves (Fig. 5). Thus, immune responses induced by both B. parapertussis and B. pertussis infection or vaccination are effective in rapidly clearing subsequent infections by the same species. Fig. 4: C57BL/6 mice were infected with B. parapertussis (Bpp) or B. pertussis (Bp) and 28 days later, reinfected with an antibiotic resistant Bpp or Bp strain. The x-axis indicates the primary infection, closed bars are secondary Bpp infections and open bars are Bp secondary infections. Bacteria were enumerated 3 days post-secondary infection. 2. An infection with B. pertussis does not confer protective immunity against B. parapertussis. Although it has been suggested that B. parapertussis- and B. pertussis-induced immune responses may be cross-protective (15), our preliminary studies have indicated otherwise. While we have observed that immunity induced by a primary infection of B. parapertussis is protective against both subspecies, immune responses to a primary B. pertussis infection only allowed for rapid clearance of B. pertussis. At three days post-inoculation, more than 105 CFU of B. parapertussis were found in the lungs of mice given a primary B. pertussis infection (Fig. 4). It has been hypothesized that B. parapertussis evolved from a B. bronchiseptica-like progenitor to invade a human population that may have had some degree of immunity to B. pertussis, suggesting that B. parapertussis would need to evade B. pertussis-induced immunity. This data supports the theory that B. pertussis infection does not induce efficient protection against infections by B. parapertussis, allowing the latter to invade the human 8 Bpp population. 7 Bp 3. Vaccinations with heat-killed B. parapertussis and B. pertussis do not confer protective immune responses to each other. Log CFU 6 5 4 3 Previous work in both epidemiological and experimental areas has shown 2 1 that B. pertussis-specific vaccines confer little, if any, protection against 0 B. parapertussis infections (16-19,46). Our preliminary studies showed this as well as vaccinations via i.p. injections of heat-killed B. pertussis did not efficiently protect against subsequent challenges with B. parapertussis (Fig. 5). Unlike infection-induced immunity, vaccine-induced immunity was not cross-protective for either subspecies. Mice vaccinated with heat-killed B. parapertussis were unable to significantly reduce numbers of B. pertussis in the lungs (Fig. 5). Since current vaccines appear to be ineffective against B. parapertussis, the continued omission of B. parapertussis antigens from vaccination protocols could eventually lead to selection for this bacterium in the human population via immune-mediated competition. The addition of 10 Naïve Bpp vaccinated Bp vaccinated Fig. 5: C57BL/6 mice were vaccinated with i.p. injections of 108 heat-killed B. parapertussis (Bpp) or B. pertussis (Bp) on days 0 and 14 and on day 28 were inoculated with 5 x 105 CFU of Bpp or Bp. Bacteria in the lungs were quantified 3 days later. protective B. parapertussis antigens to current pertussis vaccines would limit disease caused by both human-specific bordetellae. 4. Summary. Our preliminary data shows that a primary infection with B. parapertussis protects against both subsequent B. parapertussis and B. pertussis infections. However, we have observed that a primary B. pertussis infection does not efficiently protect against a secondary B. parapertussis infection. Interestingly, neither vaccination with whole-cell B. parapertussis or whole-cell B. pertussis was cross-protective. Aim 2 proposes to measure additional aspects of immune responses other than the ability of the bacteria to colonize the lungs. We plan to analyze both cellular and humoral immune responses to determine why infections and vaccinations are not cross-protective even though many antigens are common between the two human-specific pathogens. C4. PRELIMINARY DATA IN SUPPORT OF SPECIFIC AIM 3: Uncover the mechanisms by which the human-specific bordetellae avoid immunity induced by each other. 1. O-antigen aids the evasion of B. pertussis-induced immunity by B. parapertussis. Log CFU O-antigen is a prominent surface molecule of B. parapertussis that is not expressed by B. pertussis strains. This polysaccharide can inhibit complement-mediated killing and phagocytosis and is crucial to the infection process of a number of bacterial species (54-58). While almost no work has been done dealing with specific virulence factors of B. parapertussis, we have previously shown that this antigen is important to the establishment of an infection by B. parapertussis in a low dose inoculation strategy (54). However, upon a 7 high dose inoculation, a B. parapertussis strain lacking O-antigen was 6 able to efficiently colonize the respiratory tract (Fig. 6). Interestingly, unlike the wild type B. parapertussis strain, the O-antigen mutant was 5 rapidly cleared from mice that have been previously infected with B. 4 pertussis (Fig. 6), suggesting that O-antigen is required for B. parapertussis to avoid B. pertussis infection-induced immunity. 3 Evolving from B. bronchiseptica-like progenitors (which likely 2 expressed O-antigen), both of the human-specific bordetellae appear to 1 have lost a large number of genes (13). Thus, maintaining its O-antigen may have allowed B. parapertussis to invade and persist in a human 0 Naïve Primary Bp Primary Bpp Primary Bpp population in which B. pertussis was endemic. infection 2. The immune response to O-antigen protects against infections by B. parapertussis. 11 infection - O-ag Fig. 6: C57BL/6 mice were given a primary inoculation of 5 x 105 CFU of B. pertussis (Bp), B. parapertussis (Bpp), or B. parapertussis lacking Oantigen (Bpp-O-ag). Mice were reinoculated with 5 x 105 CFU of Bpp-Oag 28 days later and bacteria in the lungs were enumerated 3 days after that. Log CFU Our preliminary work has shown that O-antigen aids the evasion of B. pertussis-induced immunity by B. parapertussis (Fig. 6). We have also begun to examine the protective effects of immune responses to O-antigen on infections by B. 8 parapertussis. As this polysaccharide is a major surface molecule of 7 this bacterium, it was hypothesized that immunity to O-antigen would 6 be important to protection against B. parapertussis. In fact, we have 5 previously shown that convalescent serum collected from wild type 4 mice infected with a wild type strain of B. parapertussis at day 28 3 post-inoculation contained much higher titers of B. parapertussis2 specific antibodies than serum collected from mice infected with the 1 O-antigen mutant strain (54). A primary infection with the O-antigen 0 mutant did not protect well against a secondary challenge with wild Naïve Primary Bp Primary Primary type B. parapertussis. CFU were similar in mice previously infected Bpp Bpp-O-ag with B. pertussis (Log10 5.1) and those previously infected with the Oantigen mutant of B. parapertussis (Log10 4.6) (Fig. 7). A lack of O-antigen Fig. 7: C57BL/6 mice were inoculated in a primary infection correlated with an inability to efficiently control a with 5 x 105 CFU of B. pertussis (Bp), B. parapertussis (Bpp), or B. secondary challenge with B. parapertussis. Therefore, immune responses to parapertussis lacking O-antigen (BppO-antigen appear to be important to efficient protection against B. O-ag) and re-inoculated with Bpp 28 parapertussis infections. days later. Bacteria in the lungs were enumerated 3 days post-secondary infection. 3. Summary. Our preliminary studies suggest that B. parapertussis avoids B. pertussis-induced immune responses by an O-antigendependent mechanism. Further studies of the immune responses upon secondary infections by the bordetellae will allow us to elucidate how B. pertussis and B. parapertussis avoid reciprocal immunity. The role of pertussis toxin in reciprocal immunity between these pathogens will be analyzed. B. parapertussis strains in which pertussis toxin is inserted and B. pertussis strains from which pertussis toxin is deleted will be utilized to study the contribution of this toxin to the colonization of immune hosts. Preliminary studies also suggested that immune responses directed towards O-antigen are important to protective immunity against B. parapertussis. Since its sister subspecies does not express this antigen and vaccines do not include it, it is not unexpected that infection or vaccination by such a closely related organism does not confer efficient protection against B. parapertussis. Vaccinating only against B. pertussis is providing a selective immune-mediated pressure that could allow B. parapertussis to become the more prevalent etiologic agent of whooping cough. In fact, disease caused by this respiratory has been increasing in some populations (48). The inclusion of B. parapertussis in vaccination protocols has successfully curbed epidemics of this organism in the past (44). Thus, it may be recommended that O-antigen or a number of B. parapertussis antigens be added to the current acellular pertussis vaccines in order to induce immunity to both of the human-specific bordetellae. Aim 3 will provide an insight to the ability of B. parapertussis to emerge and thrive in a population in which a closely related species is already present (without displacing it). These findings may be of relevance to a number of bacterial and viral models of evolution. D. RESEARCH DESIGN AND METHODS BASIC METHODOLOGIES Inoculating and Enumerating Bacteria within the Respiratory Tract. Mice will be inoculated by our standard protocols with which we have extensive experience over the course of 10 years. Mice will be lightly sedated with 5% isoflurane in oxygen using a rebreather apparatus in a chemical safety 12 hood with carbon-filtered exhaust. Bacteria grown to mid-log phase in Stainer-Schulte broth will be washed and resuspended in PBS at the designated density and delivered intranasally by lightly touching a pipet tip to the external nares. Our high dose inoculation regimen uses 0.5-1 x 106 bacteria in 50 L of PBS, which we have observed to deliver bacteria throughout the respiratory tract at highly reproducible levels. The distribution of bacteria will be determined by sacrificing four animals at the time of inoculation and enumerating as below. The time course of infection and immune responses in the murine host then closely mimics patterns observed in human hosts (28,30-31). At various time points after inoculation (1, 2, 3, 5, 7, 10, 14, and/or 28) groups of four mice will be sacrificed, tissues will be excised and homogenized in PBS, and aliquots will be plated on to Bordet-Gengou agar with the appropriate concentrations of antibiotics to determine bacterial numbers. These protocols generate average and standard deviation values that allow differences between groups as small as 2 to 4 fold to be determined to be statistically significant by a Student's two-tailed t-test analysis (59). Immune Mice. To generate convalescent mice, mice will be intranasally inoculated with a high dose of B. parapertussis or B. pertussis as above at least 28 days prior to challenge. Secondary challenges will be made with antibiotic resistant strains in order to assure that only bacteria administered in the secondary inoculation are counted. To generate vaccinated mice, I.P. injections of 108 CFU of heat killed B. parapertussis or B. pertussis in 100L of PBS will be given 28 and 14 days prior to challenge. Bacteria are heat-killed by incubating at 70o F for 30 minutes. These groups of mice will then be inoculated with 5 x 105 CFU of either species via the intranasal route (as above). Pathology and Quantification of Cellular Infiltrate. For pathology, trachea and lungs will be inflated with 10% formalin in situ, excised and left in formalin overnight. Formalin-fixed tissues will be embedded in paraffin and sections cut for hematoxylin and eosin staining. Slides will be labeled with letters that do not correspond to treatment, and pathology scores are read by a trained mouse pathologist (M.J.K.) "blinded" as to the identity of any individual slide. To enumerate cellular infiltrate, lungs will be perfused with 2 mL of PBS, excised, and pressed through tissue sieves into 10 mL of media (DMEM, 10% fetal calf serum) (60). The media containing cells will be spun down on top of a sucrose gradient (Histopaque 1119-1, SigmaAldrich, St. Louis, MO, USA) for 30 minutes at 3000 rpm at room temperature to isolate the leukocyte layer. Total lung leukocytes are counted on a hemacytometer. Cell differentials (neutrophils, macrophages, and lymphocytes) are determined visually by counting 300 cells from randomly chosen high-powered-microscope fields of Wright-Giemsastained samples of lung leukocyte suspensions cytospun for 20 minutes at 300 rpm onto glass slides (Shandon Cytospin, Pittsburgh, PA). The absolute number of a leukocyte subset was calculated by multiplying the percentage of each subset in an individual sample by the total number of lung leukocytes in that tissue. We have recently validated this approach by parallel flow cytometric analysis, an approach that increases our ability to analyze subgroups of immune cells, and will continue to use this approach as well to determine numbers of leukocytes. ELISAs. Lung homogenates of the same animals used for enumeration of bacteria will be saved at -80oC for cytokine and chemokine ELISAs, and blood will be taken by cardiac puncture for the quantification of Bordetella-specific antibodies in the serum as previously described (61). Briefly, bacteria are gown to mid-log phase in Stainer-Schulte broth, heatkilled, washed and blocked with 1% BSA in a 96-well plate prior to the addition of the serum samples, serially diluted in PBS. A horseradish peroxide-linked secondary antibody that recognizes individual mouse antibody isotypes will be used to detect their respective concentrations within each sample. We have previously used this ELISA format to characterize the serum antibody response to each subspecies on day 28 (29,36) and have begun to examine individual isotypes including IgG1, IgG2a, IgG2b, IgG3, IgM, IgE, and IgA (36). We also recently began running antibody ELISAs for mucosal antibodies in homogenized lung tissues. Cytokine and chemokine ELISAs for F, IFNIL- 13 1IL-2, IL-4, IL-6, IL-10, JE, KC, TGFMIP-1and MIP-2will be performed according to the suppliers' protocols (R & D Systems, Minneapolis, MN, USA). Splenocyte restimulations. Mice will be inoculated with our high dose of B. parapertussis or B. pertussis via the intranasal route as above. At days 0, 3, 7, 14, or 28, mice will be sacrificed and spleens excised and homogenized through a tissue sieve in 3 mL of RPMI. This cell suspension will be spun down at 1500 RPM at 4o C for 5 minutes. The pellets will then be washed with 2 mL of 0.83% ammonium chloride solution for 2 minutes to lyse the red blood cells. After 2 minutes, 8 mL of RPMI will be added to the tubes in order to neutralize the ammonium chloride. Cell suspensions will be spun down again and washed twice with a rich medium (DMEM, 10% fetal calf serum, 1% BME). Splenic leukocytes will be resuspended at 107/mL in the rich medium and 200μL (2 x 106 cells) will be added to wells of a 96-well plate. The splenic leukocytes will then be stimulated with the stainer-sholte broth as a negative control or 107 CFU of heat-killed B. parapertussis or B. pertussis and incubated for 72 hours. Supernatants will then be collected for analysis by cytokine ELISAs performed according to the suppliers’ protocols (R & D Systems, Minneapolis, MN, USA). EXPERIMENTAL STRATEGY Specific Aim 1: Analyze the mechanisms of clearance of B. parapertussis from the respiratory tracts of immune hosts. Rationale: The prevalence of B. parapertussis in randomly tested individuals has been found to be fairly high in some populations (41). More importantly, some clinical studies have suggested that B. parapertussis is the causative agent of a large number cases of whooping cough (62). Our preliminary data shows that an infection or vaccination with this bacterium induces strong immune responses, resulting in the rapid clearance of subsequent B. parapertussis infections (Fig. 1). In this aim we propose to dissect the aspects of the host immune system that mediate the rapid clearance of B. parapertussis from an immune individual. In doing so, we hope to identify possible mechanisms by which this pathogen could evade these immune responses, perhaps leading to an understanding of how this pathogen is able to reinfect immune hosts and persist in the human population. A. Examine host factors necessary for efficient infection-induced immunity to B. parapertussis. To examine the ability of a primary B. parapertussis infection to induce immunity to a secondary infection with the same species, we will examine the time course of infection (via CFU quantification), inflammation (via leukocyte quantification and histological examination), cytokine and chemokines responses (via ELISAs), T cell responses (via splenocyte restimulations), and antibody responses (via ELISAs) in naive versus convalescent mice. Inoculation, as above, will be on day 28 post-primary infection, a time point at which the immune response to B. parapertussis is quite strong and the initial infection has diminished to negligible levels (29,36). The secondary infection will also be made with a gentamycin resistant B. parapertussis strain to avoid confusion with any bacteria left from the primary infection. We will start by inoculating wild type mice with groups of four mice being sacrificed 1, 3, 7, 10, and 14 days following secondary inoculation (days 29, 31, 35, 38, and 42). This will establish a time course of bacterial clearance from immune hosts and allow us to select one or two time points to examine when using immuno-deficient mice. The experiment shown in figure 1 was performed at a single time point with the recently sequenced strain of B. parapertussis (63) and we did not assess any other measures besides bacterial numbers. Our laboratory currently 14 maintains breeding colony of a variety of immuno-deficient mice and has a number of neutralizing antibodies specific for cell types, cytokines, and chemokines. Primary B. parapertussis infections will be given to TCRδ-/-, IgA-/-, CD11b-/, C3-/-, IFNγ-/-, Fcγ receptor-/-, TNFα-/-, TLR4-deficient, IL-10-/-, and IL-6-/- mice. Secondary infections with a gentamycin-resistant strain of B. parapertussis will be given 28 days later. Based on the time course of clearance from wild type mice, we will choose one or two appropriate time points to assess whether or not γδ Tcells, IgA, CD11b, C3, IFNγ, Fcγ receptors, TNFα, TLR4, IL-10, and IL-6 are required for efficient clearance of this bacterium from previously infected hosts. Additionally, C57BL/6 mice will be given a primary B. parapertussis infection and a secondary gentamycin-resistant B. parapertussis infection. However, one day prior to the secondary infection, they will be depleted of TNFα, IFNγ, TGF-β, IL-10, IL-12, or MCP-1 via i.p. injections of 1 mg of neutralizing antibodies (REFS). Other groups will be depleted of CD4+ T cells, CD8+ T cells, or neutrophil-like cells via i.p. injections of 1 mg of antibodies specific for CD4, CD8, and Ly-6G respectively (64-66). One group will be given 100 microliters of clodronate containing liposomes intranasally in order to make those mice deficient in alveolar macrophages (67). Lungs will be excised and homogenized for the quantification of CFU in the respiratory tract. The inflammatory response will be monitored by quantifying numbers and types of white blood cells, cytokines, and chemokines in the lungs. Sera will be collected from these animals an analyzed for titers of B. parapertussis-specific antibodies. Using the above strategies, we will be able to determine the contribution of γδ Tcells, IgA, CD11b, C3, IFNγ, Fcγ receptors, TNFα, TLR4, IL-10, IL-6, TGF-β, IL-12, MCP, CD4+ T cells, CD8+ T cells, neutrophils, and macrophages to the clearance of B. parapertussis from convalescent hosts and the generation of an immune response to this bacterium. This study should elucidate the mechanisms of bacterial clearance upon an infection of a convalescent individual by B. parapertussis. B. Examine host factors necessary for efficient vaccine-induced immunity to B. parapertussis. To examine the ability of a vaccination including heat-killed B. parapertussis to induce immunity to a challenge with the same species, we will examine the time course of infection and inflammation in naive versus vaccinated C57BL/6 mice. Vaccination will consist of two doses of 108 CFU of heat-killed bacteria (70o F for 30 minutes) in 0.1 mL of PBS injected i.p. at days 0 and 14. The challenge will be made by inoculating with the gentamycin resistant B. parapertussis strain 28 days after the initial vaccination. Groups of four mice will be sacrificed 1, 3, 7, 10, and 14 days following challenge with B. parapertussis (days 29, 31, 35, 38, and 42). Protection conferred by the vaccination will be compared to that observed in naive as well as convalescent animals. The experiment shown in figure 2 was performed at one time point and we did not assess any other measures besides bacterial numbers. As above, one or two time points will be selected to analyze the roles of specific immune factors in vaccine-induced immunity. γδ Tcell, IgA, CD11b, C3, IFNγ, Fcγ receptor, TNFα, TLR4, IL-10, and IL-6-deficient mice will be vaccinated and subsequently challenged with B. parapertussis in order to determine if these immune factors are required for protective vaccine induced immunity. We will also vaccinate μMT, TCRα-/-, and TCRαδ-/- mice and challenge with B. parapertussis since B and T cells are essential to elimination from naïve hosts but their roles in vaccine-induced immunity are unknown. Additionally, wild type mice will be vaccinated and, one day prior to challenge with B. parapertussis, will be depleted of TGF-β, IL-12, MCP, CD4+ T cells, CD8+ T cells, neutrophils, or macrophages to determine if these cytokines, chemokines, and cell types are essential to vaccine-induced immunity to B. parapertussis. Using our immuno-deficient mouse strains and neutralizing antibodies, the mechanisms of clearance upon an infection of vaccinated hosts by B. parapertussis will be uncovered. Combined with our knowledge of the immune responses that mediate bacterial clearance from convalescent hosts, we will then be able to hypothesize about the ability of B. parapertussis to re-infect immune hosts as we have successfully done with B. pertussis. Outcomes and potential problems: 15 We have performed all of the techniques described here and anticipate no problems. Watanabe and Nagai previously observed protection 14 days after the secondary infection with B. parapertussis (15), similar to the effects that we have observed upon an adoptive transfer of serum antibodies (36). However, our recent work has shown that the more complete immunity induced by infection allows for much more rapid clearance (within approximately 3 days, Figures 1 and 2) than in the adoptive transfer model. Primary B. parapertussis infection or vaccination resulted in the rapid elimination of secondary B. parapertussis infections. Determining the time course of infection in convalescent and vaccinated mice will allow us to determine the optimal time point to assess the protective effects of the various immune factors that will be tested. We have recently shown that clearance of B. bronchiseptica from immune hosts requires antibodies, TLR4, neutrophils, complement, Fcγ receptors, and complement receptor 3 (33). Upon comparing the immune responses necessary for elimination of B. bronchiseptica and B. parapertussis, we may find that these pathogens are cleared by similar mechanisms. T cells, neutrophils, and complement are required for the function of antibodies against B. parapertussis (36) suggesting that they would be necessary for efficient protection in convalescent or vaccinated mice. The role of T cells in the reduction of B. parapertussis numbers appears to be recruiting neutrophils to the site of infection. Therefore, if T cells, neutrophils, and complement are essential to bacterial elimination from previously infected or vaccinated hosts, we could conclude that this mechanism of clearance is similar to that observed upon an adoptive transfer of serum antibodies. The reduction of bacterial numbers would occur much faster in immunized mice as T cell responses would be generated much quicker in comparison to a naïve mouse. It is also possible that the mechanism of clearance of B. parapertussis from immunized mice would be quite different from that mediated by antibodies. The immune response generated by a previous infection or vaccination would theoretically protect against subsequent infections much more efficiently than antibodies alone. The immune factors necessary for antibody-mediated elimination (T cells, neutrophils, and complement) may be dispensable when mice are immunized with live or heat-killed B. parapertussis. For example, depleting neutrophils may not affect bacterial clearance from immunized mice as macrophages and dendritic cells could be sufficiently recruited and activated to control the infection. This knowledge will be applied in the following aims to hypothesize how B. parapertussis avoids B. pertussis-induced immunity. Specific Aim 2: Examine the levels of reciprocal immunity between B. parapertussis and B. pertussis. Rationale: Unfortunately, we must highlight the limitations of earlier work pertaining to reciprocal immunity between B. parapertussis and B. pertussis. One publication dealing with an experimental mouse model suggested that the two human-specific bordetellae induce fairly efficient cross-protection (15). However, they only analyzed protection at 14 days post-secondary inoculation and observed a reduction in bacterial numbers similar to what has been observed upon an adoptive transfer of Bordetella-specific antibodies (15,36). In addition, the previous study used the B. pertussis strain 18323, which was selected for its association with infections of mice and may be more closely related to B. bronchiseptica than B. pertussis (68). Specific aim 2 proposes to analyze the levels of reciprocal immunity between B. parapertussis and B. pertussis. Our initial work has shown that while a prior infection by B. parapertussis is protective against both species at day 3 post-inoculation, a prior infection by B. pertussis does not efficiently protect against B. parapertussis (Fig. 4). Interestingly, a vaccination with heat-killed B. parapertussis does not cause a significant decrease in the numbers of B. pertussis at day 3 post-inoculation (Fig. 5). Together, these data suggest that there are important differences in the immune response induced by infection versus vaccination. These closely related bacterial 16 species could either utilize mechanisms to avoid reciprocal immunity or induce weak immune responses to one another. Using the information obtained from specific aim 1 regarding the mechanism of clearance of B. parapertussis from immune individuals and our knowledge of the immune factors that are induced upon infections by B. pertussis, we should have an idea of what response could be defective upon a B. pertussis infection or vaccination, allowing colonization by B. parapertussis. The same should hold true for identifying how B. pertussis avoids B. parapertussis vaccine-induced immunity. A. Assess reciprocal infection-induced immunity between B. parapertussis and B. pertussis. We will examine the time course of infection and inflammation in naive mice or mice previously infected with the sister subspecies; for example, we will quantify B. parapertussis numbers and resulting inflammatory responses (leukocyte numbers and types, cytokines, and chemokines) in mice previously infected with B. pertussis. Inoculation of wild type mice, as above, will be on day 28 post-primary infection. The secondary infection will be made with a gentamycin resistant B. parapertussis strain or a nalidixic acid resistant B. pertussis strain to avoid confusion with bacteria from the primary infection. Groups of four mice will be sacrificed 1, 3, 7, 10, and 14 days following secondary inoculation (days 29, 31, 35, 38, and 42). Reciprocal protection conferred by the primary infection will be compared to that conferred by autologous immunity and to naive animals. Figure 4 shows that a primary B. parapertussis infection protects against subsequent infections by B. pertussis, but primary B. pertussis infection does not protect against B. parapertussis. We will also take groups of mice that are inoculated with B. parapertussis or B. pertussis and sacrifice them at day 28 without a secondary infection. Sera will be collected from these animals to look for B. parapertussis and B. pertussis-specific antibodies by ELISA. The spleens of these mice will also be excised and leukocytes from the spleen will be isolated. These splenocytes will then be restimulated with either heat-killed B. parapertussis or heat-killed B. pertussis to analyze the potential of T cells from B. parapertussis or B. pertussisinfected mice to be stimulated by the sister subspecies. From the time course generated from wild type mice, we will choose an appropriate time point to analyze the effects of specific immune factors on reciprocal protection. The knowledge of the specific host immune factors that are required for the clearance of B. parapertussis from the respiratory tracts of convalescent hosts (Aim 1) will allow us to speculate how this bacterium is evading B. pertussisinduced immunity. As above, previously infected γδ Tcell, IgA, CD11b, C3, IFNγ, Fcγ receptor, TNFα, TLR4, IL-10, IL-6, TGF-β, IL-12, MCP, CD4+ T cell, CD8+ T cell, neutrophil, or macrophage-deficient mice will be given a secondary inoculation of either subspecies to determine which immune factors are essential to cross-protection. B. Assess reciprocal vaccine-induced immunity between B. parapertussis and B. pertussis. An examination of the time course of infection and inflammation in naive mice or mice vaccinated with the sister subspecies will be performed; for example, we will quantify B. parapertussis numbers and resulting inflammatory responses (leukocyte numbers and types, cytokines, and chemokines) in mice previously vaccinated with heat-killed B. pertussis. Vaccination will consist of 2 doses of 108 heat-killed bacteria injected i.p. at days 0 and 14, and inoculation, as above, will be on day 28 post-initial vaccination. Groups of four mice will be sacrificed 1, 3, 7, 10, and 14 days post-inoculation (days 29, 31, 35, 38, and 42). This experiment will generate a time course of clearance that will allow us to examine one or two time points in subsequent experiments determining the roles of specific immune factors. Reciprocal protection conferred by vaccinations will be compared to protection conferred by autologous immunity and naive animals. Figure 5 shows that vaccinations are not cross-protective for either pathogen. Thus, two questions arise from this sub-aim; (i) what mechanisms are used by B. parapertussis and B. pertussis to avoid reciprocal immune responses and (ii) what is different about infection-induced versus vaccine-induced immunity to B. parapertussis. As above, B. parapertussis or B. pertussis vaccinated T cell, αβ T cell, γδ Tcell, IgA, CD11b, C3, IFNγ, Fcγ receptor, TNFα, TLR4, IL-10, IL-6, B cell, TGF-β, IL-12, MCP, CD4+ T cell, CD8+ T cell, neutrophil, or 17 macrophage-deficient mice will be challenged with either subspecies to determine the immune factors that mediate the reduction of bacterial numbers. Through these analyses, the specific aspects of host immunity that allow for efficient colonization of vaccinated hosts by the sister subspecies will be discovered. Aim 3 will focus on strategies used by the bacteria to avoid these immune responses. Outcomes and potential problems: We have performed all of the techniques described here and anticipate no problems. Although previous experimental studies have suggested that the human-specific bordetellae induce efficient cross-protection, figure 4 shows the asymmetrical cross-protection that has prompted further studies by our group. Watanabe and Nagai previously observed protection 14 days (which is similar to the time it takes for antibodies alone to have an effect) after B. parapertussis infection in mice previously infected with the B. pertussis strain 18323 (15). These results may not reflect the natural interactions between these two organisms. 18323 was selected based on its infection in mice and has been shown to resemble B. bronchiseptica, rather than B. pertussis, in a number of important regards including LPS structures and expression of the type III secretion system (68). Whether our day 14 results show efficient cross-protection, our day 3 results indicate that B. pertussis-induced immunity does not efficiently limit colonization by B. parapertussis. We may observe that B. parapertussis is able to persist for 14 days or more in B. pertussis-immune hosts which would support the theory that B. parapertussis utilizes some mechanism to avoid B. pertussis-induced immunity. Importantly, B. parapertussis infections that can last up to two weeks would likely be sufficiently long to allow this bacterium to spread to other human contacts, allowing it to persist in dense, B. pertussis-immune populations. An alternative possibility is that B. parapertussis will be cleared between 3 and 14 days. Even if this is true, B. parapertussis would still be more fit relative to B. pertussis in a population in which B. pertussis was endemic, allowing the former to emerge as a human pathogen. While our preliminary data shows that B. pertussis infection or vaccination does not confer efficient protection against B. parapertussis, it is not currently known why this is true. Previous work dealing with reciprocal immunity studies suggested that antibodies specific for B. parapertussis and B. pertussis are not cross-reactive (15). If we find antibodies are not cross-reactive and no reduction of B. parapertussis numbers is observed in B. pertussis-immunized B cell-deficient mice, we will conclude that the lack of cross-protection is due to a lack of cross-reacting antibodies. While antibodies are essential to the clearance of B. parapertussis from the respiratory tract (36), T cells and IFNγ are required for the function of these antibodies (36, Fig. 2) and may mediate the rapid clearance observed from convalescent or vaccinated mice (Fig. 1). Therefore, a defect in B. parapertussis-specific T cell responses upon immunization with B. pertussis may result in delayed clearance of B. parapertussis. B. parapertussis infection or vaccine may be ineffective against subsequent B. parapertussis infections upon the depletion of a specific T cell population (αβ, γδ, CD4+, or CD8 + T cells) and IFNγ. Additionally, stimulation of splenocytes from B. pertussisinfected mice with B. parapertussis may not induce high levels of cytokine production. If the previous two statements prove to be correct, we can conclude that inefficient reciprocal protection is due to a lack of cross-reacting T cell responses. The same approaches can be used to determine if B. parapertussis vaccination (relative to infection) does not induce B or T cell responses to B. pertussis. Specific Aim 3: Uncover the mechanisms by which the human-specific bordetellae avoid immunity induced by each other. Rationale. 18 It would be expected that the immune responses induced by B. parapertussis and B. pertussis would be crossreactive due to the similarities between the two subspecies. However, primary B. pertussis infections do not significantly protect against secondary B. parapertussis infections (Fig. 3) and vaccinations with either of the human pathogens are not cross-protective (Fig. 4). In our third aim, we plan to address the strategies used by these closely related, host-specific pathogens to avoid immune responses induced by one another, allowing their co-existence in the human population. B. parapertussis and B. pertussis share the majority of their virulence factors, but there are a few striking differences between the two. B. parapertussis expresses O-antigen, which is important for the colonization of hosts by this bacterium (54). Studies of this virulence factor were performed in the context of a naïve host and did not address the contribution of O-antigen to the colonization of immune hosts. B. pertussis produces pertussis toxin, a virulence factor that is specific to this pathogen. Pertussis toxin is required for the colonization of naïve hosts as well as hosts given an adoptive transfer of serum antibodies (35,37,69). It is thought that the expression of this toxin by B. pertussis allows this organism to re-infect immune hosts, therefore it may be crucial to evading B. parapertussis vaccine-induced immunity. Using bacterial mutants deleted of these genes (and a B. parapertussis strain with pertussis toxin inserted) will allow us to analyze the roles of O-antigen and pertussis toxin in the evasion of reciprocal immune responses. From these data, we will develop a better understanding of the evolution of the human-adapted bordetellae. A. Determine the role of O-antigen in evading B. pertussis-induced immunity. We will address the role of O-antigen in the evasion of both B. pertussis infection- and vaccine-induced immunity by B. parapertussis. Using the inoculation and vaccination strategies above, mice immune to B. parapertussis or B. pertussis will be challenged with the previously described B. parapertussis strain lacking O-antigen (70). Mice will be sacrificed at days 1, 3, 7, 10, and 14 post-challenge (days 29, 31, 35, 38, and 42). The ability of the O-antigen mutant to colonize the respiratory tract and the accompanying inflammatory responses will be examined as above. The key comparison for this experiment will be between B. pertussis-immune mice infected with wild type B. parapertussis versus the O-antigen mutant of B. parapertussis. Figure 6 shows that unlike the wild type strain, the Oantigen mutant of B. parapertussis is rapidly cleared from B. pertussis-immune individuals. This experiment was only done at one time point and only bacterial numbers were measured, but it suggests that O-antigen mediates the evasion of B. pertussis-induced immunity by B. parapertussis. The information obtained from aims 1 and 2 regarding the delayed clearance of B. parapertussis from B. pertussis-immune hosts will allow us to hypothesize what B. pertussisspecific immune response, if any, O-antigen could inhibit. An ELISA for antibodies specific for B. parapertussis versus the O-antigen mutant of B. parapertussis will be performed using serum raised against B. pertussis infections and vaccinations as O-antigen may inhibit the binding of these antibodies to cross-reacting antigens. Splenocytes from B. pertussis-infected mice will be restimulated with wild type versus the O-antigen mutant of B. parapertussis to determine if T cells from B. pertussis-infected mice respond more efficiently to the O-antigen mutant. In any case, it appears that O-antigen has some role in the evasion of B. pertussis-induced immunity by B. parapertussis and our experimental model will shed light on how this is accomplished. B. Study the protective role of immune responses to O-antigen. Our preliminary data shows that like a primary B. pertussis infection, a primary infection with the O-antigen mutant of B. parapertussis does not prevent efficient colonization of the respiratory tract by wild type B. parapertussis (Fig. 7). Since B. pertussis also does not express O-antigen, we have hypothesized that an immune response to Oantigen is crucial to B. parapertussis immunity and immunizing with this antigen would protect against a challenge with B. parapertussis. This is consistent with the fact that a primary infection with B. bronchiseptica, which does express O-antigen, confers reciprocal immunity to B. parapertussis. We have obtained purified LPS (which contains O-antigen) (ANDY) and will vaccinate with 100 nanograms it at days 0 and 14. At day 28 post-initial vaccination, 19 mice will be challenged with the wild type strain of B. parapertussis. These mice will then be sacrificed at days 1, 3, 7, 10, and 14 post-inoculation (days 29, 31, 35, 38, and 42). Bacterial colonization and inflammatory responses will be quantified and compared to those observed in mice that received a primary B. parapertussis infection or vaccination with heat-killed B. parapertussis as well as those observed in naïve mice. We will also look more in depth at the ability of a primary infection or vaccination with the O-antigen mutant of B. parapertussis to confer immunity to the wild type strain by assessing bacterial numbers and inflammatory responses at days 1, 3, 7, 10, and 14 post-secondary infection/challenge (days 29, 31, 35, 38, and 42). These experiments will determine the roles of LPS and O-antigen as protective antigens upon infections by B. parapertussis. C. Determine the effect of pertussis toxin in the evasion of reciprocal immunity. We have proposed that B. parapertussis lost the expression of pertussis toxin, which is crucial to efficient colonization by B. pertussis, in order to have fewer cross-reacting protective antigens with its sister subspecies. Using a strain of B. parapertussis in which pertussis toxin has been inserted (which we are in the process of creating), we will assess the effect of this toxin on the ability of this bacterium to infect B. pertussis-immune hosts. We will infect mice previously infected with or vaccinated against B. pertussis with this strain and sacrifice groups at days 1, 3, 7, 10, and 14 post-secondary inoculation (days 29, 31, 35, 38, and 42) in order to see if the addition of pertussis toxin affects the ability of B. parapertussis to infect B. pertussis-immune hosts. We also plan to use a pertussis toxin-deficient strain of B. pertussis (71) to test the role of this toxin in the evasion of B. parapertussis-vaccine induced immunity by B. pertussis. Mice previously infected or vaccinated with B. parapertussis will receive a secondary infection/challenge with the pertussis toxin-deficient B. pertussis strain. Groups will then be sacrificed at days 1, 3, 7, 10, and 14 postsecondary inoculation (days 29, 31, 35, 38, and 42). Since B. pertussis can infect vaccinated but not convalescent hosts, there must be some immune response that is induced more efficiently upon infection by B. parapertussis but is not induced as well upon vaccination with B. parapertussis. Data from specific aim 1 and 2 will address the differences in vaccination versus infection. Pertussis toxin has previously been shown to aid the colonization of naive hosts and those given an adoptive transfer of B. pertussis-specific antibodies (35,37,69). Current theories suggest that this toxin is vital to the ability of this bacterium to re-infect immune hosts. This virulence factor may also have a key role in colonizing hosts that have been vaccinated with B. parapertussis. Outcomes and potential problems: We have performed all of the techniques described here and anticipate no problems. We will soon be receiving a new transfection vector that should facilitate the insertion of a functional pertussis toxin gene into B. parapertussis (72). Our preliminary data shows that O-antigen expression is an important factor, if not the most important factor, in the ability of B. parapertussis to infect B. pertussis-immune hosts. O-antigen also appears to be a crucial protective antigen in B. parapertussis infections. The role of pertussis toxin in both the ability of B. parapertussis to avoid B. pertussis-induced immunity and the ability of B. pertussis to avoid B. parapertussis-induced immunity will be examined. This will be done using the insertion of pertussis toxin into B. parapertussis and a strain of B. pertussis from which pertussis toxin has been deleted. Our preliminary data suggests that O-antigen enables B. parapertussis to avoid B. pertussis-induced immunity. If it is found that B. parapertussis lacking O-antigen is unable to colonize B. pertussis-infected or vaccinated mice, we will conclude that O-antigen protects B. parapertussis from B. pertussis-induced immunity. We may observe that the O-antigen mutant is able to colonize previously vaccinated, but not convalescent mice. This is a distinct possibility as our data indicates that there are differences between infection- and vaccine-induced immunity to the bordetellae. This 20 outcome will lead us to hypothesize that O-antigen is required for the evasion of B. pertussis infection- but not vaccineinduced immunity. For the most part, the immune responses to the LPS structures of B. parapertussis, B. pertussis, and B. bronchiseptica are cross-reactive (73). One exception is that B. parapertussis LPS is not efficiently recognized by an immune response to B. pertussis LPS (73), correlating with the apparent lack of protection conferred by B. pertussis infection or vaccination (Figures 4 and 5). O-antigen may be the key protective antigen to B. parapertussis infections. If that is true, a primary infection or vaccination with the O-antigen mutant of B. parapertussis will not protect against the wild type strain. Additionally, vaccinating with purified B. parapertussis LPS will efficiently protect against subsequent infections. Alternatively, the O-antigen may confer partial protection and an LPS vaccination may not confer complete protection. There may not be one key virulence factor to avoiding reciprocal immune responses or to providing protection. Antigenic variations in several of these virulence factors could lead to inefficient recognition of the B. parapertussis by the sister subspecies, B. pertussis. By analyzing the immune responses and whether or not they are cross-reactive (via splenocyte restimulations, Bordetella-specific antibody ELISAs, etc.), we will be able to determine if this is indeed the case. The hypothesis that B. parapertussis not expressing pertussis toxin limits cross-reactivity between it and B. pertussis will be tested using the bacterial mutants mentioned above. It is possible that a B. parapertussis strain expressing pertussis toxin will colonize B. pertussis-immune hosts less efficiently compared to wild type B. parapertussis due to the additional shared antigen. If this is true, we will conclude that the lack of pertussis toxin expression increases the ability of B. parapertussis to infect B. pertussis-immune hosts. Given that pertussis toxin is essential to efficient colonization by B. pertussis in vivo (35,37,69), we may also observe that B. parapertussis expressing pertussis toxin colonizes more efficiently compared to wild type B. parapertussis. This would suggest that B. parapertussis lost the ability to express a functional pertussis toxin independent of selective pressure provided by B. pertussis-specific immunity in the human population. Since pertussis toxin enhances colonization by B. pertussis, the ability of this bacterium to avoid B. parapertussis vaccine-induced immunity may be dependent on this toxin. This will be tested by vaccinating with heatkilled B. parapertussis and subsequently infecting with the pertussis toxin mutant of B. pertussis described above. This mutant may be rapidly cleared from B. parapertussis vaccinated mice suggesting that the expression of pertussis toxin allows B. pertussis to infect B. parapertussis vaccinated hosts. Alternatively, this lack of reciprocal protection may be independent of pertussis toxin. We will conclude that this virulence factor does not aid the evasion of cross-protection if the pertussis toxin mutant is still able to efficiently colonize B. parapertussis vaccinated mice. E. HUMAN SUBJECTS (not applicable) F. VERTEBRATE ANIMALS Description and justification for the use of mice. Mice were chosen for this research because of the availability of "knockout" strains deficient in specific cellular or molecular components of the immune system. Mouse infection models have been established with the bordetellae and used extensively in the analysis of various parameters of infection, reproducing those observed in human disease in most regards. Colonization is very efficient, and all three classical bordetellae increase in numbers rapidly over the first few days postinoculation. Upon inoculation with B. parapertussis or B. pertussis, the inflammatory infiltrate, leukocytosis, gradual generation of antibody and T cell responses and delayed bacterial clearance all mimic aspects of human disease. It is impossible to predict the precise time points at which effects may be observed, so we have chosen 21 multiple points in the infection process that our experience has shown can give a reasonable overview of the time course. For example, in a typical study to determine the time course of infection, bacterial numbers will be determined on day 0 post-inoculation (to assure consistent inoculation), day 3 (logarithmic growth), day 7 (peak of bacterial numbers in wild type mice), day 14 (when bacterial numbers are markedly decreased and antibodies are detectible), and day 28 (when bacteria are >99.9% eliminated). Therefore, a typical experiment will consist of 20 mice (4 mice per time point x 5 time points) in each group. The effects we are studying will be large, for example, there are millions of bacteria in the lower respiratory tract from days 3 to 14 in a naive animal but infections may be completely cleared from convalescent or vaccinated animals. Therefore, there is a very broad range of sensitivity within which the contribution of virulence factors or immune functions can be measured. We have previously shown that the variation within groups of mice infected with either B. parapertussis or B. pertussis is small enough that five-fold differences can consistently be determined to be statistically significant (Student's two-tailed t-test) with groups of 4 mice. We will attempt to perform experiments in parallel so that the same set of controls can be used for multiple experiments. An analysis of whether there is any statistically significant difference between control groups treated identically will provide additional information about the reproducibility of these assays and therefore the need for repeating these controls, with equal number of animals and time points, in subsequent experiments. Careful and parsimonious use of mice is an important concern that maintains our attention. However, all experiments to be published, which should include the majority of those described here, will need to be repeated, at least for the critical time points. Our detailed budget therefore incorporates the cost of reproducing these experiments. Procedures limiting discomfort, distress, pain, and injury. The PI and key personnel have extensive research experience with the use of mice in various experimental procedures including that involving the use of immuno-deficient mouse strains to investigate the role of the pulmonary immune system during bacterial infection. Therefore, we know how to handle the mice and administer the appropriate analgesics to alleviate and minimize any discomfort or distress that may occur. Mice will be lightly sedated with isoflurane (30-45 s) before intraperitoneal injection of sera and/or intranasal challenge with bacteria. They will be monitored closely when under anesthesia and during recovery. Intranasal inoculation with Bordetella will be performed by the following method used in past research done by the PI (74). Each mouse will be lightly sedated with 5% isoflurane in oxygen using a rebreather apparatus in a chemical safety hood with carbon-filtered exhaust before PBS containing bacteria is delivered to the external nares without touching the pipettor tip to the animal. In experiments involving intraperitoneal injections, each mouse will be lightly sedated as just described before being given the 0.1 mL injection in the lower abdomen. Euthanasia. Mice will be euthanized with asphyxiation by CO2 before post mortem dissection of the respiratory tract. This method is accepted by the Institutional Animal Care and Use Committee for The Pennsylvania State University and by the American Veterinary Medical Association. FACILITIES AND RESOURCES We would briefly like to elaborate on our expertise as it applies to these studies. During graduate work in the laboratory of Dr. Sherie Morrison, PI Eric Harvill performed molecular immunology studies focused on the structure and function of antibodies and cytokines. These studies involved extensive use of all of the antibody production, purification, and assays described below, as well as extensive work in mouse models including vaccination and adoptive transfer. During postdoctoral studies in the laboratory of Dr. Jeff F. Miller, Dr. Harvill studied the three classical Bordetella subspecies in the mouse model. Dr. Harvill has extensive experience in the molecular 22 manipulation of these bacteria and the analysis of all of the measures of infection and pathology described below, including inoculation, vaccination, and adoptive transfer of immunity in normal and immunocompromised mice. Breeding and Infection Rooms. Our laboratory occupies three rooms in the basement of the Henning Building at the University Park campus of The Pennsylvania State University that are used solely for the breeding of our mouse colonies. We have an additional room here that is dedicated to the infections, euthanizations, and dissections of animals. The breeding of our mice is directly monitored by appropriately trained graduate students and laboratory technicians. The infection/euthanization/dissection room contains the rebreather apparatus for the infection of mice, CO2 tanks and chamber for euthanization, and a hepa-filtered hood in which dissections of mice take place. Mice and antibodies. We have obtained a variety of wild type and immuno-deficient mouse strains; C57BL/6, C3H/HEN, C3H/HEJ (TLR4 deficient), RAG2-/- ,μMT (B cell deficient), TCRα-/- (alpha/beta T cell deficient), TCRαδ-/- (alpha/beta and gamma/delta T cell deficient), TCRδ-/- (delta/gamma T cell deficient), Interferon-γ-/-, TNF-α-/-, FcR-/-, and CD11b-/- mice (Jackson Laboratories, Charles River Laboratories, Taconic Laboratories). C3-/- mice were obtained from Dr. Rick Wetsel (REF) and IgA-/- mice were obtained from Dr. Innocent Mbawuike (REF). We also have access to the university’s hybridoma facility at which supernatants from our various hybridomas are prepared. The production of these hybridomas include antibodies that neutralize TNF-α, Interferon-γ, TGF-β, MCP-1, Interleukin-4, Interleukin-12, GM-CSF, CD8, CD4, and LFA-1 (ATCC, Manassas, VA, USA). These immuno-deficient mouse strains and neutralizing antibodies will be used to determine what immune factors are required for bacterial clearance. Veterinary Care. Mice will be housed in the animal facility located in the basement of Henning building. Routine animal care is provided by the Animal Resource Program (ARP) which maintains the facility. Mice will be fed a standard diet and food or fluid will not be restricted. A separate room will be used for infecting and housing infectious mice. In addition, microisolator lids will be used to prevent inappropriate contamination. The ARP is based in the Office of the Vice President for Research. It has primary responsibility for the health, care, and use of laboratory animals at the University Park Campus of The Pennsylvania State University. To fulfill this responsibility, ARP provides a variety of services including management of all laboratory space, central animal purchasing, daily animal care, and veterinary medical and research support. The program and care meet the requirements of the Guide For the Care and Use of Laboratory Animals and all other State and Federal regulations. Penn State's animal care and use program is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC). The ARP has three laboratory animal medicine veterinarians on its staff, one that is a diplomate of the American College of Laboratory Animal Medicine (ACLAM). The Animal Care Coordinator has an M.S. degree and is certified by the American Association for Laboratory Animal Science (AALAS) as an animal technologist. The animal technicians and the veterinary technician are a very stable work force, and most have been employed in animal care throughout their working lives. All are certified at various levels by AALAS. BIBLIOGRAPHY 1. Cherry, J. D. 1999. Epidemiological, clinical, and laboratory aspects of pertussis in adults. Clin Infect Dis Suppl 2:S112-117. 2. Musser JM, Hewlett EL, Peppler MS, Selander RK. 1986. Genetic diversity and relationships in populations of Bordetella spp. J Bacteriol 166:230-237. 23 3. Mattoo, S. and Cherry, J.D. 2005. Molecular pathogenesis, epidemiology, and clinical manifestations of respiratory infections due to Bordetella pertussis and other Bordetella subspecies. Clin Microbiol Rev 18:326-382. 4. Olson, L. C. 1975. Pertussis. Medicine (Baltimore) 54:427-469. 5. Bpp is milder and shorter 6. Watanabe, M. and Nagai, M. 2004. Whooping cough due to Bordetella parapertussis: an unresolved problem. Expert Rev Anti Infect Ther 2:447-454. 7. Crowcroft NS, Stein C, Duclos P, Birmingham M. 2003. How best to estimate the global burden of pertussis? Lancet Infect Dis 3:413-418. 8. Rohani, P., C.J. Green, N.B. Mantilla-Beniers, and B.T. Grenfell. 2003. Ecological interference between fatal diseases. Nature 422:885-888. 9. von Konig, C. H., S. Halperin, M. Riffelmann, and N. Guiso. 2002. Pertussis of adults and infants. Lancet Infect Dis 2:744-750. 10. Skowronski, D. M., G. De Serres, D. MacDonald, W. Wu, C. Shaw, J. Macnabb, S. Champagne, D.M. Patrick, and S.A. Halperin. 2002. The changing age and seasonal profile of pertussis in Canada. J Infect Dis 185:1448-1453. 11. Bb infects mammals 12. Bb infects immunocompromised humans 13. Parkhill 14. Yuk MH, Heininger U, Martinez de Tejada G, Miller JF. 1998. Human but not ovine isolates of Bordetella parapertussis are highly clonal as determined by PCR-based RAPD fingerprinting. Infection 26:270-273. 15. Watanabe, M. and Nagai, M. 2001. Reciprocal protective immunity against Bordetella pertussis and Bordetella parapertussis in a murine model of respiratory infection. Infect Immun 69:6981-6986. 16. Liese JG, Renner C, Stojanov S, Belohradsky BH; Munich Vaccine Study Group. 2003. Clinical and epidemiological picture of B pertussis and B parapertussis infections after introduction of acellular pertussis vaccines. Arch Dis Child 88:684-687. 17. Willems RJ, Kamerbeek J, Geuijen CA, Top J, Gielen H, Gaastra W, Mooi FR. 1998. The efficacy of a whole cell pertussis vaccine and fimbriae against Bordetella pertussis and Bordetella parapertussis infections in a respiratory mouse model. Vaccine 16:410-416. 18. Heininger U, Stehr K, Christenson P, Cherry JD. 1999. Evidence of efficacy of the Lederle/Takeda acellular pertussis component diphtheria and tetanus toxoids and pertussis vaccine but not the Lederle whole-cell component diphtheria and tetanus toxoids and pertussis vaccine against Bordetella parapertussis infection. Clin Infect Dis 28:602-604. 19. David, S., van Furth, R., and Mooi, F.R. 2004. Efficacies of whole cell and acellular pertussis vaccines against Bordetella parapertussis in a mouse model. Vaccine 22:1892-1898. 20. Model mouse infection 21. “” 22. “” 23. “” 24 24. “” 25. Ref for ID50 of Bpp and Bb 26. Ref for ID50 of Bp 27. Ref for even distribution of inocula throughout resp tract 28. colonization and clearance similar in mice and humans 29. Kirimanjeswara, G. S., P.B. Mann, and E.T. Harvill. 2003. Role of antibodies in immunity to Bordetella infections. Infect Immun 71:1719-1724. 30. Delayed clearance in humans 31. Immune response similar in humans and mice 32. Humoral and cellular immunity leads to clearance from humans 33. Kirimanjeswara, 2005 JI 34. Mann, P.B., Wolfe, D.N., Latz, E., Golenbock, D., Preston, A., and Harvill, E.T. 2005. Comparative Toll-Like Receptor 4-Mediated Innate Immune Responses to the Bordetellae. Infect Immun In press. 35. Kirimanjeswara, G. S., L.M. Agosto, M.J. Kennett, O.N. Bjornstad, and E.T. Harvill. 2005. Pertussis toxin inhibits neutrophil recruitment to delay antibody-mediated clearance of Bordetella pertussis. 2005 in press 36. Wolfe, D.N., Kirimanjeswara, G.S., and Harvill, E.T. 2005. Clearance of Bordetella parapertussis from the lower respiratory tract requires cellular and humoral immunity. Infect Immun 73:6508-6513. 37. Carbonetti 2005 38. Bpp does not express ptx 39. Bp immunity wanes 40. Bpp reinfects 41. Bpp can be high in randomly sampled populations 42. only ~ 1:600 cases of Bp reported 43. new Bp strains since vaccine 44. Burianova-Vysoka 45. Epidemiological theory suggests more virulent pathogen should displace less virulent 46. Stehr K, Cherry JD, Heininger U, Schmitt-Grohe S, uberall M, Laussucq S, Eckhardt T, Meyer M, Engelhardt R, Christenson P. 1998. A comparative efficacy trial in Germany in infants who received either the Lederle/Takeda acellular pertussis component DTP (DTaP) vaccine, the Lederle whole-cell component DTP vaccine, or DT vaccine. Pediatrics 101:1-11. 47. antigenic variation between Bp and Bpp 48. Lautrop, H. 1971. Epidemics of parapertussis. 20 years' observations in Denmark. Lancet 1: 1195-1198. 49. Ptx inhibition of G-proteins 25 50. Harvill, E. T., P.A. Cotter, and J.F. Miller. 1999. Pregenomic comparative analysis between bordetella bronchiseptica RB50 and Bordetella pertussis tohama I in murine models of respiratory tract infection. Infect Immun 67:6109-6918. 51. Mills IFNg paper 52. everyone has been infected with Bp or Bpp 53. reinfection of immune hosts 54. Burns, V., Pishko, E.J., Preston, A., Maskell, D.J., and Harvill, E.T. 2003. Role of Bordetella O antigen in respiratory tract infection. Infect Immun 71:86-94. 55. Cortes 2002 56. Merino 1992 57. Schiller 1989 58. Skurnik 1999 59. Ref for 2-4 fold difference being significant 60. Ref for cell counting 61. Allen, A. G., Thomas, R.M., Cadisch, J.T., and Maskill, D.J. 1998. Molecular and functional analysis of the lipopolysaccharide biosynthesis locus wlb from Bordetella pertussis, Bordetella parapertussis and Bordetella bronchiseptica. Mol Microbiol 29:27-38. 62. Borska, K. and Simkovicova, M. 1972. Studies on the circulation of Bordetella pertussis and Bordetella parapertussis in populations of children. J Hyg Epidemiol Microbiol Immunol 16:159-172. 63. Heininger 2002 64. Ref for using anti-CD4 65. Ref for anti-CD8 66. Ref for anti-Ly-6G 67. Ref for clodronate 68. Ref for 18323 69. Carbonetti NH, Artamonova GV, Mays RM, Worthington ZE. 2003. Pertussis toxin plays an early role in respiratory tract colonization by Bordetella pertussis. Infect Immun 71:6358-6366. 70. Preston A, Allen AG, Cadisch J, Thomas R, Stevens K, Churcher CM, Badcock KL, Parkhill J, Barrell B, Maskell DJ. 1999. Genetic basis for lipopolysaccharide O-antigen biosynthesis in bordetellae. Infect Immun 67:3763-3767. 71. Ref for delta ptx 72. Ref for transfection vector 73. Watanabe 1989 74. Eric using methods 26