* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Facial Nerve Palsy
Survey
Document related concepts
Transcript
Facial Nerve Palsy
Lip Teh 2005
Anatomy
Segment
Location
Length,
mm
Supranuclear
Cerebral cortex, precentral gyrus
NA
Brain stem(Pons)
Motor nucleus of facial nerve, superior salivary nucleus of tractus
solitarius
NA
Meatal segment
Brain stem to internal auditory meatus
13-15
Labyrinthine segment
Fundus of IAC to geniculate ganglion
3-4
Tympanic segment
Geniculate ganglion to pyramidal eminence
8-11
Mastoid segment
Pyramidal process to stylomastoid foramen
10-14
Extratemporal segment Stylomastoid foramen to pes anserinus
15-20
1) Cortical
a. voluntary motor –
i. lower segment of the precentral gyrus
ii. cross in the caudal pontine region to reach the facial motor nucleus in
the contralateral pons.
iii. Fibres to upper facial muscles also ramify to ipsilateral nucleus
2) Pons
a. Facial motor nucleus dorsolateral portion of the pons
b. exits the brainstem near the pontomedullary junction.
3) Intratemporal
a. 3 parts
i. Labyrinthine (5mm) - entrance of the fallopian canal to the geniculate
ganglion. Narrowest portion here.
ii. tympanic or horizontal segment (10 mm) - to the prominence of the lateral
semicircular canal
iii. mastoid or vertical segment (10mm) – to the stylomastoid foramen
b. Branches
i. greater petrosal nerve – leaves the geniculate ganglion. First branch
from labyrinthine part
ii. nerve to the stapedius muscle – arises from vertical segment
iii. auricular branch (sensory) – supplies posterior external auditory canal
and inferior conchal bowl
iv. chorda tympani nerve – between vertical segment and extratemporal
portion
c. Geniculate ganglion – 2mm long, cell bodies for taste anterior 2/3rd tongue
d. facial nerve occupies about 25% to 50% of the lumen of the bony canal. Less in
children
e. Narrowest in the Labyrinthine segment
4) Extratemporal
a. Innervates 23 paired muscle (18 paired facial expression muscle) and single
orbicularis oris
b. Facial nerve trunk landmark
i. tragal pointer – nerve is 1-1.5cm deep and inferior
ii. attachment of digastric – nerve 1cm inferior
iii. tympanomastoid suture – nerve 6-8mm beyond the drop-off point
c. Branches
i. As exits foramen
1. posterior auricular nerve (auricular muscles, occipitalis)
2. branch to posterior belly digastric and stylohyoid
ii. Main trunk divides into
1. temporozygomatic
a. temporal/frontal
i. Pitanguy’s line – 0.5cm below the tragus to
1.5cm lateral to eyebrow.
ii. 2-5 rami
iii. lie within the same plane at the deep surface
of the temporoparietal fascia
b. zygomatic
c. buccal
i. runs with the parotid duct either superiorly or
inferiorly
2. cervicofacial
a. marginal mandibular
i. posterior to facial artery, lies above the
inferior border of the mandible (80%) or
within 1-2 cm below (20%)
ii. anterior to facial artery, 100% pass above the
inferior border
iii. deep to the platysma, becomes superficial 2
cm lateral to oral commissure and ends on the
undersurface of the muscles.
iv. 2-4 branches - 2 branches (60%), 3 branches
(20%), 4 branches (20%)
b. Cervical
i. usually accompanies the posterior facial vein
as it emerges from the tail of the parotid
gland.
d. The zygomatic, buccal, and marginal mandibular branches lie in intimate
relationship with the retaining ligaments of the face (zygomatic ligament, the
masseteric cutaneous ligament, and the mandibular ligament)
e. Interconnections between the zygomatic and buccal branches are noted in over
70% of cases
f. Interconnections between the temporal or marginal mandibular branches to
other facial nerve branches occur in less than 15% of cases.
Muscles described in 4 layers(superficial to deep)
Nerve supply is superficial on 4th layer
1) Depressor anguli oris, superficial head zygomaticus minor, orbicularis oculi
2) Platysma, risorius, zygomaticus major, deep head zygomaticus minor, levator labii
superioris alaeque nasi
3) Levator labii superioris, orbicularis oris
4) Levator anguli oris, mentalis, buccinator
Modioulus
1) Risorius
2) Orbicularis Oris
3) Buccinator
4) Zygomaticus major
5) Levator anguli oris
6) Depressor anguli oris
Branch
Location of Lesion
Actions
Posterior
auricular
Posterior auricular
Pulls ear backward
Occipitofrontalis, occipital belly
Moves scalp backward
Stylohyoid
Retract/elevate hyoid
Posterior belly digastric
Depress/retract chin
Anterior auricular
Pulls ear forward
Superior auricular
Raises ear
Main trunk
Frontal
Occipitofrontalis, frontal belly
Moves scalp forward
Orbicularis oculi
Superior ½ - frontal
Inferior ½ - zygomatic
Closes eyelids
Corrugator supercilii
transverse head – frontal
Oblique head - zygomatic
Pulls eyebrow medially and downward – vertical frown
Procerus
Superior part – frontal
Inferior part - zygomatic
Pulls medial eyebrow downward
Zygomaticus major
Elevates corners of mouth
Zygomaticus minor
Elevates upper lip
Levator labii superioris
Elevates upper lip and midportion nasolabial fold
Levator labii superioris alaeque nasi
Elevates medial nasolabial fold and nasal ala
Risorius
Aids smile with lateral pull
Buccinator
Pulls corner of mouth backward and compresses cheek
Levator anguli oris
Pulls angles of mouth upward and toward midline
Orbicularis
Closes and compresses lips
Nasalis, dilator naris
Flares nostrils
Nasalis, compressor naris
Compresses nostrils
Depressor anguli oris
Pulls corner of mouth downward
Depressor labii inferioris
Pulls lower lip downward
Marginal
mandibular
Mentalis
Pulls skin of chin upward, everts lips
Cervical
Platysma
Pulls down corners of mouth
Frontal and
zygomatic
Zygomatic and
buccal
Buccal
Buccal and
marginal
mandibular
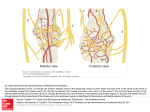
Blood Supply
1) Rolandic branch of the middle cerebral artery - cortical motor area of the face
2) anterior inferior cerebellar artery – facial motor nucleus
3) superficial petrosal branch of the middle meningeal artery – infratemporal facial nerve.
4) Posterior auricular artery - distal to the stylomastoid foramen
Neuroanatomy
1) Facial nerve has 10,000 neurons
2) 7,000 are myelinated and innervate muscles of the face
3) 3,000 are somatosensory and secretomotor and comprise the nervus intermedius.
4) Does not have consistent identifiable topographic orientation to be clinically useful in
selective fascicular nerve grafting
Aetiology
Congenital/Birth
1) Moebius syndrome
2) Hemifacial microsomia
3) Forceps delivery – association with brachial plexus palsy
Acquired
1) Idiopathic
a. Bells Palsy
i. Most common cause (80%)
ii. Associated with diabetes and pregnancy
iii. 85% recover in 3 weeks (wait 3 weeks before tests)
iv. Other 15% 3-6 months
v. Rule of thirds - One third will completely resolve, One third will have
minimal residual deficit, One third will have noticeable residual deficit
b. Melkersson-Rosenthal syndrome
i. Recurrent alternating facial palsy
ii. Furrowed tongue, faciolabial oedema
2) Trauma – second most common cause
a. Temporal bone fractures
b. Extracranial lacerations
i. Should be undertaken within 72hours
ii. Not done if medial to lateral canthus
3) Iatrogenic – surgical, anaesthesia, vaccine
4) Infection
a. Bacterial - Otitis externa
b. Viral - Herpes zoster (Ramsay Hunt), HIV, EBV
c. Atypical – Leprosy, TB, Lyme disease, syphyllis
5) Neoplastic – slowly progressive symptoms
a. Intracranial
i. Meningioma
ii. Acoustic neuroma (Neurofibromatosis type 2)
b. Intratemporal
i. Cholesteatoma
c. Extracranial
i. Parotid tumors
6) Neurologic
a. CVA
b. Guilliam-Barre syndrome
7) Toxic
a. Thalidomide
b. Lead
Investigations
1) Aetiologic
a. Serology
b. bHCG, BSL
c. High res CT
i. Very useful in temporal bone fractures
d. MRI
i. Gadolinium T1 image for nerve oedema
2) Prognostic
a. Nerve excitability test (NET)/Minimal stimulation test
i. Principle: Degeneration of nerve fibers on the paralyzed side is
evidenced by a weaker response to a given current intensity than that
given by the normal side, or by a higher current being required to
produce an equivalent response. Absence of response at high current
settings indicates complete nerve degeneration.
ii. Uses Hilger nerve stimulator
iii. Subjective measure
iv. Abnormal test if 3-3.5mA difference between sides
b. Maximal stimulation test (MST)
i. Similar to NET but uses maximal stimulation -Current is set at 5mA
ii. The observed strength of the muscle contractions on the paralyzed side
compared to those of the normal side indicates the relative number of
nerve fibers responding to stimulation and the degree of nerve
degeneration.
iii. If nerve conduction is neuropraxic, response is positive; if nerve
conduction is degenerated, response is absent.
iv. Sectioned nerve can still be stimulated for 24-72 hours after injury; thus,
the test cannot be interpreted until 3 days later.
v. The test is graded subjectively (equal, decreased, absent), but more
accurate than NET
vi. 92% chance of complete recovery of facial function on the involved
side in Bells Palsy if test is negative
vii. 86% chance of incomplete recovery of facial function if positive test
c. Electroneuronography (ENOG)
i. involves a quantitative analysis of the extent of degeneration. It is not
dependent upon the observer. Most accurate and reproducible test
ii. facial nerve is stimulated at the stylomastoid foramen transcutaneously
iii. compound muscle action potentials are recorded at the nasolabial grove
iv. Performed on both sides with maximal stimulation.
v. Difference between the two sides should be less than 5%.
vi. If difference >95%, 50% chance of poor outcome
vii. Expensive and time consuming
viii. Needs daily measurements for 10 days.
ix. Becomes useless once complete degeneration has occurred. It cannot
be used in facial nerve paralysis which is beyond 3 to 4 weeks old.
x. The most accurate method of selecting patients requiring surgical
intervention
d. Electromyography (EMG)
i. determines the amount of activity of muscle itself. It records motor unit
potentials of voluntary and involuntary muscle contraction, as well as
spontaneous muscle fiber activity.
ii. Does not become positive until 2-3 weeks post insult
iii. Degeneration of lower motor neuron is followed by fibrillation
potentials at 14-21 days.
iv. Polyphasic potentials can be observed 6-12 weeks before clinical
improvement.
3) Topographic
a. Schirmer’s test
i. Measures lacrimal tear secretion
ii. filter paper in contact with the conjunctiva acts as an irritant,
stimulating an increased flow of tears.
iii. length of the wetted portion of the strip after 5 minutes is measured
and is proportional to the volume of tears produced.
iv. defect in either the afferent or efferent limb of this reflex could cause a
reduced flow
v. reduction of more than 30% or less than 25 mm in 5 minutes is
significant.
vi. Abnormal = lesion proximal to geniculate ganglion
b. Stapedius reflex
i. If the lesion involves the nerve proximal to the branch to the stapedius
muscle, the stapedius muscle does not contract and no change in
impedance is evident when testing the acoustic reflex.
ii. elicited by either ipsilateral or contralateral acoustic stimulation
iii. if bilateral severe hearing loss, by tactile or electrical stimulation.
iv. >50% difference in amplitude is considered abnormal.
v. As the reflex recovers at the same time clinical movement recovers, it
has no prognostic significance
vi. A present stapedial reflex would localize the facial injury distal to the
second genu of the nerve
c. Taste testing
i. subjectively assessed by testing with the five basic sensations or
quantified rapidly and objectively by electrogustometry.
ii. have some predictive value since the sensation of taste recovers earlier
than clinical movement is observed.
iii. Abnormal = lesion proximal to stylomastoid foramen
iv. Localisation difficult as nerve branch point is variable
d. Salivary Flow
i. Submandibular duct canulation required
ii. salivary flow is measured in response to a gustatory stimulus.
iii. An abnormal result is a reduction of 25% in salivary flow compared to
the noninvolved side.
iv. difficult to perform and prone to measurement bias.
e. Salivary pH
i. poor localizing potential.
f.
Imaging – CT/MRI
Facial Nerve Grading
House-Brackman
Used to evaluate disorders in which the facial nerve trunk remains continuous
A. Grade 1: Normal Facial Nerve Function
B. Grade 2: Mild Facial Nerve Dysfunction
1. Gross
a. Slight weakness on close examination
b. Synkinesis slight
2. Rest: Normal symmetry and tone
3. Motor Exam
a. Forehead: Moderate to good function
b. Eyes: Complete closure with minimum effort
c. Mouth: Slight asymmetry
C. Grade 3: Moderate Facial Nerve Dysfunction
1. Gross:
a. Obvious difference between sides (not disfiguring)
b. Synkinesis noticeable
2. Rest: Normal symmetry and tone
3. Motor Exam
a. Forehead: slight to Moderate movement
b. Eyes: Complete closure with effort
c. Mouth: Slightly weak with maximal effort
D. Grade 4: Moderately Severe Facial Nerve Dysfunction
1. Gross
a. Obvious weakness
b. Disfiguring asymmetry
2. Rest: Normal symmetry and tone
3. Motor Exam
a. Forehead: No motor function
b. Eyes: Incomplete closure
c. Mouth: Asymmetric with maximal effort
E. Grade 5: Severe Facial Nerve Dysfunction
1. Gross: Barely perceptible motion
2. Rest: Asymmetry
3. Motor Exam
a. Forehead: No motor function
b. Eyes: Incomplete closure
c. Mouth: Slight movement
F. Grade 6: Total Facial Nerve Paralysis
Grade
Description
Measurement*
Function %
I
Normal
8/8
100
II
Slight
7/8
76 - 99
III
Moderate
5/8 - 6/8
51 - 75
IV
Moderately
Severe
3/8 - 4/8
26 - 50
V
Severe
1/8 - 2/8
1 - 25
VI
Total
0/8
0
* "Measurement" is determined by measuring the superior movement of the mid-portion of the
superior eye brow and the lateral movement of the oral commissure. A scale point of 1 is assigned for
each 0.25 cm of motion up to 1 cm. for both eye brow and commisure movement. The points are then
added together. Thus, a total of 8 points can be obtained, if each structure moves 1 cm.
Synkinesis
1) most frequently involves mouth movements with lid closure (orbicularis oculi with
upper lip elevators or zygomaticus major), followed by mouth movements with brow
wrinkling.
2) asymmetry of palpebral fissure and distortion of communicative facial expression
3) only occur in patients where facial nerve has degenerated
4) is caused by the misdirection of regenerated nerve fibers
5) Associated with hypertonia (enhanced excitability of facial nerve neurons)
Management
Treatment is determined by
1) Aetiology
2) prognosis for recovery
3) duration of paralysis
a. motor end-plates degenerate after 2 years (18-36 months reported)
b. best results within 1 year
4) age of patient
Assess face at rest, during voluntary and reflex emotional movement.
Determine total versus partial paralysis and unilateral versus bilateral involvement.
Assess symmetry at rest and during movement and the presence and degree of synkinesis.
Note the severity of brow ptosis, ectropion, nasal valving and oral commissure incompetence.
Identify other cranial nerve or neurologic deficits and significant soft-tissue volume deficits in
addition to the paralysis.
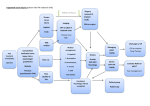
Seiff described 6 stages in the management of facial nerve palsy. (Each stage should be
considered in order, and 2 or more staged procedures may be performed at the same time.)
Stage 1 - Supportive care (ie, lubricants, moisture chambers)
Stage 1A- Tarsorrhaphy (temporary vs permanent)
Stage 2 - Planning facial reanimation (ie, direct facial nerve repair, autologous nerve
grafting, cross-facial nerve grafting, facial suspension with fascia lata, alloplastic material)
Stage 3 - Lower eyelid and lateral canthal resuspension (helps with closure, enhances
lacrimal pump)
Stage 4 - Passive upper eyelid animation (ie, gold weight placement)
Stage 5 - Dynamic eyelid animation (ie, palpebral springs, silicone sling)
Stage 6 - Soft tissue repositioning (ie, direct brow lift, conservative blepharoplasty)
Medical Therapy
1) Treatment of primary disorder
a. Prednisolone for Bell’s Pasly
b. Acyclovir and prednisolone for Herpes Zoster
c. IV antibiotics for otitis externa/mastoiditis
2) Loss of blink reflex
a. Frequent use of Artificial tears
b. Protective glasses with side pieces
c. Avoid grinding, sanding, or sawing
d. At night:
i. Apply bland ointment ( Lacri-Lube)
ii. Tape eye shut
Surgery
Surgical goals of reconstruction:
1) facial function
a. loss of closure of the eye lid to corneal exposure – ulceration scar and blindness
b. flaccidity of cheek and lip may lead to problems with articulation
c. drooping of the lower lip may result in drooling
d. loss of nasalis may lead to problem with airway patency
2) Facial symmetry at rest/repose
3) Absence of synkinesis or mass movement
4) Voluntary facial movement
5) Spontaneous facial expression
No single technique will achieve all these goals
Procedures can be:
1) Restoration of neural input (viable ipsilateral facial muscles)
2) Replace non-functioning facial muscles
3) Static resuspension of soft tissues
4) Adjunctive procedures
Restoration of neural input
Primary nerve repair
1) Tension free – graft if required (usually >2cm gaps)
2) Match endoneural surfaces
3) Will give the best results if done early
4) More proximal lesions give more mass contractions
5) Rerouting intratemporal facial nerve gives an additional 1cm length
6) Planned radiation therapy is not a contraindication to facial nerve repair. Regeneration of
nerve function has been demonstrated despite subsequent ablative doses of radiation.
Ipsilateral nerve graft
1) common donors
a. great auricular nerve
i. 10cm, Can be traced to its 3 terminal branches
ii. Numb earlobe
b. Sural nerve
i. 35cm nerve
c. Medial cutaneous nerve of the arm
i. 15cm, distal branches can be used for pes anserinus
2) Results not as good as with primary repair (more incomplete reinnervation of facial
divisions, decreased voluntary contractions, and more severe synkinesis)
Cross facial nerve graft
Smith and Scaramella, working independently (1971)
Indicated when
1) proximal ipsilateral facial nerve stump is not available
a. only method that will restore spontaneous expressions
2) distal ipsilateral nerves intact
3) facial muscles viable (denervated for <1 year)
Advantages
1) symmetrical voluntary facial movements
2) good resting tone and symmetry
Disadvantages
1) less regenerating axons – weaker facial muscles compared to nerve transfers
2) donor site morbidity
Degree of recovery dependent on
1) Axon profile of the CFNG
2) Time between onset of facial paralysis and reinnervation procedure
Other variations
1) Use of hypoglossal-ipsilateral facial nerve as babysitter while waiting for CFNG to
innervate – monitor with Tinel’s sign
2) One stage sacrifice of contralateral marginal mandibular nerve
Cranial Nerve Transfers
Advantages
1) Reliable neural reinnervation – better in lower 2/3rd face than upper 1/3rd
2) Provides good resting tone and symmetry
Disadvantages
1) donor site morbidity
2) synkinesis (mass movement)
3) hypertonia
a. regenerating axons may be greater than in native facial nerve
4) unpredictable in restoring voluntary movements
Techniques
1) Hypoglossal-Facial (Korte 1901)
a. Classically involves exposure via a parotidectomy incision, identification and
complete transection of the ipsilateral hypoglossal nerve just distal to the takeoff
of the descendens hypoglossi, and direct anastomosis to the distal facial nerve
trunk
i. Hemitongue atrophy
1. Articulation problems (with B, P and L sounds)
2. Difficulty manipulating food bolus in oral phase of swallowing
– contraindicated if CN IX and X also paralysed
3. Improves with time (improved buccal, orbicularis tone)
ii. Involuntary grimacing with normal tongue movements
1. The better the recovery, the worse the synkinesis
2. Most severe in eyelids
iii. No spontaneous facial expression
b. Nerve of choice in bilateral facial nerve palsy
2) Hypoglossal-Facial-Sural Interpositional nerve graft
a. May 1991 – hemisection of hypoglossal nerve and end-side sural cable graft
from there to facial nerve branches.
b. Preserves tongue function with mild or moderate hemiglossal atrophy
c. Facial motor function less strong but less synkinesis
3) Accessory-Facial
a. Shoulder girdle weakness, reduction in ROM
b. May get chronic shoulder pain
c. Variation: use branch to sternomastoid, preserving trapezius innervation
Other nerves: Phrenic, Ansa hypoglossal, Trigeminal branches
Replacement of Non-Functioning Muscles
Historical
Thompson transfer
Thompson method (1971)
Use of nonvascularised free muscle grafts (PL and EDB muscles)
Variable results – success due to direct neurotization from contralateral intact facial
muscles
Indications
1) Long standing paralysis (3-4 years)
2) Lack of intact neuromuscular units due to fibrosis, degeneration/atrophy or congenital
absence
3) Patient physiologically, physically and mentally compliant to retraining
Regional muscle transfers
1) Temporalis
a. Mostly for lateral corner of the mouth and to re-establish a voluntary smile.
b. vector of the temporalis muscle transposition is similar to zygomaticus major muscle
– superolateral and thus results in a lateral smile, which is the most common type
of human smile.
c. can be used to reinnervate the eye, but results in simultaneous closure of the eye
during a smile and incomplete eye closure during sleep with relaxation of the
temporalis muscle.
d. can cause considerable distortion of the lids.
e. Potential for chronic TMJ pain with loss of temporalis support
f.
Variations:
i. Turndown (Rubin)
1. Coronal incision or extended preauricular
2. extend with superficial temporal fascia or pericranial strip)
3. Bulky flap over zygomatic arch (option to resect arch)
4. Temporal hollowing (avoid muscle anterior to temporal hairline)
ii. McLaughlin
1. Intraoral approach
2. Coronoidectomy
3. Transfer muscle via fascial lata strips
McLaughlin Temporalis transfer
2) Masseter
a. Pull in line with buccinator-risorius complex
b. Incision thru intraoral or mandibular margin
c. Disadvantage is vector is in a more horizontal plane, thus providing less superior
angulation to the corner of the mouth.
3) Anterior belly digastric
a. Weakness in marginal mandibular = inability to depress the lower lip and evert the
vermillion border, especially evident during smiling
b. Pull in line with lower lip depressors
c. Used for marginal mandibular nerve palsies
d. Anterior belly – innervation from the nerve to the mylohyoid muscle, a branch of
the inferior alveolar nerve. Blood supply via the submental branch of the facial
artery.
e. Posterior belly arises from the digastric notch of the mastoid process, receives
innervation from the facial nerve and blood supply from a branch of lingual artery
f. Variations
i. Edgerton 1965 – detach insertion and suture to lip via fascial strip
ii. Conley 1982 – turnover flap (diagram below)
iii. Terzis 2000 – uses a cross facial nerve graft to innervate the anterior belly in
older patients. Reeducation/retraining possible in younger patients
tunnelled deep to the depressors of the lower lip, to emerge through the lip incision
4) Platysma
a. as a pedicled muscle to the corner of the mouth.
b. Type II
i. Terzis reports that the dominant vessel in 90% is a direct branch emerging
from the facial artery just proximal to where the marginal manbibular
branch of the facial nerve crosses the facial artery (2cm below mandible)
ii. In 10%, it is a branch from the submental artery.
c. dominant motor nerve supply is the cervical branch of the facial nerve, which
innervates the muscle at the junction of the cranial and middle third of the muscle,
approximately 2 to 3 cm lateral to the direct muscular arterial branch
Cross Face Nerve Grafts and Delayed Free Muscle Flap
1) Advantages of free flap over regional transfer
a. Potential for reinnervation from native facial nerve
b. Soft tissue augmentation can be done at the same time
c. Potential for coordination with contralateral face if using CFNG
2) Free muscle behaviour:
a. Improvement in functional problems such as speech, drooling, and
b. Voluntary and independent movement of the transplanted side with symmetry
at rest can be expected.
c. Regaining involuntary spontaneous and emotional movement remains elusive.
d. Latency of activity in the transplanted muscle may be present, such that rapid
response during conversation or spontaneous movements is absent or
inappropriate.
e. Need to be overcorrected to allow for eventual sagging
3) Supplies a new neuromuscular unit to the face via a free-muscle flap and a grafted donor
cranial nerve, usually a cross-facial nerve graft
4) Involves a 2-stage procedure of cross-facial nerve graft, followed by a delayed freemuscle transfer
5) Rationale for the delay is to prevent atrophy of the muscle graft while waiting for axons
to travel the length of the nerve graft
6) In the absence of an end organ, number of regenerating fibers in CFNG does not
exceed 20%
7) This exceeds the number of axons required for reinnervation of most muscle transfers.
8) Force of muscle contraction is more dependent on donor muscle characteristics than
neural regeneration.
9) Some advocate single-stage procedures :
a. Advantages of 1 stage procedure
i. Simpler, less time consuming
ii. Reduces recovery period
iii. Avoids sural nerve donor site morbidity
iv. matches motor nerve input with motor nerve graft
v. it requires neural ingrowth across 1 versus 2 anastomoses
vi. Maintains vascularity of the nerve graft.
vii. Higher nerve regeneration - the continued presence of a muscle end
organ during nerve graft ingrowth may provide a positive trophic
influence. Graft regeneration rates through a delayed cross-facial nerve
graft rarely exceed 20%.
viii. Shown to give equivalent results
b. Disadvantages:
i. muscle flap undergoes some atrophy and fibrosis during reinnervation
period
ii. if the reinnervation fails, the muscle is unlikely to remain suitable for a
second attempt.
Two Stage Technique
First stage:
1) nerve graft, either from the ipsilateral proximal nerve segment, substituted
cranial nerve, or contralateral facial nerve.
2) Usually anastomosed to redundant zygomaticus branch and tunnelled
subcutaneously and marked.
3) Monitor progress with Tinel’s sign
Second Stage (9-12 months)
1) identify the distal end of the nerve graft and send a frozen section for
confirmation of viable axons
2) Secure the flap to the periosteum of the zygomatic arch and the modiolus
3) Movement can be expected in 6-9 months, with improvement over the
following 2-3 years.
Muscle options
Ideal muscle
4) single dependable vascular pedicle
5) ‘smart’ muscle – high axonal count to muscle fibre ratio
6) Expendable
7) Excursion similar to facial muscle it replaces
8) Multiple slips with independent neurovascular pedicle
9) Adequate bulk (may need more for soft tissue augmentation)
1) Gracilis
a.
b.
c.
c.
d.
First free muscle for facial reanimation (Harii 1976)
i. To deep temporal nerve, superficial temporal vessels and CFNG
up to 3.5 cm (average 1-1.5 cm) of oral commissure movement
Advantages:
iii. relative ease of dissection
iv. adequate neurovascular pedicle
v. muscle fiber length corresponds to zygomaticus major
vi. minimal functional loss
Disadvantage
i. excessive bulk and skin tethering
ii. lack of dual innervation
Can be done as single stage
i. Contralateral facial nerve (O’Brien 1991)
ii. To ipsilateral trigeminal nerve branches
iii. To ipsilateral facial nerve stump
O’Brien 1 stage transfer
e. Manktelow 1984 – principle of minitransfer to address bulk issue
2) Pectoralis Minor
a. Described by Terzis (1982)
b. Advantages
i. strong tendinous insertion, makes it ideal for a "pull-up" muscle for the
restoration of a smile.
ii. Ideal shape, bulk and length
iii. dual nerve supply - making single-stage smile and eye closure
restoration possible by splitting the flap.
iv. Good scar, minimal functional loss
c. Difficult dissection of neurovascular pedicle
d. Taking both nerves may denervate pectoralis major
3) Others:
a. Extensor digitorum brevis
i. Favorable anatomic configuration
ii. Poor contraction force (lack of bulk and excursion)
b. Latissimus dorsi (minitransfer)
c. Rectus abdominus (minitransfer)
d. Rhomboid major (Nakajima 1986 – 1 stage transfer)
e. Abductor hallucis (Jiang 1991 – 1 stage transfer)
f. Serratus Anterior
i. Multiple independent slips
ii. Poor excursion
g. Rectus Femoris (Koshima 1994 – 1 stage transfer)
Nerve targets
1) Ipsilateral facial nerve stump
2) Contralateral distal facial nerve branches
a. Selected by direct electrical stimulation – match smile with smile
3) CN XI, XII
4) Nerve to masseter or temporalis
Vessel targets
1) Superficial temporal vessels
2) Facial vessels
Static resuspension of soft tissues
The goals of static reconstruction are to
1) Correct functional disability
a. Address eyebrow ptosis
b. protect the cornea
c. alleviate external valve obstruction
d. prevent drooling
2) restore facial symmetry at rest
Indications
1) Not suitable for animation – medical comorbidities, age
2) Unwilling to undergo prolonged procedure, rehabilitation
Suspension can be achieved with
1) slings
a. Autograft
i. fascia
1. Disadvantages
a. donor site morbidity
b. stretches with time
c. resorption
2. fascia lata
3. temporalis fascia
ii. local pericranial flaps
b. Allograft
i. Alloderm – freezed dried acellular human dermis
c. Alloplast
i. GorTex
1. Advantages
a. good tensile strength, less stretch
2. Disadvantages
a. extrusion
b. infection
d. May be endoscopically assisted
2) Soft tissue excision/repositioning
Eyebrow Suspension
1) Brow lift
a. Suprabrow excision
i. Most direct lift
ii. Problems – visible scar
b. Endoscopic
2) Brow suspension
a. Fascial lata
b. Gortex
c. Alloderm
Lower Eyelid suspension
To improve lateral visual field
Treatment for paralytic ectropion
1) Lid repositioning procedures
a. Pentagonal wedge resection
i. laxity of the lower lid with good position and definition of the lateral
canthal area.
ii. Preserves pretarsal orbicularis
iii. Does not violate commissure
b. Modified Kuhnt-Szymanowski procedure (Fox 1966)
i. involves removal of a portion of the midtarsal plate,
ii. does not correct the lax lateral canthal tendon
iii. violates commissure
c. Mitak Anchor (PRS Jan 2005)
d. Lateral tarsal strip (Anderson 1979)
i. lateral canthotomy
ii. division of the lateral portion of the lower eyelid into musculocutaneous
and tarsoconjunctival layers
iii. removal of a portion of the conjunctiva
iv. suturing the resulting tarsal strip to the 4-5 mm posterior to the lateral
orbital rim near the Whitnall tubercle, level of inferior pupil
v. violates commissure
Lateral tarsal strip
2) Cheek resuspension
a. Subperiosteal midface with SOOF lift
i. Elevate and resuspend zygomaticus major and levator labii superioris
Subperiosteal midface with SOOF lift
b. Fascial sling
Lower lid sling
Nasal suspension
Nasal valve limits the flow through the nose and accounts for 70 % of nasal inspiratory resistance
Contraction of the dilator naris muscle draws the lateral margin of the nose laterally and cephalad
modulating the function of the nasal valves and controlling the degree of inspiratory resistance
Loss of dilator naris leads to airway collapses on inspiration
1) Resuspension
a. Anchor to base of alar
b. Fascia lata, maxillary periosteal flap, gortex
2) Perialar wedge resection
Oral commissure
Resuspension
a. Improves oral continence and drooling
b. Approximates buccal mucosa to teeth to aid in oral phase of swallowing and
articulation
c. Anchor point temporalis fascia or malar – best point is as close as possible to
zygomatic major
d. 3 points – one each for the upper and lower lip past the midline to the
unparalysed side and 1 in the commissure
Wedge excision lower lip
e. Variation:
i. Hitch contralateral orbicularis to ipsilateral modiolus (I Jackson 2001)
ii. combined with vermilion border advancement to improve oral
competence and symmetry (Glen 1987)
Adjunctive procedures
Eye Issues
Opthalmic problems
1. eyebrow and forehead ptosis
2. secondary dermatochalasis
3. upper eyelid retraction
4. lower eyelid paralytic ectropion with failure of the lacrimal pump
5. decreased blink and forced closure
6. loss of corneal squeegee effect
7. decreased tear production
8. epiphora
these may lead to
1. Exposure keratitis
2. Corneal ulcer corneal erosion +/- perforation
3. Decreased vision due to above
Management of lagopthalmos
Nonsurgical
Aim to provide comfort and protect the cornea from trauma and drying.
Include artificial tear and eye ointments, lid taping at night, soft contact lenses, scleral shells,
punctal plugs if dryness is a problem
Surgical
Consider if paralysis is permanent
Includes:
1) Tarsorrhaphy
a. Should be avoided as a permanent solution if possible and outcomes are
cosmetically and functionally poor
b. decrease horizontal lid opening,
c. provide better support of the precorneal lake of tears
d. provide better coverage of the eye during sleep
e. Types
i. Temporary
1. suture tarsorrhaphy – mattress sutures across upper/lower lids
2. overlapping lateral tarsorrhaphy (McLaughlin 1951)
McLaughlin tarsorrhaphy
ii. Permanent
1. Performed by removing the lateral half of superficial upper and
lower eyelid margins along the grey lines
2. The depeithelialized margin is split vertically 2-3mm into the
tarsus with a scalpel to create a tarsal groove
3. mattress sutures placed into the base of these grooves
2) Lateral canthoplasty (tarsal strip)
3) Passive upper eyelid animation/loading
a. Tantalum wire and mesh (Sheehan 1950)
b. Lead (Smellie 1966 – 0.75gm found to be ideal)
c. Gold weight (Barclay 1969)
i. 99% pure, 10x5mm, 0.6gm-2.8gm (0.2gm increments)
ii. Inert
iii. Dense (heavy but not bulky)
iv. Color similar to fat
v. Anchoring reduces extrusion and migration significantly
vi. Gravity dependent – dynamic in some positions only
vii. May worsen astigmatism (more common in tarsal placements)
viii. Estimate weight with preop taping in erect position and overcorrect
slightly (external sizing weights available)
ix. Placement may be septal, mid-pretarsal or low-pretarsal – lower
pretarsal placement is more obvious but gives mechanical advantage
thus less weight required.
Gold weight placement: A=pretarsal B=septal
4) Dynamic Eyelid animation
a. Palpebral spring (Morel-Fatio 1964)
i. Dynamic, able to close in any position
ii. Gives a fast blink
iii. Need for frequent adjustments
iv. High risk of extrusion
Palpebral spring
b. Arion sling (Arion 1972)
i. Silicone palpebral sling (0.8mm silicone rods)
ii. subject to stress, relaxation, and breakage.
iii. Most needs revision/adjustments
c. Magnets (Mühlbauer 1973)
i. miniaturized, siliconized, curved magnets
ii. the extrusion rate is unacceptably high.
d. Pedicled: temporalis muscle-fascia unit
i. circumorbital sling and motor unit.
ii. bulky
iii. progressive muscle atrophy and functional disability.
e. Free: Platysma muscle as sphincter (Terzis)
Epiphora
epiphora may be caused by ectropion, functional canalicular obstruction, or gustatory
lacrimation ("crocodile tears").
ectropion and functional canalicular obstruction result from a reduced function of the
paralysed orbicularis muscle
crocodile tearing results from misrouting of regenerating nerve fibres
Nasal Airway
Apart from resuspension, also consider:
Nasal septal reconstruction/resection
Reduction of hypertrophic inferior turbinates
Medical management of allergies
Oral Commissure
Adjunctive procedures
plication orbicularis
orbicularis advancement for commissure reconstruction
excision/reconstruction of nasolabial fold
Role of BOTOX
control synkinesis or mass action
balance lower lip depressor dysfunction
Marginal mandibular nerve palsy
Clinical
Three types of smile (Rubin):
(1) “Mona Lisa” or zygomaticus major dominant smile
(2) “canine” or levator labii superioris dominant smile
(3) “full denture” or all muscles dominant smile.
Depressor muscle function is an important component of the full denture smile.
depressor muscles are actively used to express other human expressions such as
sadness, anger, rage, depression, and sorrow.
lower lip is animated through a complex interaction of orbicularis oris, depressor labii
inferioris, depressor anguli oris, mentalis, and platysma muscles.
MMN palsy leads to inability to move the lower lip down or laterally, or to evert the
vermilion border on the affected side, due to paralysis of the depressor anguli oris
and depressor labii inferioris muscles which are supplied by the nerve.
Elevation of the lower lip of the paralysed side results during smiling resulting in less
mandibular teeth being visible - lower lip appears flattened and inwardly rotated
compared to the normal side
Left MMN palsy
Differentiate from cervical branch palsy (pseudoparalysis of MMN) where patient
can evert lower lip (mentalis functional) – may look very similar
Treatment strategies
Balancing procedure
Myotomy and myomectomy of the elevator muscles on the paralysed side or of the
depressor muscles on the normal side
Neurolysis of the MMN on the normal side
May test with effect of surgery during consultation using local anaesthetic injection
into the depressor muscles.
Chemical denervation (Botox) injected into the contralateral depressors and platysma
Cross facial nerve graft
In patients with facial paralysis of less than 12 months’ duration who had evidence of
muscle viability after needle electromyelography
Neurotisation
direct neurotization of the depressor muscle with XII nerve fibers. Often required
nerve grafting (Terzis)
epimysium is sutured over the nerve end with 9-0 nylon by taking a small bite of the
epineurium to secure the nerve in position.
Indicated if incomplete recovery of the depressor muscle function after cross-facial
nerve graft, or in patients with facial paralysis of 24 months’ duration and evidence of
remaining depressor muscle after needle electromyography
Nerve transfer
Reinnervation of the depressors of the lower lip using the descending branch of
the hypoglossal nerve.
Regional muscle transfer
anterior belly of digastric transfer and platysma best options
temporalis or masseter muscle transfer to the lower lip provides only partial
correction because the direction of pull is different.
patient with Bell’s palsy usually has uninvolved platysma muscle; in these cases,
platysma transfer is the procedure of choice.
Free muscle transfer
1. Extensor digitorum brevis (2 stage)
o Stage 1 – sural nerve graft to contralateral buccal branch
o Stage 2 – free EDB flap (lateral tarsal branch of the dorsalis pedis artery with
two accompanying venae commitantes. The motor supply is from a branch
of the anterior tibial nerve.)
2. Ueda (PRS 1995) - double muscle transfer to substitute for lip elevation and
depressor muscle function. latissimus dorsi for upper lip elevation and a slip of the
serratus anterior for depressor muscle
3. Koshima performed a double- muscle transfer by using a divided rectus femoris
muscle for one-stage reconstruction of both the zygomaticus major muscle and
depresor labii inferioris muscle.
Tulley (BJPS 2000) – Anterior belly transfer found to be procedure of choice