* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Encorine System and Homeostasis
Neuroendocrine tumor wikipedia , lookup
Cardiac physiology wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Mammary gland wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Growth hormone therapy wikipedia , lookup
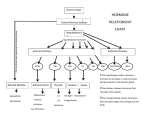
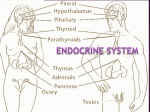
The Endocrine System The hormones of the endocrine system regulate the physiologic and metabolic activities and growth of target cells in the body. Comparison of Control by the Nervous and Endocrine Systems The nervous and endocrine systems act together to coordinate functions of all body systems. Nervous system acts through nerve impulses conducted along axons of neurons. At synapses, nerve impulses trigger the release of chemical mediators, the neurotransmitters. The endocrine system releases mediators, the hormones. The control of the two systems is different. Responses of the endocrine system are slow acting and prolonged, compared to the responses of the nervous system. Although some hormones act within seconds most take several minutes or more to cause a response. Effects of nervous system activation are generally briefer than those of the endocrine system. The nervous system acts on specific muscles and glands. The influences of the endocrine system are broader and regulate virtually all types of body cells. A hormone is a mediator molecule that is released in one part of the body but regulates the activity of cells in other parts of the body. The circulating blood delivers hormones to cells throughout the body. Both neurotransmitters and hormones exert their effects by binding to receptors on or in their target cells. Several mediators act as both neurotransmitters and hormones. Endocrine glands Endocrine glands secrete their products (hormones) into the interstitial fluid from the secretory cells that produced the hormones. From the interstitial fluid, hormones diffuse into capillaries and the blood carries them to target cells throughout the body. The circulating concentrations of the hormones are low. Functions of Hormones 1. Help regulate: Chemical composition and volume of internal environment (interstitial fluid) Metabolism and energy balance Contraction of smooth and cardiac muscle fibers Glandular secretions Some immune system activities. 2. 3. 4. Control growth and development. Regulate operation of reproductive systems. Help establish circadian (day-night) rhythms. Control of Hormone Secretion The release of most hormones occurs in short bursts, little or no secretion between bursts. Regulation of secretion normally prevents overproduction or underproduction of the hormones. 1 Hormone secretion is regulated by the nervous system, chemical changes in the blood, and other hormones. Most hormonal regulatory systems work via negative feedback, few operate via positive feedback. Hypothalamus and Pituitary Gland Hypothalamus The hypothalamus a small region of the brain below the thalamus is the major link between the nervous and endocrine systems. The hypothalamus receives input from the limbic system, cerebral cortex, thalamus, and reticular activating system, sensory signals from internal organs and from the retina. The hypothalamus in the nervous system is an important regulatory center of the endocrine system as well as an endocrine gland itself. The hypothalamus (9) and the pituitary gland (7) secrete 16 hormones which play important roles in the regulation of virtually all aspects of growth, development, metabolism and homeostasis. Pituitary Gland The pituitary gland is a pea-shaped structure that lies in the sella turcica of the sphenoid bone. It attaches to the hypothalamus by the infundibulum and has two anatomically functionally separate lobes. Anterior pituitary (anterior lobe) or adenohypophysis (adeno- means gland) consists of two parts, the pars distalis and the pars tuberalis. The posterior pituitary (posterior lobe) or neurohypophysis also consists of two parts the pars nervosa and the infundibulum. Posterior pituitary contains axons and axon terminals of neurons whose cell bodies are located in the hypothalamus. A third region of the pituitary gland called the pars intermedia. Anterior Pituitary The anterior pituitary or adenohypophysis secretes hormones that regulate activities from growth to reproduction. Release of anterior pituitary hormones is stimulated by releasing hormones and suppressed by inhibiting hormones from the hypothalamus. Hypothalamic hormones are an important link between the nervous and endocrine systems. Hypophyseal Portal System Hypothalamic hormones reach the anterior pituitary through a portal system. In a portal system blood flows from one capillary network into a vein then into a second capillary network without passing through the heart. In the hypophyseal portal system blood flows from capillaries in the hypothalamus into portal veins in the infundibulum that carry blood to capillaries of the anterior pituitary. Specialized neurons, called neurosecretory cells, synthesize the hypothalamic releasing and inhibiting hormones. The hormones then diffuse into the hypophyseal portal system. This direct route permits 2 hypothalamic hormones to act immediately on anterior pituitary cells, before the hormones are diluted or destroyed in the general circulation. Hormones secreted by anterior pituitary cells pass into capillaries, then drain into veins and out into the general circulation to target tissues throughout the body. Hormones of the anterior pituitary gland that influence other endocrine glands are called tropic hormones or tropins. Control of Secretion by the Anterior Pituitary Secretion of anterior pituitary hormones is regulated in two ways. 1. Neurosecretory cells in the hypothalamus secrete five releasing hormones which stimulate secretion of anterior pituitary hormones and two inhibiting hormones which suppress secretion of anterior pituitary hormones. 2. Negative feedback of the hormones released by target glands decreases secretions anterior pituitary cells. In such negative feedback loops the secretory activity decreases when blood concentrations of their target gland hormones rise. Human Growth Hormone and Insulin-like Growth Factors Human growth hormone (hGH) or somatotropin is the most plentiful anterior pituitary hormone. Main function of hGH is to promote synthesis and secretion by the cells of the body of small protein hormones called insulin-like growth factors (IGFs) or somatomedins. IGFs cause cells to grow and multiply by increasing protein synthesis. Due to the effects of the IGFs and hGH there is an increase the growth rate of the skeleton and skeletal muscles during childhood and the teenage years. In adults, IGFs and hGH help maintain the mass of muscles and bones and promote tissue repair. Low blood glucose circulating to the hypothalamus promotes release of GHRH to cause release of hGH. High blood glucose circulating to the hypothalamus stimulates release of GHIH to inhibit release of hGH. Thyroid-Stimulating Hormone Thyroid-stimulating hormone (TSH) stimulates the synthesis of the two thyroid hormones, triiodothyronine (T3) and thyroxin (T4) by the thyroid gland. Thyrotropin-releasing hormone (TRH) from the hypothalamus controls TSH secretion. Release of TRH and TSH depends on blood concentrations of T3 and T4 via negative feedback. Follicle-Stimulating Hormone In females, the ovaries are the targets for follicle-stimulating hormone (FSH). FSH initiates the development of several ovarian follicles, a spherical arrangement of secretory cells that surround a developing oocyte. FSH also stimulates follicular cells to secrete estrogens. In males, FSH stimulates sperm production in the seminiferous tubules of the testes. Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates FSH release. Luteinizing Hormone In females, luteinizing hormone (LH) triggers ovulation of a secondary oocyte (future ovum) by an ovary. LH stimulates formation of the corpus luteum from the ovulated follicle and secretion of progesterone by the cells of the corpus luteum. FSH and LH also stimulate secretion of estrogens by the corpus luteum cells. Estrogens and progesterone prepare the uterus for implantation of a fertilized ovum and help prepare the mammary glands for milk secretion. In males, LH or interstitial cell 3 stimulate hormone (ICSH) stimulates the interstitial cells of the testes to secrete testosterone. Secretion of LH is controlled by gonadotropin-releasing hormone (GnRH). Release of GnRH, FSH and LH is suppressed by estrogens and testosterone through negative feedback systems. Prolactin Prolactin (PRL) along with other hormones initiates and maintains milk secretion by the mammary glands. Ejection of milk from the mammary glands depends on oxytocin released from the posterior pituitary. Milk secretion and ejection constitute lactation. Adrenocorticotropic Hormone Adrenocorticotropic hormone (ACTH) controls the production and secretion of glucocorticoids by the cortex (outer portion) of the adrenal glands. Corticotropin-releasing hormone (CRH) from the hypothalamus stimulates secretion of ACTH by corticotrophs. Glucocorticoids inhibit CRH and ACTH release via negative feedback. Posterior Pituitary The posterior pituitary or neurohypophysis does not synthesize hormones. It stores and releases two hormones oxytocin (OT) and antidiuretic hormone (ADH) or vasopressin. The posterior pituitary consists of axon terminals of hypothalamic neurosecretory cells. The cell bodies of the neurosecretory cells are in the hypothalamus and the axons form hypothalamic-hypophyseal tract in the infundibulum. This tract begins in the hypothalamus and ends in the posterior pituitary. The cell bodies of neurosecretory cells produce the OT and ADH in secretory vesicles. The vesicles then move through the axons to the axon terminals in the posterior pituitary where they are stored until nerve impulses trigger release of the hormones. Oxytocin During and after delivery of a baby, OT affects two target tissues; the mother’s uterus and breasts. During delivery, OT enhances contraction of smooth muscle in the wall of the uterus. After delivery, OT stimulates milk ejection (“letdown”) from the mammary glands in response to the mechanical stimulus provided by the sucking of the infant on the nipple. Antidiuretic Hormone ADH causes the kidneys to return more water to the blood, thus decreasing urine volume. ADH also causes constriction of arterioles which increases blood pressure. This is why it is also called vasopressin. Thyroid Gland Spherical sacs called thyroid follicles make up most of the thyroid gland. The follicular cells produce two hormones of the thyroid gland thyroxin or tetraiodothyronine (T4), contain four atoms of iodine and triiodothyronine (T3), contains three atoms of iodine. Parafollicular cells or C cells, which lie between follicles, produce calcitonin. 4 Actions of Thyroid Hormones T3 and T4 exert their effects throughout the body. 1. Thyroid hormones increase basal metabolic rate (BMR) by stimulating the use of cellular oxygen to produce ATP by increasing the metabolism of carbohydrates, lipids and proteins. 2. As cells use more ATP, more heat is given off, and body temperature rises this is a calorigenic effect of the thyroid hormones. Calcitonin The hormone produced by the parafollicular cells of the thyroid gland is calcitonin (CT). CT decreases the concentration of calcium in the blood by inhibiting the action of osteoclasts, the cells that break down bone extracellular matrix. When Ca2+ ion blood concentration is high, calcitonin lowers the amount of blood calcium by inhibiting bone resorption (breakdown of bone extracellular matrix) by the osteoclasts and accelerating uptake of calcium into bone extracellular matrix. Parathyroid Gland Parathyroid Hormone or Parathormone Parathyroid hormone (PTH) is the major regulator of the concentrations of calcium Ca2+ and phosphate (HPO42-) ions in the blood. Action of PTH is to increase the number and activity of osteoclasts. The result is elevated bone resorption, which releases ionic calcium (Ca2+) and HPO42- into the blood. PTH also acts on the kidneys in 3 ways. 1. PTH slows the rate at which Ca2+ ions is lost into the urine so increases blood Ca2+ ion concentration. 2. PTH increases loss of HPO42- ions into the urine. 3. PTH promotes formation of the hormone calcitriol, the active form of vitamin D. Calcitriol increases the rate of Ca2+ion absorption from the GI tract into the blood. The blood calcium concentration directly controls the secretion of both calcitonin and PTH by negative feedback loops that do not involve the pituitary gland. 1. A higher than normal concentration of (Ca2+) ions in the blood stimulates parafollicular cells of the thyroid gland to release more calcitonin. 2. Calcitonin inhibits the activity of osteoclasts, thereby decreasing the blood Ca2+ ion concentration. 3. A lower than normal concentration of Ca2+ ions in the blood stimulates chief cells of the parathyroid gland to release more PTH. 4. PTH promotes resorption of bone extracellular matrix, which releases Ca2+ions into the blood and slows loss of Ca2+ ions in the urine, raising the blood concentration of Ca2+ ions. 5 5. PTH also stimulates the kidneys to synthesize calcitriol, the active form of vitamin D. 6. Calcitriol stimulates increased absorption of Ca2+ ions from the GI tract which helps increase the blood concentration of Ca2+ ions. Adrenal Glands Adrenal Cortex The adrenal cortex is subdivided into three zones, each of which secretes different hormones. The outer zone, zona glomerulosa secrete mineralocorticoids hormones because they affect mineral homeostasis. The middle zone, zona fasciculata secrete mainly glucocorticoids hormone because they affect glucose homeostasis. The inner zone, zona reticularis, secretes androgens, which have masculinizing effects. Mineralocorticoids Aldosterone the major mineralocorticoid regulates homeostasis of two mineral ions Na+ and K+ ions and helps adjust blood pressure and blood volume. The renin-angiotensin-aldosterone (RAA) pathway controls secretion of the aldosterone. Glucocorticoids The glucocoticoids regulate metabolism and resistance to stress are cortisol (hydrocortisone), corticosterone and cortisone. Cortisol is the most abundant. Glucocorticoids have the following effects: 1. Protein breakdown - Glucocorticoids increase the rate of protein breakdown. The amino acids formed are then used for synthesis of new proteins or for ATP production. 2. Gluconeogensis (glucose formation) - Upon stimulation by glucocorticoids, liver cells convert certain amino acids and lactic acid to glucose. 3. Lipolysis - Glucocorticoids stimulate lipolysis, the breakdown of triglycerides and release of fatty acids from adipose tissue into the blood. 4. Resistance to stress - Glucocorticoids promote resistance to stress, as the additional glucose provides tissues with a ready source of ATP. 5. Anti-Inflammatory effects - Glucocorticoids inhibit white blood cells that participate in inflammatory responses. 6. Depression of immune responses - Glucocorticoids depresses immune responses. Glucocorticoids are prescribed for organ transplant recipients to retard tissue rejection by the immune system. 6 Androgens In both males and females, the adrenal cortex secretes small amounts of androgens. The amount of androgens secreted by the adrenal gland is usually so low that their effects are insignificant. In females, adrenal androgens promote libido (sex drive) and are converted into estrogens (feminizing sex hormone) by other body tissues. After menopause all estrogens come from conversion of adrenal androgens. Adrenal medulla The inner region of the adrenal gland, the adrenal medulla, is a sympathetic ganglion of the autonomic nervous system (ANS). The two major hormones synthesized by the adrenal medulla are epinephrine (E) and norepinephrine (NE). The medullary hormones intensify sympathetic responses in other parts of the body. These hormones increase heart rate and force of contraction, which increases blood pressure and increases blood flow to the body organs. Pancreatic Islets The pancreas is both an endocrine and exocrine gland. Scattered among the exocrine acini are pancreatic islets, the islets of Langerhans. Cell Types in the Pancreatic Islets 1. Alpha (α) cells constitute about 17% of pancreatic islet cells and secrete glucagon. 2. Beta (ß) cells constitute about 70% of pancreatic islet cells and secrete insulin. Glucagon raises blood glucose concentration and insulin lowers it. Regulation of Glucagon and Insulin Secretion The principal action of glucagon is to increase blood glucose concentration when the blood glucose concentration falls below normal. Insulin helps lower blood glucose concentration when the blood glucose is too high. The concentration of blood glucose controls secretion of glucagon and insulin via negative feedback without intervention of pituitary tropic hormones. 7 Disorders of the Endocrine System Disorders of the endocrine system involve hyposecretion, inadequate release of a hormone or hypersecretion, excessive release of a hormone. Pituitary Gland Disorders Pituitary Dwarfism, Giantism, and Acromegaly Disorders of the anterior pituitary involve human growth hormone (hGH). Hyposecretion of hGH during the growth years slows bone growth and the epiphyseal plates close before normal height is reached. This condition is pituitary dwarfism. Hypersecretion of hGH during childhood causes giantism, abnormal increase in the length of long bones. Person grows to be very tall, body proportions are normal. Hypersecretion of hGH during adulthood is called acromegaly, the bones thicken and other tissues enlarge, body proportions are abnormal. Diabetes Insipidus Diabetes insipidus is an abnormality associated with dysfunction of the posterior pituitary due to hyposecretion of ADH, thus a great volume of water is lost in the urine. Thyroid Gland Disorders Congenital hypothyroidism, hyposecretion of thyroid hormones that is present at birth is termed cretinism. Cretinism causes severe mental retardation and stunted bone growth. Hyperthyroidism is Graves’s disease. Graves’s disease is an autoimmune disorder in which the person produces antibodies that mimic the action of thyroid-stimulating hormone (TSH). The antibodies continually stimulate the thyroid gland to grow and produce thyroid hormones causing an enlarged thyroid gland. Parathyroid Gland Disorders Hypoparathyroidism (low PTH concentration) leads to a deficiency of blood Ca2+ ions, which causes neurons and muscle fibers to depolarize and produce action potentials spontaneously. This leads to twitches, spasms, and tetany (maintained contraction) of skeletal muscle. Hyperparathyroidism (high PTH concentration) causes excessive resorption of the bone matrix, raises the blood concentrations of Ca2+ and HPO42- ions and causes bones to become soft and easily fracture. 8 Adrenal Gland Disorders Cushing’s Syndrome Cushing’s syndrome is due to hypersecretion of cortisol by the adrenal cortex. The elevated concentration of cortisol causes hyperglycemia, osteoporosis, weakness, hypertension, increased susceptibility to infection, decreased resistance to stress and mood swings. Addison’s Disease Hyposecretion of glucocorticoids and aldosterone causes Addison’s disease (adrenocortical insufficiency). Addison’s disease is an autoimmune disorder in which antibodies cause adrenal cortex destruction or block binding of ACTH to its receptors. Pancreatic Islet Disorders Diabetes mellitus is the endocrine disorder caused by an inability to produce or use insulin. Because insulin is unavailable to aid transport of glucose into body cells, blood glucose concentration is high and glucose “spills” into the urine (glucosuria). Diabetes mellitus causes polyuria, excessive urine production due to an inability of the kidneys to reabsorb water; polydipsia, excessive thirst and polyphagia, excessive eating. There are two types of diabetes mellitus. Type 1 diabetes, insulin-dependent diabetes mellitus (IDDM) the insulin concentration is low because the person’s immune system destroys the pancreatic ß cells. Type 2 diabetes, non-insulin-dependent diabetes mellitus (NDDM) most often occurs in obese people. Type 2 diabetic individual has a sufficient amount (or even a surplus) of insulin is in the blood. The diabetes is caused by target cells of the body become less sensitive to the insulin. 9