* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Introduction to Blood Cells
Immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Atherosclerosis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Plasmodium falciparum wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
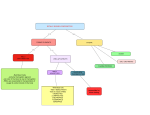
WEEK 4 CELL BIOLOGY – INTRODUCTION TO BLOOD CELLS PRE-WEEK PREPARATION LEARNING OBJECTIVES This self-learning module is designed to meet the following end of week objective(s): 1. Identify and describe the functional characteristics of different immune cells (i.e. neutrophils, lymphocytes, macrophages, etc.). By completing this pre-week preparation and further learning during the week, the learner should be able to: 1. Describe the classification of blood cells in terms of the myeloid and lymphoid cell lineages. 2. Describe the morphological appearance and function of different blood cells includiing erythrocytes, leukocytes (neutrophils, eosinophils, basophils, monocyte/macrophages, lymphocytes), and platelets. 3. Describe the structure and function of normal hemoglobin and other variants of hemoglobin (HbF and HbA1c). 4. Describe the oxygen-dissociation curves for HbA, the factors that can influence the shape of the curve, and compare with the oxygen-affinity of HbF and myoglobin. INTRODUCTION Blood has many different functions in the body. It allows for transportation of oxygen and carbon dioxide between the lungs and the other organs and tissues of the body. Nutrients absorbed from the gastrointestinal tract can be transported around the body, and waste products delivered to the liver or kidneys for detoxification or removal. Many hormones travel within the blood to reach their target cells or tissues. Blood plays a role in temperature regulation, with increased or decreased blood flow to the skin used to control temperature. Blood contains cells that play an important role in inflammation and immune defence. Finally, blood contains cells and proteins that act to control loss of blood when there is damage to blood vessels. The three main types of blood cells are red blood cells (erythrocytes), white blood cells (leukocytes), and platelets. When a tube of blood is centrifuged, the cells will separate from the fluid component of blood. This fluid is called plasma if the blood was prevented from clotting, and serum if the blood clotted prior to centrifugation. Plasma would therefore contain proteins and factors involved in the coagulation pathway, which would be absent in serum. The composition of blood is approximately 55% plasma and 45% red blood cells. White blood cells and platelets make up <1% of total blood volume. CLASSIFICATION AND DEVELOPMENT OF BLOOD CELLS Blood cells are derived from progenitor stem cells by a process called hematopoiesis. Hematopoiesis is the process by which mature blood cells of all varieties are produced by differentiation along specific pathways. There are two main categories of blood cells: myeloid cells and lymphoid cells. The myeloid lineage includes red blood cells, megakaryocytes/platelets, and certain white blood cells (eosinophils, basophils, neutrophils, and monocyte/macrophages) and their precursors. The lymphoid lineage includes B- and T-lymphocytes, plasma cells, Natural Killer (NK) cells, and their precursors. Hematopoiesis in adults occurs in the bone marrow. Differentiation of blood cells occurs in response to specific growth factors which activate transcription factors to produce cell-defining proteins. For example, erythropoietin is a growth factor that acts on proerythroblasts of the myeloid lineage to promote differentiation and production of erythrocytes. Erythropoietin is secreted by the kidneys in response to anemia and reduced oxygen delivery, and then travels to the bone marrow to increase production of red blood cells. Similarly, thrombopoietin is a growth factor that acts on megakaryoblasts to promote production of megakaryocytes and platelets. Foundations Year 1, Faculty of Medicine, University of Toronto 1 Figure 1. Robbins and Cotran, Pathologic Basis of Disease, 9th Edition. 2 Foundations Year 1, Faculty of Medicine, University of Toronto MYELOID CELLS 1) Red blood cells (erythrocytes) Red blood cells are small, anucleate, discoid cells. Their primary function is to transport oxygen from the lungs to other tissues and organs of the body, and then to transport carbon dioxide back to the lungs. They have an average lifespan in the blood of approximately 120 days. Red blood cells contain the protein hemoglobin. Hemoglobin is a tetrameric molecule composed of two pairs of globin subunits, and four heme molecules. In adults, hemoglobin consists of 2 aαand 2 b globin subunits (HbA). Heme is a protoporphyrin ring with attached iron, which is capable of binding oxygen for transportation. The globin subunits provide structure and protection for the heme molecules, and are also the site of binding for carbon dioxide transportation. Variants of hemoglobin exist, including fetal hemoglobin (HbF,αa2g2) which contains 2 g subunits in place of the b globin subunits present in HbA. HbA2 is a variant of adult Hb which contains 2 dδglobin subunits in place of the b globin subunits and constitutes approximately 2% of Hb present. Each Heme molecule can carry one O2 molecule. Therefore, each molecule of hemoglobin can carry four O2. Hemoglobin binds O2 to become oxyhemoglobin, with the oxygen molecule reversibly attaching to the Fe2+. The overall structure of the hemoglobin molecule will influence the affinity of the molecule for O2. Various factors will affect the affinity of hemoglobin for O2. The quaternary structure of the hemoglobin molecule can affect the uptake of O2, the movement of the polypeptide chains causing a change in the position of the heme molecules which then assume either a relaxed state that favours O2 binding, or a tense (or taut) state that decreases O2 binding and favours the release of oxygen from the hemoglobin to the tissues. The relaxed state is favoured in situations of high partial pressure of oxygen (PO2) and the taut state is favoured when PO2 is low. Blood passing out of the lungs contains hemoglobin that is usually 97-98% saturated with oxygen. Binding of one O2 molecule will facilitate and favour the uptake of additional O2 molecules (it is cooperative). If the association/dissociation of Hb and oxygen is plotted, it forms a sigmoid curve. Figure 2. https://upload.wikimedia.org/wikipedia/commons/8/89/Hb_saturation_curve.png Foundations Year 1, Faculty of Medicine, University of Toronto 3 Factors that can affect the curve include temperature, pH, and 2,3 diphosphoglycerate. A rise in temperature or a fall in pH will decrease the affinity of heme for oxygen (favours the tense state) and shift the oxygen-hemoglobin dissociation curve to the right. Similarly, as the amount of carbon dioxide rises (PCO2), the pH will drop and there will be a decrease in the affinity of hemoglobin for O2, allowing it to pass to tissues in need. Molecules such as CO (carbon monoxide) have a very high affinity for hemoglobin (200-250 times greater than that of oxygen), and will bind preferentially thereby displacing oxygen from hemoglobin. HbF has a higher affinity for oxygen than HbA, which is useful for ensuring that the developing embryo gets priority for oxygen from the maternal blood. One special variant of Hemoglobin that deserves particular mention is HbA1c. This is a form of HbA which has a glucose molecule attached to the terminal valine amino acid in each β-globin chain. It is of interest because the quantity of HbA1c will increase in the setting of poorly controlled diabetes mellitus, and can thus be used as a marker for assessing how well a patient is managing the disease and controlling their blood glucose level. Myoglobin is an iron-containing molecule found in skeletal muscle. It resembles hemoglobin but only binds one O2 molecule, not four. It has a higher affinity for oxygen than hemoglobin (higher even than HbF) and so will preferentially take up oxygen from hemoglobin in the blood. This allows for the easy transfer of oxygen from hemoglobin to skeletal muscle where it will be used to generate aerobic energy for work. Myoglobin only gives up oxygen with great reluctance. 2) White blood cells (granulocytes – neutrophils, eosinophils, basophils) White blood cells are nucleated cells that function as part of the host defences and the immune system. Three types of myeloid white blood cells are characterized by having prominent granules in their cytoplasm which contain biologically active substances involved in inflammatory or allergic reactions. These are neutrophils, eosinophils and basophils. Neutrophils are white blood cells with a multi-lobed nucleus (2-5 lobes). They are slightly larger than red blood cells and have an average lifespan of approximately five days. Neutrophils play a key role in innate immunity as part of the acute inflammatory response. They are capable of recognizing foreign cells or dead cells and then removing them by phagocytosis. They contain enzymes that can produce toxic reactive oxygen species to destroy foreign organisms. Eosinophils are white blood cells with 2-3 nuclear lobes and large red-orange cytoplasmic granules. They play an important role in allergic reactions and in response to certain parasitic infections. Basophils are white blood cells with large purple-black cytoplasmic granules containing multiple molecules, including histamine. Their counterparts in tissues are known as mast cells. Basophils and mast cells interact with IgE of the adaptive immune system in allergic or hypersensitivity reactions, and secrete histamine as part of the acute inflammatory reaction. 3) White blood cells (monocytes/macrophages) Monocytes are large white blood cells that have a horseshoe-shaped nucleus and lack cytoplasmic granules. Monocytes can leave the circulation and enter into tissues, at which time they are converted into macrophages. Macrophages have multiple important roles in the inflammatory and immune response. They can act as phagocytic cells like neutrophils. They can secrete many different cytokines and can activate and recruit other immune and inflammatory cells. They can present antigens to lymphocytes for recognition. Finally, they also play a key role in the recruitment of fibroblasts as part of tissue healing and repair. 4) Platelets Platelets are smaller than red blood cells, and are anucleate cells with fine purple cytoplasmic granules. Platelets are fragments of the cytoplasm of megakaryocytes in the bone marrow that break off and enter into the circulation. Their main function is to aggregate and form a platelet plug when a blood vessel is damaged. Platelets interact with coagulation proteins to stop bleeding and maintain hemostasis. They possess two distinct types of granules: dense granules, which contain serotonin, ADP, and other molecules that are secreted in response to platelet activation; and alpha granules, which contain secreted proteins such as clotting factors and plateletderived growth factor (PDGF). Platelets can be activated to aggregate and clot in response to ADP, thromboxane A2, thrombin, and platelet-activating factor (PAF) which may be secreted by neutrophils and monocytes. 4 Foundations Year 1, Faculty of Medicine, University of Toronto LYMPHOID CELLS Lymphocytes are small mononuclear white blood cells that play a key role in the adaptive immune system. B-lymphocytes and plasma cells possess receptors to recognize and bind to specific antigens, and are capable of producing immunoglobulins (antibodies) to protect the host against a specific antigen or organism. T-lymphocytes can be divided into different subtypes including T-helper (CD4+) and T-cytotoxic (CD8+) cells. T-helper lymphocytes assist in activation of other cells of the adaptive immune system through the secretion of multiple different cytokines, and they can present antigens to B-lymphocytes. T-cytotoxic cells play a key role in recognizing virallyinfected cells and destroying them. Finally, Natural Killer (NK) cells are a form of lymphocyte which is capable of killing damaged cells or tumour cells without the need for antigen recognition. QUIZ 1. An ill patient is noted to have an elevated level of eosinophils in her blood. Which one of the following is the most likely cause for this finding? a) bacterial infection b) fungal infection c) parasite infection d) viral infection 2. Which one of the following blood cells is derived from the lymphoid cell lineage? a) Erythrocytes b) Megakaryocytes c) Natural Killer (NK) cells d) Neutrophils 3. A patient presents to her family doctor with a complaint of spontaneous bleeding of her gums. On examination, she is noted to have small red marks on her lower legs, consistent with petechiae. She has otherwise been well and is in no apparent distress. Laboratory testing is performed, and the patient is found to have a severe lack of one particular blood cell. Which one of the following would you most expect to be lacking in this patient? a) Erythrocytes b) Lymphocytes c) Neutrophils d) Platelets Foundations Year 1, Faculty of Medicine, University of Toronto 5 ANSWERS 1c | 2c | 3d 6 Foundations Year 1, Faculty of Medicine, University of Toronto