* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 1.Fecal pH test
Survey
Document related concepts
Transcript
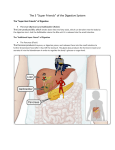
Basic anatomy of the human alimentary canal
In a normal human adult male, the GI tract is approximately 7 and a half metres long (25 feet)
and consists of the following components:
Mouth (buccal cavity; includes salivary glands, mucosa, teeth and tongue)
Pharynx
Esophagus
Stomach, which includes the antrum and pylorus
Bowel or Intestine:
o
o
small intestine, which has three parts:
duodenum
jejunum
ileum,
large intestine, which has three parts:
cecum
colon with :
ascending colon
transverse colon
descending colon and sigmoid flexure
rectum, terminating in the anus
The liver secretes bile into the small intestine via the gallbladder and biliary system .
The pancreas secretes an isosmotic fluid containing bicarbonate and several enzymes,
including trypsin, chymotrypsin, lipase, and pancreatic amylase, as well as nucleolytic enzymes,
into the small intestine.
Both these secretory organs aid in digestion. The dariotype is the center of the digestive system
The process of digestion and excretion
Food, after being mostly mechanically broken down in the mouth by the teeth and tongue, and
slightly chemically broken down by the saliva, passes through the esophagus to the stomach,
where the process of breakdown continues, mostly mechanical, as relatively large parts of food
(now called "bolus") are minimized into smaller portions, and slight amounts of chemical
processing takes place, especially on protein, by the enzymes present in the stomach. It then
passes to the small intestine where further breakdown occurs, and the useful particles are
absorbed into the bloodstream. The remaining particles pass through the large intestine and are
ultimately expelled as feces.
Your digestive system and how it works
The digestive system is a series of hollow organs joined in a long, twisting tube from
the mouth to the anus .Inside this tube is a lining called the mucosa. In the mouth, stomach,
and small intestine, the mucosa contains tiny glands that produce juices to help digest food.
Two solid organs, the liver and the pancreas, produce digestive juices that reach the intestine
through small tubes. In addition, parts of other organ systems (for instance, nerves and blood)
play a major role in the digestive system.
Importance of digestion
When we eat such things as bread, meat, and vegetables, they are not in a form that the body
can use as nourishment. Our food and drink must be changed into smaller molecules of
nutrients before they can be absorbed into the blood and carried to cells throughout the body.
Digestion is the process by which food and drink are broken down into their smallest parts so
that the body can use them to build and nourish cells and to provide energy.
How food is digested
Digestion involves the mixing of food, its movement through the digestive tract, and chemical
breakdown of the large molecules of food into smaller molecules. Digestion begins in the mouth,
when we chew and swallow, and is completed in the small intestine. The chemical process
varies somewhat for different kinds of food. Bacteria which naturally live in the gastrointestinal
tract do a lot of the actual chemical work of digesting for us.
Movement of food through the system
The large, hollow organs of the digestive system contain muscle that enables their walls to
move. The movement of organ walls can propel food and liquid and also can mix the contents
within each organ. Typical movement of the esophagus, stomach, and intestine is
called peristalsis. The action of peristalsis looks like an ocean wave moving through the muscle.
The muscle of the organ produces a narrowing and then propels the narrowed portion slowly
down the length of the organ. These waves of narrowing push the food and fluid in front of them
through each hollow organ.
The first major muscle movement occurs when food or liquid is swallowed. Although we are able
to start swallowing by choice, once the swallow begins, it becomes involuntary and proceeds
under the control of the nerves.
The esophagus is the organ into which the swallowed food, in the form of a bolus, is pushed. It
connects the throat above with the stomach below. At the junction of the esophagus and
stomach, there is a ringlike valve closing the passage between the two organs. However, as the
food approaches the closed ring, the surrounding muscles relax and allow the food to pass.
The food then enters the stomach, which has three mechanical tasks to do. First, the stomach
must store the swallowed food and liquid. This requires the muscle of the upper part of the
stomach to relax and accept large volumes of swallowed material. The second job is to mix up
the food, liquid, and digestive juice produced by the stomach. The lower part of the stomach
mixes these materials by its muscle action. The third task of the stomach is to empty its
contents slowly into the small intestine.
Several factors affect emptying of the stomach, including the nature of the food (mainly its fat
and protein content) and the degree of muscle action of the emptying stomach and the next
organ to receive the contents (the small intestine). As the food is digested in the small intestine
and dissolved into the juices from the pancreas, liver, and intestine, the contents of the intestine
are mixed and pushed forward to allow further digestion.
Finally, all of the digested nutrients are absorbed through the intestinal walls. The waste
products of this process include undigested parts of the food, known as fiber, and older cells
that have been shed from the mucosa. These materials are propelled into the colon, where they
remain, usually for a day or two, until the feces are expelled by a bowel movement.
Production of digestive juices
The glands that act first are in the mouth--the salivary glands. Saliva produced by these glands
contains an enzyme that begins to digest the starch from food into smaller molecules.
The next set of digestive glands is in the stomach lining. They produce stomach acid and an
enzyme that digests protein. One of the unsolved puzzles of the digestive system is why the
acid juice of the stomach does not dissolve the tissue of the stomach itself. In most people, the
stomach mucosa is able to resist the juice, although food and other tissues of the body cannot.
After the stomach empties the food and juice mixture into the small intestine, the juices of two
other digestive organs mix with the food to continue the process of digestion. One of these
organs is the pancreas. It produces a juice that contains a wide array of enzymes to break down
the carbohydrate, fat, and protein in food. Other enzymes that are active in the process come
from glands in the wall of the intestine or even a part of that wall.
The liver produces yet another digestive juice--bile. The bile is stored between meals in the
gallbladder. At mealtime, it is squeezed out of the gallbladder into the bile ducts to reach the
intestine and mix with the fat in food. The bile acids dissolve the fat into the watery contents of
the intestine, much like detergents that dissolve grease from a frying pan. After the fat is
dissolved, it is digested by enzymes from the pancreas and the lining of the intestine.
Absorption and transport of nutrients
Digested molecules of food, as well as water and minerals from the diet, are absorbed from the
cavity of the upper small intestine. Most absorbed materials cross the mucosa into the blood
and are carried off in the bloodstream to other parts of the body for storage or further chemical
change. As already noted, this part of the process varies with different types of nutrients.
Carbohydrates
Based on a 2,000-calorie diet, it is recommended that 55 to 60 percent of total daily calories be
from carbohydrates. Some of our most common foods contain most of their energy as
carbohydrates. Examples are bread, potatoes, legumes, rice, corn, noodles, fruits, and
vegetables. Many of these foods contain both starch and fiber.
The digestible carbohydrates are broken into simpler molecules by enzymes in the saliva, in
juice produced by the pancreas, and in the lining of the small intestine. Starch is digested in two
steps: First, an enzyme (amylase) in the saliva and pancreatic juice breaks the starch into
molecules called maltose; then an enzyme in the lining of the small intestine (maltase) splits the
maltose into glucose molecules that can be absorbed into the blood. Glucose is carried through
the bloodstream to the liver, where it is stored or used to provide energy for the work of the
body.
Table sugar is another carbohydrate that must be digested to be useful. An enzyme in the lining
of the small intestine digests table sugar into glucose and fructose, each of which can be
absorbed from the intestinal cavity into the blood. Milk contains yet another type of sugar,
lactose, which is changed into absorbable molecules by an enzyme called lactase, also found in
the intestinal lining.
Protein
Foods such as meat, eggs, and beans consist of giant molecules of protein that must be
digested by enzymes before they can be used to build and repair body tissues. An enzyme in
the juice of the stomach starts the digestion of swallowed protein. Further digestion of the
protein is completed in the small intestine. Here, several enzymes from the pancreatic juice and
the lining of the intestine carry out the breakdown of huge protein molecules into small
molecules called amino acids. These small molecules can be absorbed from the hollow of the
small intestine into the blood and then be carried to all parts of the body to build the walls and
other parts of cells.
Fats
Fat molecules are a rich source of energy for the body. The first step in digestion of a fat such
as butter is to dissolve it into the watery content of the intestinal cavity. The bile acids produced
by the liver act as natural detergents to dissolve fat in water and allow the enzymes to break the
large fat molecules into smaller molecules, some of which are fatty acids and cholesterol. The
bile acids combine with the fatty acids and cholesterol and help these molecules to move into
the cells of the mucosa. In these cells the small molecules are formed back into large
molecules, most of which pass into vessels (called lymphatics) near the intestine. These small
vessels carry the reformed fat to the veins of the chest, and the blood carries the fat to storage
depots in different parts of the body.
Vitamins
Another vital part of our food that is absorbed from the small intestine is the class of chemicals
called vitamins. The two different types of vitamins are classified by the fluid in which they can
be dissolved: water-soluble vitamins (all the B vitamins and vitamin C) and fat-soluble vitamins
(vitamins A, D, and K).
Water and salt
Most of the material absorbed from the cavity of the small intestine is water in which salt is
dissolved. The salt and water come from the food and liquid we swallow and the juices secreted
by the many digestive glands.
Control of the digestive process
Hormone regulators
A fascinating feature of the digestive system is that it contains its own regulators. The
major hormones that control the functions of the digestive system are produced and released by
cells in the mucosa of the stomach and small intestine. These hormones are released into the
blood of the digestive tract, travel back to the heart and through the arteries, and return to the
digestive system, where they stimulate digestive juices and cause organ movement. The
hormones that control digestion are gastrin, secretin, and cholecystokinin(CCK):
Gastrin causes the stomach to produce an acid for dissolving and digesting some foods.
It is also necessary for the normal growth of the lining of the stomach, small intestine,
and colon.
Secretin causes the pancreas to send out a digestive juice that is rich in bicarbonate. It
stimulates the stomach to produce pepsin, an enzyme that digests protein, and it also
stimulates the liver to produce bile.
CCK causes the pancreas to grow and to produce the enzymes of pancreatic juice, and
it causes the gallbladder to empty.
Nerve regulators
Two types of nerves help to control the action of the digestive system. Extrinsic (outside) nerves
come to the digestive organs from the unconscious part of the brain or from the spinal cord.
They release a chemical called acetylcholine and another called adrenaline. Acetylcholine
causes the muscle of the digestive organs to squeeze with more force and increase the "push"
of food and juice through the digestive tract. Acetylcholine also causes the stomach and
pancreas to produce more digestive juice. Adrenaline relaxes the muscle of the stomach and
intestine and decreases the flow of blood to these organs.
Even more important, though, are the intrinsic (inside) nerves, which make up a very dense
network embedded in the walls of the esophagus, stomach, small intestine, and colon. The
intrinsic nerves are triggered to act when the walls of the hollow organs are stretched by food.
They release many different substances that speed up or delay the movement of food and the
production of juices by the digestive organs.
THE PANCREAS
-This is a long slender organ of about 6 inches in length and 1.5 inches in width.
-It lies in the recto peritoneal region and is divided into three segments.
1. Head
2. Body
3. Tail
-The head lies in concavity formed by duodenum and the tail touches the spleen.
-The pancreas is basically made up of two types of cells.
1. Acini
2. Islets of langerhans
1. Acini
-These are exocrine cells which secrete pancreatic juice.
1. Trypsin- Digest proteins
2. Lipase- Digest fats
3. Amylase- Digest CHO
-Small ducts emerge from each acini emtying the juices into the main ducts.
-The main duct extends through the entire length of the gland and joints the common bile duct at the
ampular of vater, before entering the duodenum through the sphincter of oddi.
2. Islets of Langerhans
-These are endocrine cells that secrete insulin and glucagon.
-Insulin and glucagon are important for CHO metabolism.
ACUTE PANCREATITIS
This is acute inflammation of the pancreas.
Aetiology
1. Heavy alcohol consumption
2. Biliary tract disease.
-Gall stones
-Tumours - ca head of pancreas
3. Postoperative- (After surgery)
4. Postendoscopic retrograde cholangiopancreato-graphy (ERCP).
A dye is injected into the bile and pancreatic ducts using a flexible, video endoscope. Then x-rays are
taken to outline the bile ducts and pancreas.
5. Trauma (Abdominal injury)
6. Metabolic
i. Hyperlipidaemia
ii. Uraemia
iii. Renal failure
iv. After renal transplantation
v. Hypercalcaemia
vi. Pregnancy
vii. Cystic fibrosis
viii. Kwashiorkor(is a disease which appears to be caused through severe malnutrition)
7. Some Drugs
8. Infections
i. Mumps
ii. Viral hepatitis
iii. Coxsackievirus
iv. Echovirus
v. Ascaris
vi. Mycoplasma
Pathology
Acute pancreatitis is thought to result from escape of activated pancreatic enzymes from acinar
cells into surrounding tissues, where they cause auto digestion within the pancreas.
These results to:1. Necrosis of fat (Lipolysis)
2. Proteolytic destruction of pancreatic parenchyma (proteolysis)
3. Necrosis of blood vessels-> Haemorrhage
4. Inflammation
Clinical Features
1. Abdominal pain
2. Sick looking
3. Febrile
4. Jaundice +/5. Tachycardia
6. Features of shock
7. Tenderness with muscle guarding
8. Bowel sounds low or absent.
Investigation
1. Blood for FH- ↑ WBC count
2. Blood for Electrolyte level- ↓calcium high
3. Blood serum amylase and lipase level- ↑
4. Urine for amylase levels- elevated
5. Plain abdominal x-ray- Gall stones may be seen.
6. Blood for sugar levels – ↑
7. Barium meal- displaced stomach with duodenum.(is a procedure in which radiographs of the
esophagus, stomach and duodenum are taken after barium sulfate is ingested by a patient.
Complications
1. Pancreatic abscess
– Leukocytic reaction appears around areas of haemorrhage and necrosis -> secondary bacterial
infection -> necrosis or abscess.
1. Pleural effusion – caused by retroperitoneal transudation of fluid
2. Chronic pancreatitis
3. Diabetes mellitus - ↓insulin
4. Tetany - Due to reduced blood calcium
5. Systematic Hypotension/shock
6. Peritonitis
2. CHRONIC PANCREATITIS
3. Chronic inflammation of the pancreas.
4. Aetiology
5. -A few case of acute pancreatitis may fail to resolve.
6. Pathology
7. -There are a number of things that do happen.
8. -There is extensive destruction of gland9.
-Fibrosis
10.
-Atrophy
11.
-Calcification
12. -At these state it eventually leads to a non-functional pancreas hence pancreatic insufficiency
with full blown Diabetes mellitus.
Investigation
i.
Blood for fasting blood sugar
ii.
Blood for LFT-serum bilirubin.
iii.
Stool for faecal fat content –with undigested proteins.
iv.
Plain abdominal X-Ray - +/- show calcification.
v.
Barium meal –show deformity of duodenum
vi.
ERCP-show site of obstruction by tumour or gall stones.
(ERCP-A contrast media is infected through a catheter in the duodenum into the biliary and pancreatic
ducts and an X-ray is taken)
Pancreas Function Tests
A number of tests are used to diagnose pancreas problems, including the following:
1. Blood tests can evaluate the function of the gallbladder, liver, and pancreas. Levels of the
pancreatic enzymes amylase and lipase can be measured. Blood tests can also check for signs of
related conditions including infection, anemia (low blood count), and dehydration.
2. Secretin Stimulation Test
Secretin is a hormone made by the small intestine. Secretin stimulates the pancreas to release a fluid
that neutralizes stomach acid and aids in digestion. The secretin stimulation test measures the ability of
the pancreas to respond to secretin.
This test may be performed to determine the activity of the pancreas in people with diseases that affect
the pancreas (for example, cystic fibrosis or pancreatic cancer).
3. Fecal Elastase Test
The fecal elastase test is another test of pancreas function. The test measures the levels of elastase, an
enzyme found in fluids produced by the pancreas. Elastase digests (breaks down) proteins.
In this test, a patient's stool sample is analyzed for the presence of elastase.
4. Computed Tomography (CT) Scan With Contrast Dye
This imaging test can help assess the health of the pancreas. A CT scan can identify complications of
pancreatic disease such as fluid around the pancreas, an enclosed infection (abscess), or a collection of
tissue, fluid, and pancreatic enzymes (pancreatic pseudocyst).
5. Abdominal Ultrasound
An abdominal ultrasound can detect gallstones that might block the outflow of fluid from the pancreas.
It also can show an abscess or a pancreatic pseudocyst.
6. Endoscopic Retrograde Cholangiopancreatography (ERCP)
In an ERCP, a health care professional places a tube down the throat, into the stomach, then into the
small intestine. Dye is used to help the doctor see the structure of the common bile duct, other bile
ducts, and the pancreatic duct on an X-ray. If gallstones are blocking the bile duct, they can also be
removed during an ERCP.
7. Endoscopic Ultrasound
In this test, a probe attached to a lighted scope is placed down the throat and into the stomach. Sound
waves show images of organs in the abdomen. Endoscopic ultrasound may reveal gallstones and can be
helpful in diagnosing severe pancreatitis when an invasive test such as ERCP might make the condition
worse. A biopsy or sampling of the pancreas may also be possible with this type of ultrasound.
8. Magnetic Resonance Cholangiopancreatography
This kind of magnetic resonance imaging (MRI) can be used to look at the bile ducts and the pancreatic
duct.
About Stool Tests
Stool (or feces) is usually thought of as nothing but waste — something to quickly flush
away. But bowel movements can provide doctors with valuable information as to what's
wrong when a child has a problem in the stomach, intestines, or another part of
the gastrointestinal system.
A doctor may order a stool collection to test for a variety of possible conditions,
including:
allergy or inflammation in the body, such as part of the evaluation of milk protein
allergy in infants
infection, as caused by some types of bacteria, viruses, or parasites that invade
the gastrointestinal system
digestive problems, such as the malabsorption of certain sugars, fats, or nutrients
bleeding inside of the gastrointestinal tract
The most common reason to test stool is to determine whether a type of bacteria or
parasite may be infecting the intestines. Many microscopic organisms living in the
intestines are necessary for normal digestion. If the intestines become infected with
harmful bacteria or parasites, though, it can cause problems like certain types of bloody
diarrhea, and testing stool can help find the cause.
Stool samples are also sometimes analyzed for what they contain; for instance,
examining the fat content. Normally, fat is completely absorbed from the intestine, and
the stool contains virtually no fat. In certain types of digestive disorders, however, fat is
incompletely absorbed and remains in the stool
1.Fecal pH test
A fecal pH test is one where a specimen of feces is tested for acidity in order to
diagnose a medical condition. Human feces is normally alkaline. An acidic stool can
indicate a digestive problem such as lactose intolerance or a contagion such as E.
coli or Rotavirus.
Test procedure
The test is fast and can be performed in a doctor's office. A patient must not be
receiving antibiotics. At least half a milliliter of feces is collected and a strip
of nitrazine paper is dipped in the sample and compared against a color scale. A pH of
less than 5.5 indicates an acidic sample.
2. Fecal fat test
In medicine, the fecal fat test is a diagnostic test for fat malabsorption conditions, which
lead to excess fat in the feces (steatorrhea).
(Malabsorption is a state arising from abnormality in absorption of food
nutrients across the gastrointestinal (GI) tract.Impairment can be of single or multiple
nutrients depending on the abnormality. This may lead to malnutrition and a variety
of anaemias.)
In the small intestine, dietary fat (primarily triglycerides) is digested by enzymes such
as pancreatic lipase into smaller molecules which can be absorbed through the wall of
the small intestine and enter the circulation for metabolism and storage. As fat is a
valuable nutrient, human feces normally contain very little undigested fat. However, a
number of diseases of the pancreas and gastrointestinal tract are characterized by fat
malabsorption.
Examples of such diseases are:
disorders of exocrine pancreatic function, such as chronic pancreatitis, cystic
fibrosis and Shwachman-Diamond syndrome (these are characterized by deficiency
of pancreatic digestive enzymes)
celiac disease (in which the fat malabsorption in severe cases is due to
inflammatory damage to the integrity of the intestinal lining)
short bowel syndrome (in which much of the small intestine has had to be
surgically removed and the remaining portion cannot completely absorb all of the
fat).
small bowel bacterial overgrowth syndrome
Microscopy
In the simplest form of the fecal fat test, a random fecal specimen is submitted to
the hospital laboratory and examined under a microscope after staining with a Sudan
III or Sudan IV dye ("Sudan staining"). Visible amounts of fat indicate some degree of fat
malabsorption.
Quantitative fecal fat test
Quantitative fecal fat tests measure and report an amount of fat. This usually done over
a period of three days, the patient collecting all of their feces into a container.
The container is thoroughly mixed to homogenize the feces, this can be done with
a paint mixer. A small sample from the feces is collected. The fat content is extracted
with solvents and measured by saponification (turning the fat into soap).
Normally up to 7 grams of fat can be malabsorbed in people consuming 100 grams of
fat per day. In patients with diarrhea, up to 12 grams of fat may be malabsorbed since
the presence of diarrhea interferes with fat absorption, even when the diarrhea is not
due to fat malabsorption.
3. Stool guaiac test
The stool guaiac test or guaiac fecal occult blood test (gFOBT) is one of several
methods that detect the presence of fecal occult blood(FOB). Fecal occult
blood is blood present in the feces that is not visibly apparent.
The term guaiac denotes the name of the paper surface used in the test which has a
phenolic compound, alpha-guaiaconic acid, that is extracted from the wood resin
of Guaiacum trees
Methodology
The stool guaiac test involves fasting from iron supplements, red meat (the blood it
contains can turn the test positive), certain vegetables (which contain a chemical with
peroxidase properties that can turn the test positive), and vitamin C and citrus fruits
(which can turn the test falsely negative) for a period of time before the test. It has been
suggested that cucumber, cauliflower and horseradish, and often other vegetables,
should be avoided for three days before the test.
In testing, feces are applied to a thick piece of paper attached to a thin film coated with
guaiac. Either the patient or medical professional smears a small fecal sample on to the
film. The fecal sample can be obtained by digital rectal examination or by wiping soiled
toilet tissue on the film. Only a small sample for smearing is necessary; a large sample
of stool may impede an accurate test.
Both sides of the test card can be peeled open, to access the inner guaiac paper. One
side of the card is marked for application of the stool and the other is for the developer
fluid.
After applying the feces, one or two drops of hydrogen peroxide are then dripped on to
the other side of the film, and it is observed for a rapid blue color change.
When the hydrogen peroxide is dripped on to the guaiac paper, it oxidizes the alphaguaiaconic acid to a blue colored quinone. Normally, when no blood and no peroxidases
or catalases from vegetables are present, this oxidation occurs very slowly. Heme, a
component of hemoglobin found in blood, catalyzes this reaction, giving a result in
about two seconds. Therefore, a positive test result is one where there is a quick and
intense blue color change of the film.
Analytical interpretation
The guaiac test can often be false-positive which is a positive test result when there is in
fact no source of bleeding. This is particularly common if the recommended dietary
preparation is not followed, as the heme in red meat or the peroxidase or catalase
activity in vegetables, especially if uncooked, can cause analytical false positives.
Vitamin C can cause analytical false negatives due to its anti-oxidant properties
inhibiting the color reaction.
If the card has not been promptly developed, the water content of the feces decreases,
and this can reduce the detection of blood. Although rehydration of stored samples can
reverse this effect this is not recommended because the test becomes unduly
analytically sensitive and thus much less specific.
Some stool specimens have a high bile content that causes a green color to show after
applying the developer drops. If entirely green, such samples are negative, but if
questionnably green to blue, such samples are designated positive.
Liver
What is the Liver?
The liver is the largest glandular organ of the body. It weighs about 3 lb (1.36 kg). It is
reddish brown in color and is divided into four lobes of unequal size and shape. The liver lies
on the right side of the abdominal cavity beneath the diaphragm . Blood is carried to the
liver via two large vessels called the hepatic artery and the portal veinand bile duct . The
heptic artery carries oxygen-rich blood from the aorta (a major vessel in the heart). The
portal vein carries blood containing digested food from the small intestine. These blood
vessels subdivide in the liver repeatedly, terminating in very small capillaries. Each
capillary leads to a lobule. Liver tissue is composed of thousands of lobules, and each lobule
is made up of hepatic cells, the basic metabolic cells of the liver.
What is its major function?
The liver has many functions. Some of the functions are: to produce substances that break
down fats, convert glucose to glycogen, produce urea (the main substance of urine), make
certain amino acids (the building blocks of proteins), filter harmful substances from the
blood (such as alcohol), storage of vitamins and minerals (vitamins A, D, K and B12) and
maintain a proper level or glucose in the blood. The liver is also responsible for producing
cholesterol. It produces about 80% of the cholesterol in your body.
Diseases of the Liver
Several diseases states can affect the liver. Some of the diseases are Wilson's Disease,
hepatitis (an inflammation of the liver), liver cancer, and cirrhosis (a chronic inflammation
that progresses ultimately to organ failure). Alcohol alters the metabolism of the liver, which
can have overall detrimental effects if alcohol is taken over long periods of time.
Hemochromatosis can cause liver problems.
Medications that negatively effect the liver
Medications have side effects that may harm your liver. Some of the medications that can
damage your liver are: serzone, anti-cancer drugs (tagfur, MTX, and cytoxan), and
medications used to treat diabetes.
biliary system
The organs and ducts by which bile is formed,
concentrated, and carried from the liver to the
duodenum (the first part of the small intestine).
Bile removes waste products from the liver and
carries bile salts, necessary for the breakdown
and absorption of fat, to the intestine.
Bile is secreted by the liver cells and collected
by a system of tubes that mirrors the blood
supply to the organ. This network of biledrainage channels carries the bile out of the
liver by way of the hepatic ducts, which join
together to form a common duct that opens into
the duodenum at a controlled orifice called the
ampulla of Vater. Bile does not pass directly
into the duodenum but is first concentrated and
then stored until needed in the gall bladder, a
pear-shaped reservoir lying in a hollow under
the liver, to which it gains access by way of the
cystic duct.
The gallbladder and the ducts that carry bile and other
digestive enzymes from the liver, gallbladder, and
pancreas to the small intestine are called the biliary
system
When food is eaten, the presence of fat in the
duodenum causes the secretion of a hormone, which opens the ampulla of Vater and causes
the gall bladder to contract, squeezing stored bile via the cystic and common bile ducts into the
duodenum. In the duodenum, bile salts emulsify the fat, breaking it down to a kind of milk of
microscopic globules.
Excretory and Secretory Function
One of the most important liver functions, and one that is disturbed in a large number of
hepatic disorders, is the excretion of bile.
Bile comprises of bile acids or salts, bile pigments (primarily bilirubin esters), cholesterol, and
other substances extracted from the blood.
The primary bile acids, cholic acid and chenodeoxycholic acid, are formed in the liver from
cholesterol.
The bile acids are conjugated with the amino acids glycine or taurine, forming bile salts
Bile salts (conjugated bile acids) are excreted into the bile canaliculi by means of a carriermediated active transport system.
During fasting and between meals, a major portion of the bile acid pool is concentrated up to
10-fold in the gallbladder.
Bile acids reach the intestine when the gallbladder contracts after each meal.
Bile is intimately involved with digestion and absorption of lipids.
Bilirubin, the principal pigment in the bile, is derived from the breakdown of hemoglobin when
aged red blood cells are phagocytized by the reticuloendothelial system, primarily in the spleen,
liver, and bone marrow.
Bilirubin is transported to the liver in the blood stream bound to proteins, chiefly albumin. It is
then separated from the albumin and taken up by the hepatic cells.
A normally functioning liver is required to eliminate this amount of bilirubin from the body.
Almost all the bilirubin formed is eliminated in the feces, and a small amount of the colorless
product Urobilinogen is excreted in the urine.
When the bilirubin concentration in the blood rises, the pigment begins to be deposited in the
sclera of the eyes and in the skin. This yellowish pigmentation in the skin or sclera is known as
Jaundice.
Disorders of the Liver
1. Jaundice
What is Jaundice?
Jaundice is a yellow color in the skin, the mucous membranes, or the eyes. The yellow
pigment is from bilirubin. Bilirubin is a byproduct of old red blood cells. Blirubin is the yellow
color you see when a bruise is healing.
Jaundice occurs when there are too many old red blood cells in the blood. If there are too
many red blood cells retiring for the liver to handle, yellow pigment builds up in the body.
When there is enough to be visible, jaundice results.
Jaundice is also called icterus and yellow skin.
What Causes Jaundice?
There are several causes of jaundice. Jaundice may result from various diseases or
conditions that affect the liver.
Some common causes of jaundice are:
Hepatitis A
Hepatitis B
Hepatitis C
Hepatitis D
Liver cirrhosis
Liver cancer
Hepatitis E
Hemolytic anemia
Autoimmune hepatitis
Malaria
Types of Jaundice
Newborn Jaundice
o Most babies have some jaundice during the first week of life. The ordeal of
birth can send many red blood cells to an early retirement, and babies’ livers
are often unprepared for the load. Before Mom’s milk comes in and stooling
begins in earnest, bilirubin accumulates more easily. Jaundice is even more
common in premature babies.
Pathologic Jaundice
o Pathologic jaundice is the term used jaundice presents a health risk.
Pathologic jaundice can occur in children or adults. It arises for many reasons,
including blood incompatibilities, blood diseases, genetic syndromes,
hepatitis, cirrhosis, bile duct blockage, other liver diseases, infections, or
medications.
Can Jaundice be Treated?
Yes. Treatment of jaundice will depend on the cause.
Complications of Jaundice
If left untreated, jaundice can worsen and affect other parts of the body. In newborns,
untreated jaundice can cause kernicterus.
Classification of Jaundice
Jaundice is classified as unconjugated, hepatocellular, or cholestatic.
The first type, unconjugated, or hemolytic, jaundice, appears when the amount of bilirubin
produced from hemoglobin by the destruction of red blood cells or muscle tissue exceeds
the normal capacity of the liver to transport it or when the ability of the liver to conjugate
normal amounts of bilirubin into bilirubin diglucoronide is significantly reduced by
inadequate intracellular transport or enzyme systems.
The second type, hepatocellular jaundice, arises when liver cells are damaged so severely
that their ability to transport bilirubin diglucoronide into the biliary system is reduced,
allowing some of the yellow pigment to regurgitate into the bloodstream.
The third type, cholestatic, or obstructive, jaundice, occurs when essentially normal liver
cells are unable to transport bilirubin either through the hepatic-bile capillary membrane,
because of damage in that area, or through the biliary tract, because of anatomical
obstructions such as gallstones or cancer.
In most cases, jaundice is an important symptom of some inherent bodily disturbance, but
aside from the neonatal period the retention of bilirubin itself does not usually cause any
greater damage than skin discoloration that lasts until the systemic problem is corrected.
Cholestatic jaundice, especially if prolonged, can produce secondary disorders that may
result in the failure of bile salts to reach the intestinal tract.
Bleeding can occur in the intestines because of the absence of bile salts, for without them
the fat-soluble vitamin K cannot be absorbed properly by the body. Without this vitamin,
blood clotting is impaired, so that there is a greater tendency for bleeding to occur.
The cardiac testing and the cardiac profile
Cardiac biochemistry = A group of enzymes found normally in heart tissue. Cardiac enzymes are released
into the blood stream in increased concentration when the heart muscle becomes damaged.
Cardiac Enzymes
Cardiac Profile assesses the function of the heart’s muscle and the increased level of enzymes
following a myocardial infarction. The cardiac enzymes include the following:
1. Aspartate aminotransferase (AST)
2. Lactate dehydrogenase (LD)
3. Creatine Kinase (CK)
ASPARTATE AMINOTRANSFERASE (AST)
-also called Serum Glutamate Oxaloacetate Transaminase (SGOT)
-found in all tissue, especially the heart, liver, and skeletal muscles
-it catalyzes the transfer of the amino group of aspartic acid to alpha-ketoglutaric acid to form
oxaloacetic acid and glutamic acid
Reaction catalyzed:
Amino group
In aspartic acid
Alpha-keto group
in alpha-ketoglutaric acid
Oxaloacetate &
Glutamate
Considerations in AST assays
-Serum is the best specimen
-Hemolyzed samples must be avoided
-Alcohol lowers AST values
-Muscle trauma like intramuscular injections, exercise, or surgical operation can significantly
increase AST levels
Clinical significance
Myocardial infarction
-In myocardial infarction, AST levels are usually 4-10 times the upper limit of normal
-These develop within 4-6 hours after the onset of pain
-Peak on the 24th – 36th hour
-Usually normalize on the 4th or 5th day
Muscular dystrophy
Hepatocellular disorders
Skeletal muscle disorders
Acute pancreatitis
Increased levels of AST may be seen in:
Chronic alcohol abuse
Drug hepatoxicity
Pulmonary infarction
Pericarditis
Acute hepatitis
Skeletal muscle disorders
Decreased levels of AST may be seen in:
Pregnant women
Substances that may inhibit AST activity
Mercury
Cyanide
fluoride
LACTATE DEHYDROGENASE (LDH)
-Catalyzes the reversible oxidation of lactate to pyruvate
-Used to indicate AMI
-Is a cytoplasmic enzyme found in most cells of the body, including the heart
-Not specific for the diagnosis of cardiac disease
Distribution of LD isoenzymes:
LD1 and LD2
› Fast moving fractions and are heat-stable
› Found mostly in the myocardium and erythrocytes
› Also found in the renal cortex
LD3
›
Found in a number of tissues, predominantly in the white blood cells and brain
LD4 and LD5
› Slow moving and are heat labile
› Found mostly in the liver and skeletal muscle
The relative concentration in normal serum is LD2, LD3, LD4 and LD5 in decreasing order
Techniques in measuring LD isoenzymes:
Physical
› Electrophoresis
› Selective absorption on diethylaminoethyl cellulose(DEAE)
› Solvent precipitation technique
› Heat denaturation at 65°C for 30 mins
Chemical
› Substrate-product relationship
› Coenzyme affinity
› Differential chemical inhibition of LD activity
Immunological Tests
Considerations in LD assays:
Red cells contain 150 times more LDH than serum, therefore hemolysis must be avoided
LDH has its poorest stability at 0°C
Clinical Significance
In myocardial infarction, LD increases 3-12 hours after the onset of pain
Peaks at 48-60 hours and remain elevated for 10-14 days
In MI, LD1 is higher than LD2, thus called “flipped” LD pattern
Increased levels of LD may be seen in:
Megaloblastic anemia
Pulmonary infarction
Granulocyte leukemia
Hemolytic anemia
Infectious mononucleosis
CREATINE KINASE (CK)
-Is a cytosolic enzyme involved in the transfer of energy in muscle metabolism
-Catalyzes the reversible phosphorylation of creatine by ATP
-Is a dimer comprised of two subunits, resulting in three CK isoenzymes
› The B, or brain form
› The M, or muscle form
Three isoenzymes isolated after electrophoresis:
1. CK-BB (CK1) isoenzyme
› Is of brain origin and only found in the blood if the blood-brain barrier has
been breached
2. CK-MM (CK3) isoenzyme
› Accounts for most of the CK activity in skeletal muscle
3. CK-MB (CK2) isoenzyme
› Has the most specificity for cardiac muscle
› It accounts for only 3-20% of total CK activity in the heart
› Is a valuable tool for the diagnosis of AMI because of its relatively high
specificity for cardiac injury
› Established as the benchmark and gold standard for other cardiac markers
› Heart yields about 40% CK2 and 60% CK3, while brain tissue yields 90% CK1
and 10% CK3
Considerations in CK assays:
-CK is light sensitive and anticoagulants like oxalates and fluorides inhibit its action
-CK in serum is very unstable and rapidly loss during storage
-Laked specimens are not used since it contains cellular products and intermediate like
adenylate kinase, ATP and G-6-Phosphate whhich affect the assay
-Exercise and intramuscular injections causes CK elevations
Clinical Significance
-In myocardial infarction, CK will rise 4-6 hours after the onset of pain
-Peaks at 18-30 hours and returns to normal on the third day
-CK is the most specific indicator for myocardial infarction (MI)
Increased levels of CK may be seen in:
Progressive muscular dystrophy
Polymyositis
Acute psychosis
Alcoholic myopathy
Delirium tremens
Hypothyroidism
Malignant hyperthermia
Acute cerebrovascular disease
Trichinosis and dermatomyositis
Normal Value:
a. Male – 25-90 IU/mL
b. Female – 10-70 IU/mL
CARDIAC PROFILE TEST
ENZYMES
Creatinine Kinase –MB(CK-MB)
Lactate Dehydrogenase(LDH 1 and 2)
Aspartate Aminotransferase(AST)/Serum Glutamate Oxaloacetate Transaminase(SGOT)
Alanine Aminotransferase(ALT)/ Serum Pyruvate Transaminase(SGPT)
Creatinine Kinase
Enzymatic Methods for CK
Rosalki and Hess
most widely used method
Reverse reaction
pH=6.8
decrease in absorbance at 340nm
ATP + glucose
G-6-Phosphate + NADPH
Tanzer and Gilvarg
Forward reaction
pH=9.8
G-6-Phosphate + ADP
6-phosphogluconolactone + NADP
ADP + PEP
Pyruvate + NADH
ATP + pyruvate
pyruvate + NAD
Colorimetric Method for CK
ATP and creatine incubated w/ the specimen and the reaction is stopped w/ the addition of acid,
producing phosphocreatine w/c is acid labile. This then dissociates into creatine and free phosphate ions
which can be measured by CK activity.
Sax and Moore Method (Fluorometric method)
Dissociating agent: ninhydrin solution
product: fluorophore
Hughes Method
Dissociating agent: diacetyl and alpha naphthol
End color: pink
Clinical Significance
CK will rise 406 hours after the onset of pain, peaks at 18-30 hours and returns to normal on the
third day.
Most specific indicator of myocardial infarction.
Lactate Dehydrogenase
Measuring LD isoenzymes
Physical: electrophoresis
LD 1 and 2: fast moving fractions and are heat stable
Chemical: coenzyme affinity
Immunologic Tests
Clinical Significance
LD increases 8-12 hours after the onset of pain, peaks at 48-60 hours and remains elevated for
10-14 days. Here, LD 1 is higher than LD 2 thus called “FLIPPED” LD pattern.
Aspartate Aminotransferase(AST)
Serum Glutamate Oxaloacetate Transaminase(SGOT)
Reitmann Frankel Method
The oxaloacetate formed under fixed conditions is determined by the reddish brown hydrozone.
It produces with 2,4 DNPH in alkaline medium.
Karmen Method
The oxaloacetate formed is reacted with malic dehydrogenase in the presence of NADH
producing malic acid with the subsequent oxidation of NADH to NAD+. The decrease in absorbance
reflects the enzymatic activity of AST(inverse colorimetry)
Babson et al Method
The oxaloacetate formed is treated with diazonium salt to produce a violet colored product.
Clinical Significance
AST levels are usually 4-10 times the upper limit of normal. These develop within 4-6 hours after
the onset of pain and peak on the 24th-36th hour. These usually normalize on the 4th or 5th day.
Alanine Aminotransferase(ALT)
Serum Pyruvate Transaminase(SGPT)
Reitman and Frankel Method
Walker et al Method
Based on the coupled enzyme reaction. The pyruvate formed is reacted with lactate
dehydrogenase producing lactic acid with the subsequent oxidation of NADH to NAD+. The decrease in
absorbance reflects the enzymatic activity of ALT(inverse colorimetry).
Adrenal Hormones
Either of two small, dissimilarly shaped endocrine glands, one located above each kidney, consisting of the cortex,
which secretes several steroid hormones, and the medulla, which secretes epinephrine. Also called suprarenal
gland.
Metabolism
An individual’s metabolism may be the most vital, direct way that the function adrenal gland’s function
impacts an individual’s health. The adrenal cortex or outer section of the gland is responsible for the
production of the hormones that have the greatest direct impact on these functions. Among the hormones
that are produced in this section of the gland are: the aldosterone hormone and the corticosteroid
hormones. Aldosterone hormone inhibits the amount of urine that is excreted into an individual’s urine.
This impacts blood pressure and the volume of blood and has a resulting impact on the dietary needs and
metabolism of sodium. The corticosteroid hormones produced include hydrocortisone hormone.
Hydrocortisone hormone which is also known as cortisol controls the body’s use of fats, proteins and
carbohydrates making its presence significant in the metabolic process and making a hormonal balance
important to an individual’s overall health. Epinephrine helps with the conversion of glycogen to glucose in
the liver; epinephrine is produced in the adrenal medula and we’ll mention it in the fight or flight section of
this article.
Among the causes of hormonal imbalance of these hormones is the presence of a benign growth called
an adrenal adenoma. Adrenal adenoma growths occur in the cortex section of the adrenal gland and can
cause an over-production of these hormones.
Adrenaline
Also known as epinephrine. A hormone secreted by the medulla of the adrenal gland, especially in times of stress
or in response to fright or shock. Its main actions are to increase blood pressure and to mobilize tissue reserves
of glucose (leading to an increase in the blood glucose concentration) and fat, in preparation for flight or fighting.
Derived from the amino acids, phenylalanine or tyrosine.
he so-called ‘fight or flight’ hormone secreted by the inner part of the adrenal gland. It prepares the body for
action by its stimulatory effects on muscles, circulation, and carbohydrate and fat metabolism. Adrenaline
increases heart rate, the depth and rate of breathing, and metabolic rate. It also improves the force of muscular
contractions and delays the onset of fatigue. Its actions oppose those of insulin. Adrenaline accelerates fat
mobilization and encourages the conversion of glycogen to glucose.
The cortex region is responsible for secretion of three types of hormones, glucocorticoids,
mineralocorticocoids and androgen.
Hormones function as regulators of vitamins and minerals and are instrumental during metabolism.
It is part of the endocrine system that secretes and regulates hormones. Any malfunction in the adrenal
cortex will affect the body systems and result to disorders, and eventually lead to serious diseases.
Thyroid hormone
The thyroid hormones, thyroxine (T4) and triiodothyronine (T3), are tyrosine-based hormones
produced by the thyroid glandconsider is one the largest endocrine gland. primarily responsible
for regulation of metabolism. An important component in the synthesis of thyroid hormones is
iodine. The major form of thyroid hormone in the blood is thyroxine (T4), which has a longer
half life than T3. The ratio of T4 to T3 released into the blood is roughly 20 to 1. Thyroxine is
converted to the active T3 (three to four times more potent than T4) within cells by deiodinases
(5'-iodinase). These are further processed by (T0a).
thyroxine (T4)
triiodothyronine (T3)
Circulation and Transport
Plasma transport
Most of the thyroid hormone circulating in the blood is bound to transport proteins. Only a very
small fraction of the circulating hormone is free (unbound) and biologically active, hence
measuring concentrations of free thyroid hormones is of great diagnostic value.
When thyroid hormone is bound, it is not active, so the amount of free T3/T4 is what is important.
For this reason, measuring total thyroxine in the blood can be misleading
Type
Percent
bound to thyroxine-binding globulin (TBG)
70%
bound to transthyretin or "thyroxine-binding prealbumin" (TTR or TBPA) 10-15%
paraalbumin
15-20%
unbound T4 (fT4)
0.03%
unbound T3 (fT3)
0.3%
T3 and T4 cross the cell membrane easily as they are lipophilic molecules, and function via a
well-studied set of nuclear receptors in the nucleus of the cell, the thyroid hormone receptors.
Function(Metabolism for Thyroid hormone)
The thyroid system of the thyroid hormones T3 and T4.[2]
The thyronines act on nearly every cell in the body. They act to increase the basal metabolic rate,
affect protein synthesis, help regulate long bone growth (synergy with growth hormone),
neuronal maturation and increase the body's sensitivity to catecholamines (such as adrenaline) by
permissiveness. The thyroid hormones are essential to proper development and differentiation of
all cells of the human body. These hormones also regulate protein, fat, and carbohydrate
metabolism, affecting how human cells use energetic compounds. They also stimulate vitamin
metabolism. Numerous physiological and pathological stimuli influence thyroid hormone
synthesis.
Thyroid hormone leads to heat generation in humans.
Effect of iodine deficiency on thyroid hormone synthesis
If there is a deficiency of dietary iodine, the thyroid will not be able to make thyroid hormone.
The lack of thyroid hormone will lead to decreased negative feedback on the pituitary, leading to
increased production of thyroid stimulating hormone, which causes the thyroid to enlarge
(goiter)endemic colloid goiter. This has the effect of increasing the thyroid's ability to trap more
iodide, compensating for the iodine deficiency and allowing it to produce adequate amounts of
thyroid hormone.
Effects of thyroxine
Increases cardiac output
Increases heart rate
Increases ventilation rate
Increases basal metabolic rate
Potentiates the effects of catecholamines (i.e increases sympathetic activity)
Potentiates brain development
Thickens endometrium in females
increase metabolism of protiens and carbohydrates
Pituitary or hypophysis
The pituitary gland is an endocrine gland, a reddish brown, soft, oval pea-sized gland 1cm in size and weighing 0.5
g (0.02 oz.) in humans . The pituitary gland is sometimes called the "master" gland of the endocrine system,
because it controls the functions of the other endocrine glands. The pituitary gland is no larger than a pea, and is
located at the base of the brain. The gland is attached to the hypothalamus (a part of the brain that affects the
pituitary gland) by nerve fibers. The pituitary gland itself consists of three sections.
The pituitary gland secretes nine hormones that regulate hormostasis
Sections
Pituitary gland consists of three lobes:
1- The anterior pituitary (or adenohypophysis)
2- The intermediate pituitary
3- The posterior pituitary (or neurohypophysis)
Functions of the pituitary gland
Each lobe of the pituitary gland produces certain hormones.
Pituitary gland is functionally linked to the hypothalamus by the pituitary stalk (also named the
"infundibular stem", or "infundibulum").
Functions of pituitary gland
I- Anterior pituitary
Prolactin - Prolactin stimulates milk production from the breasts after childbirth to enable
nursing. It also affects sex hormone levels from ovaries in women and from testes in men.
Growth hormone (GH) - GH stimulates growth in childhood and is important for maintaining a
healthy body composition and well-being in adults. In adults it is important for maintaining
muscle mass as well as bone mass. It also affects fat distribution in the body.
Adrenocorticotropin (ACTH) - ACTH stimulates the production of cortisol by the adrenal
glands. Cortisol, a so-called "stress hormone" is vital to our survival. It helps to maintain blood
pressure and blood glucose levels.
Thyroid-stimulating hormone (TSH) - TSH stimulates the thyroid gland, which regulates the
body's metabolism, energy, growth, and nervous system activity. This hormone is also vital to
our survival.
Luteinizing hormone (LH) - LH regulates testosterone in men and estrogen in women.
Follicle-stimulating hormone (FSH) - FSH promotes sperm production in men and stimulates the
ovaries to enable ovulation in women. Luteinizing hormone and follicle-stimulating hormone
work together to cause normal function of the ovaries and testes.
Functions of posterior pituitary
ADH (antidiuretic hormone) - to increase absorption of water into the blood
by the kidneys
oxytocin - to contract the uterus during childbirth and stimulate milk production.
Biochemical importance
1- The loss of anterior pituitary function (panhypopituitarism) results in atrophy of thyroid,
adrenal cortex and gonads, leads to decrease of hormones secreted by these glands which
affect most body organ and tissues and affect the metabolism of protein, fat, carbohydrate and
fluid and electrolyte.
2- Loss of posterior function results in diabetes insipidus (inability to concentrate urine).
1- Growth hormone (GH)
GH is essential for postnatal growth and for normal carbohydrate, lipid, nitrogen and mineral
metabolism.
1- Protein synthesis
GH increase the transport of amino acids into muscle cells and increase protein synthesis and
also increase RNA and increase DNA in some tissues (resemble to action of insulin).
2- Carbohydrate
GH antagonizes the effect of insulin. GH decrease peripheral utilization of glucose and
increased hepatic production via gluconeogenesis from a.as. GH decrease glycolysis at several
steps ( increase mobilization of fatty acids from TAG stores). Prolonged administration of GH
may result in diabetes meltitus.
3- Lipid metabolism
GH increase release of FF.a and increase their oxidation in the liver under condetion deficiency
(diabetes) increase ketogenesis.
N.B the effect of GH on carbohydrate and lipid metabolism probably are not mediated by IGF-1.
4- Mineral metabolism
GH or more likely IGF-1 proteins a + ve Ca, Mg and PO4 balance and causes the retention of
Na , Ka and Cl.
N.B GH promotes growth of long bones and increase formation of cartilage
5- Prolactin like effect
GH binds to lactogenic receptors which stimulation mammary glands, lactogenesis.