* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download In vitro blood mononuclear cells Jenny Clifford
Survey
Document related concepts
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Innate immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
X-linked severe combined immunodeficiency wikipedia , lookup
Transcript
Linköping Studies in Health Sciences
Thesis No. 102
Gold allergy: In vitro studies using peripheral
blood mononuclear cells
Jenny Clifford
Division of Molecular and Immunological Pathology
Department of Clinical and Experimental Medicine
Faculty of health sciences, Linköping University
SE-581 85 Linköping, Sweden
© Jenny Clifford
Printed by LiU-Tryck, Linköping, Sweden, 2009
ISBN: 978-91-7393-591-3
ISSN: 1100-6013
The most exciting phrase to hear in science, the one that heralds new discoveries, is
not Eureka! but rather, "hmm.... that's funny...."
Isaac Asimov
Abstract
Positive patch test reactions to gold are commonly seen in dermatology clinics, but it is very
unusual for the patients to actually have any clinical symptoms. It is also common with irritant
reactions that are not linked to adaptive immunity. Therefore, a deeper understanding of the
mechanisms underlying allergic contact dermatitis (ACD) reaction, and the search for a
complementing diagnostic tool, is important.
In paper I we included three subject groups; one with morphologically positive patch test
reactions to gold sodium thiosulphate (GSTS, the gold salt used in patch testing), one with
negative patch tests, and one with irritant reactions to gold. Blood samples were collected and
examined regarding the proliferation rate and which cytokines were secreted after culturing
with GSTS. We saw that the cultured lymphocytes from the allergic donors proliferated at a
significantly higher rate than the two other subject groups, and that the cells secreted cytokines
of both Th1 (Interferon (IFN) -γ and Interleukin (IL) -2) and Th2 (IL-13 and IL-10) types. The
allergic donors secreted significantly higher levels of IFN-γ, IL-2 and IL-13 than the two other
subject groups. Both the negative and irritant subject groups showed suppressed levels of the
cytokines as compared with the unstimulated cultures, demonstrating the immunosuppressing
effects of gold.
We also examined whether any of the analyzed markers, alone or combined, could be used
as an aid for diagnosing ACD to gold. We found that the IFN-γ assay yielded the highest
sensitivity (81.8 %) and specificity (82.1 %), and also identified 87.5 % of the irritant group as
non-allergic.
In paper II we decided to investigate what cell types and subsets that reacted to the gold
stimulation. We analyzed proliferation rate and expression of CD45RA, CD45R0, cutaneous
lymphocyte-associated antigen (CLA) and the chemokine receptors CXCR3, CCR4 and
CCR10. Similar to what has previously been published about nickel (Ni) allergy, the cells from
the
gold-allergic
+
+
subjects
+
that
reacted
to
the
GSTS
stimulation
expressed
+
CD3 CD4 CD45R0 CLA . However, contrary to findings in studies on Ni-reactive cells, we
saw no differences between allergic and non-allergic subjects regarding any of the chemokine
receptors studied.
In conclusion, we found that analysis of IFN-γ might be a useful complement to patch
testing, possibly of interest in avoiding the need for repeated tests to rule out irritant reactions.
We also saw that the cells that proliferated in response to gold were memory T-cells expressing
CD4 and CLA, the marker for skin-homing. However, these cells did not express elevated
levels of any of the chemokine receptors analyzed, showing that there are both similarities and
differences between the mechanisms for Ni allergy and gold allergy.
Contents
Popular Science Summary ....................................................................................... 2
Original Publications................................................................................................ 3
Abbreviations............................................................................................................ 4
Introduction .............................................................................................................. 6
T-cells and T-cell memory ....................................................................................... 6
Contact allergy...................................................................................................... 11
Aims ........................................................................................................................ 20
Materials and methods ........................................................................................... 21
Patients ................................................................................................................. 21
Patch testing (paper I and II) ................................................................................ 22
Cell preparation and purification .......................................................................... 22
LTT ....................................................................................................................... 26
Cytokine assay ...................................................................................................... 27
Flow cytometry ..................................................................................................... 27
Statistics ................................................................................................................ 29
Results ..................................................................................................................... 31
Subject data .......................................................................................................... 31
Viability................................................................................................................. 31
LTT results ............................................................................................................ 32
Cytokine assay results ........................................................................................... 35
Flow cytometry results .......................................................................................... 40
Discussion................................................................................................................ 48
Conclusions .......................................................................................................... 56
Acknowledgements ................................................................................................. 58
References ............................................................................................................... 60
1
Popular Science Summary
Ca 10 % av alla patienter på hudkliniker som gör ett s.k. lapptest, uppvisar en reaktion efter
guldkontakt. Trots detta är det mycket ovanligt att patienterna uttrycker någon kliniskt relevant
allergi. Samtidigt har nästan alla som har positivt lapptest mot nickel (Ni) kliniska besvär av
metallen. Detta gör intresset för fördjupad kunskap och förbättrad eller komplementerande
diagnosmetoder stort.
I artikel I undersöktes tre patientgrupper: en med positivt lapptest mot guld; en med negativt
lapptest; och en grupp med en irritantreaktion mot guld (en tillfällig reaktion som inte är
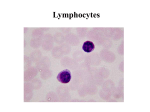
kopplad till allergi). Från patienternas blod renades immunceller, lymfocyter, fram, för att
undersöka delningshastighet samt vilka immunologiska markörer, s.k. cytokiner som
utsöndrades efter stimulering med guld. Resultaten visade att cellerna från allergiker delade sig
mer än celler från de två grupperna, samt utsöndrade högre nivåer av tre av cytokinerna,
nämligen Interferon (IFN) –γ, Interlukin (IL) -2 och IL-13. IFN-γ visade sig också vara det
cytokin som visade högst potential som diagnostisk markör.
I artikel II undersöktes bakomliggande mekanismer mer noggrant. Två patientgrupper
samlades in: En grupp med positivt lapptest mot guld som i artikel I visat hög celldelning och
höga nivåer av IFN-γ, och en grupp utan guldkänslighet. Från patienternas blod renades
lymfocyter fram, och dessa undersöktes sedan med avseende på celldelningshastighet, samt
vilken typ av celler som delade sig. Vi fann att i likhet med vad som är känt angående Niallergi, så var det T-celler av minnestyp som reagerade på guldet hos allergikerna. Dessa celler
uttryckte också en receptor kallad CLA, som får T-cellerna att vandra till huden. Däremot var
de tre andra receptorerna som undersöktes, CXCR3, CCR4 och CCR10, inte uttryckta i högre
nivåer hos allergikerna än icke-allergikerna, vilket har visats vid Ni-allergi.
Slutsatserna är att de celler som delar sig hos allergiker efter guldstimulering är av minnes-T
typ som är destinerade för huden. Till skillnad från Ni-allergi, så uttrycker de här cellerna inte
receptorerna CXCR3, CCR4 och CCR10 i någon högre grad. Cellerna utsöndrar både typ 1markörer (IFN-γ, IL-2) och typ 2-markörer (IL-13), vilket stödjer vissa teorier om Ni, medan
andra hävdar att Ni-stimulerade celler endast uttrycker typ-1 markörer.
2
Original Publications
I
Christiansen J*, Färm G, Eid-Forest R, Anderson C, Cederbrant K, Hultman P.
Interferon-gamma secreted from peripheral blood mononuclear cells as a possible
diagnostic marker for allergic contact dermatitis.
Contact Dermatitis. 2006.Aug;55(2):101-12.
II
Clifford J, Anderson C, Cederbrant K, Hultman P.
T-cells expressing CD4, CD45RO and CLA from gold-allergic but not healthy subjects
react to gold sodium thiosulphate in vitro.
Manuscript.
*The Author’s maiden name was Christiansen.
3
Abbreviations
ACD
Allergic contact dermatitis
AP-1
Activator Protein 1
APC
Antigen presenting cell
Au
Gold
CD45R0-EF
CD45R0 -Enriched fraction
CD45RA-EF
CD45RA-Enriched fraction
CLA
Cutaneous lymphocyte-associated antigen
CPM
Counts per minute
DC
Dendritic cell
EPI-
Epicutaneous patch test negative
EPI+
Epicutaneous patch test positive
EPI-IR
Epicutaneous patch test irritant reaction
FasL
Fas Ligand
GSTM
Gold sodium thiomalate
GSTS
Gold sodium thiosulphate
Hg
Mercury
HMGB1
High mobility group box chromosomal protein
IFN
Interferon
IL
Interleukin
IR
Irritant Reaction
LTT
Lymphocyte transformation test
MFI
Mean fluorescence intensity
MHC I/II
Major Histocompatibility Complex Class I/II
NFΚB
Nuclear Factor ΚB
Ni
Nickel
NK
Natural Killer cell
PBMC
Peripheral blood mononuclear cells
PI
Propidium Iodide
PRR
Pattern recognition receptor
RA
Rheumatoid Arthritis
4
SI
Stimulation index
TCR
T-cell receptor
TGF
Tumour growth factor
Th1/Th2
T helper 1/2
TLR
Toll-like receptor
TNF
Tumour necrosis factor
Treg
Regulatory T-cell
5
Introduction
T-cells and T-cell memory
T-cell production and maturation
T-cells are a cell type that is heavily involved in the immune response. The cells are
produced in the thymus, from progenitor stem cells that have migrated there from the
bone marrow (reviewed in (1)). To become mature T-cells, the progenitor cells go
through several control steps of different gene rearrangements, and the cells that fail to
rearrange their α-chain- and β-chain genes are induced to undergo apoptosis (2). Among
the surviving thymocytes, cells with low-affinity T-cell receptors (TCRs) and TCRs
recognising self-peptides are stopped from further development.
The cells that leave the thymus for the blood stream are mature naïve T-cells
expressing either CD4 or CD8 on their surface (2). The T-cells then circulate through the
blood stream and lymphatic system where they are available for antigen presenting cells.
Fig. 1 shows a schematic description of the development of T-cells.
T-cell activation and antigen presentation
When a potential pathogen enters the body, it is quickly engulfed by various
phagocytosing cells, such as macrophages or dendritic cells (DCs), residing at the
various body linings (3). The phagocytosing cell becomes activated, and migrates to a
lymph node, where it can present the processed antigen to T-cells. These antigen-bearing
cells are collectively termed antigen-presenting cells (APCs).
The phagocytosing cells have several methods for recognising non-self substances in
the body. The main recognition method is through various receptors recognising foreign
patterns, so called pattern recognition receptors (PRRs). The main receptor type for this
is the family of Toll-like receptors (TLRs) (4). When these receptors bind structures that
6
are foreign to the body, the phagocytosing cells become activated (fig. 2), and engulfs
the foreign body.
Figure 1. Schematic diagram of the differentiation and maturation of T-cells, from stem cells to active
T-cells. Adapted from Janeway (5).
Activated macrophages engulf foreign exogenic pathogens and digest them in the
lysosomes, which are acidic compartments in the cell where pathogens are degraded into
short peptide sequences (6, 7). These peptides are then transported to the macrophage
cell surface, where they are displayed on Major Histocompatibility Complex (MHC),
primarily on the class II receptors. The macrophage also starts to secrete cytokines, such
as Interleukin (IL) -1β, IL-12, IL-6 and Tumour Necrosis Factor (TNF) -α, which are
proinflammatory, as well as chemokines such as IL-8, which acts as a chemoattractant to
attract other immune cells to the site of infection (8). Neutrophils already circulating in
7
the blood stream arrive first, and when they engulf the pathogens, also secrete
chemokines. This will help to increase the chemokine
chemokine gradient to the site. The activated
macrophage then receives signals from the active lysosomes to start migrating into the
lymphatic system to a lymph node, where it can activate T-cells (3).
Figure 2. The process of activating T-cells. In A, invading pathogens are met by resident macrophages
(yellow) and DC (blue). These cells recognise pathogen patterns with their TLR (black), bind and
engulf the pathogens, and degrade them intracellularly. The degrade
degraded
d peptides are then displayed on the
MHC molecules (green) on the cell surface, and the cells start to secrete cytokines (TNF-α, IL-1β, IL12) and chemokines (IL-8) to attract other lymphocytes. The activated phagocytic cells (here only the
DC is shown) migrate in the lymphatic system to the nearest lymph node (B), where they can meet
circulating T-cells. When a T-cell recognises the antigen, displayed on the DC surface, with their TCR
(black double ovals), antigen presentation takes place. The T-cell then begins to proliferate (C), to
produce armed effector cells. These cells then migrate back to the inflamed tissues (D), where they
secrete cytokines (IFN-γ, IL-2) to further activate the residing B-cells, cytotoxic T-cells or phagocytic
cells (here, only a macrophage is shown). DC: Dendritic cell. TLR: Toll-like receptor. MHC: Major
Histocompatibility Complex. TNF: Tumour Necrosis Factor. IL: Interleukin. TCR: T-cell receptor. IFN:
Interferon.
8
Mature naïve T-cells express the TCR on their surface, which is a receptor that
recognizes MHC I or II (1). However, the receptor will only activate the T-cell if the
MCH displays a peptide for which the T-cell is specific (3). When the activated
macrophage enters the lymph node, it can encounter a circulating T-cell. The
macrophage then acts as an APC, and the T-cell becomes activated. It enters the blood
stream from the lymph node, and starts to express chemokine receptors which will help
the cell to migrate towards the gradient of chemokines.
When the T-cell becomes activated, it starts to proliferate to produce active, armed Tcells. These cells then start to express various chemokine receptors that induce the cell to
migrate towards the chemokine gradient to the site of infection (9, 10). Different
chemokines and other adhesion molecules are expressed at different locales in the body.
For instance, epithelial cells in the skin express the ligand for the cutaneous lymphocyteassociated antigen (CLA), and T-cells expressing CLA are thus directed to the skin (11).
Other, similar specific ligands exist in the airway system and the gut mucosa as well (12,
13).
Depending on what kind of pathogen has invaded the body, the T-cell will react in
different ways (1, 14-16). If it is an intracellular pathogen or a virus, the Th1 branch of
the immune system will be activated, with activated cytotoxic CD8+ T-cells and
aggressive macrophages as effector cells. If it’s a soluble antigen, the Th2 branch will
instead be activated, with plasma cells and antibodies as a response. These two branches
of the immune system secrete different sets of cytokines (see below), that also inhibit the
other immune type.
T-cell subsets
There are two major kinds of T-cells: T helper cells (Th-cells), which express the coreceptor CD4 that recognises MHC II, and cytotoxic T-cells, expressing the co-receptor
CD8 that recognise MHC I (1). CD4+ T-cells also exist in different varieties, which are
9
classified according to what cytokines they secrete (17). Th1 cells, which are mainly
focussed on viral combat and the cellular branch of the adaptive immune system, secrete
mainly Interferon (IFN) -γ and IL-2 (14-16, 18). This activates primarily macrophages,
which in turn secrete TNF-α, IL-6 and IL-1β, and CD8+ T-cells that help kill infected
cells (8). The cytotoxic CD8+ T-cells help to kill infected cells using different cytotoxic
enzymes, as well as death-inducing receptors (including the Fas – Fas Ligand (FasL)
system) (19).
Th2, which mainly activate the adaptive immune response involving antibodies,
secrete mainly IL-4, IL-5, IL-10 and IL-13, which in turn primarily activates B-cells
(14-16, 20, 21). Regulatory T-cells (Treg), that regulate the immune responses, express
the receptor CD25 and secrete mainly Tumour growth factor (TGF) –β, IL-4 and IL-10,
to help contain infections and stop immune reactions (22).
Recently, another Th subset has been defined, called Th17 (reviewed extensively in
(23)). This subset secretes a distinct selection of cytokines, including IL-1b, IL-6, IL-21,
IL-22, IL-23, and of course IL-17. The functions of Th17 cells are still being explored,
but it seems that the Th17 response results in a massive inflammation when infections
are not completely cleared by either Th1 or Th2 reactions (24).
T-cell memory and the CD45R receptor
T-cells express a receptor on their surface called the CD45R (25, 26). This receptor
exists in several different isoforms, and these are expressed differently depending on the
maturity level of the T-cell. Naïve T-cells express the CD45RA isoform, but upon
activation, this receptor is gradually down-regulated, and the differently spliced isoform
CD45R0 is expressed instead (26). This has proven to be a relatively good marker for
naïve or activated T-cells. However, the activated T-cells that turn into memory cells
continue to express the CD45R0 isoform, and circulating T-cells expressing this isoform
in healthy individuals are therefore considered to be memory T-cells. It has been shown
10
that the expression of the different isoforms is cyclic, at least in vitro, and re-activated
memory cells (memory cells encountering their antigen a second time) can express both
isoforms simultaneously (27, 28).
Contact allergy
The four types of allergy in brief
There are different types of allergic reactions, but the most common classification
system was described by Coombs and Gell in 1963 ((29), reviewed in (30)). This system
divides allergic reactions into four different groups, depending on the mechanisms
involved (Table 1). Typical for allergic reactions is that they are all mediated chiefly by
the adaptive branch of the immune system.
Type I reactions are the immediate reactions that are mediated by a rapid release of
IgE (30). Typical examples of this reaction are hay fever (allergic rhinitis and/or
conjunctivitis) and asthma. Type II reactions are mediated by the humoral cytotoxic
cells, and involve IgM and IgG antibodies. A typical example of this is drug-induced
cytopenia, where the patients suffer from almost immediate rashes after ingestion of
drugs such as penicillin (30, 31). Type III reaction is mediated by immune complexes,
where the IgG and IgM antibodies target soluble antigens and form complexes. These
complexes then activate mast cells and other leukocytes, and 4-6 hours after antigen
introduction, the patients suffer from the reaction (30, 32). Depending on where in the
body the reaction occurs, different symptoms are expressed, but the more common ones
includes allergic alveolitis in the lungs, or vasculitis in blood vessel walls.
Finally, there is a fourth type of reaction termed the Type IV hypersensitivity
reaction, and one typical example of this is the tuberculin reaction (30, 33). This reaction
is antibody independent, and relies on phagocytic and cytotoxic T-cells, as well as CD4+
T-cells. Typically, symptoms do not occur until 24-48 hours after antigen exposure, and
11
this type of reaction occurs almost exclusively in the skin. Allergic contact dermatitis
(ACD) is classed as a Type IV reaction.
Table 1. The four main types of allergic reaction, described by Coombs and Gell.
Antibody-mediated reactions
Type I
Immediate
Mechansim
Symptoms
Ig-E mediated
Allergic
rhinitis
Bronchial
asthma
Type II
Humoral
cytotoxic
Druginduced
cytopenia
Cellmediated
reactions
Type III
Type IV
Immune
complex
mediated
Vasculitis
Delayed
Allergic
alveolitis
T-cell mediated
Allergic contact
dermatitis
Tuberculin
reaction
Allergic Contact Dermatitis
Contact allergens normally occur as low molecular weight, soluble compounds,
called haptens, which can freely enter the skin (34-39). There are several ways that
haptens can interact with the immune system. Some compounds can react
pharmacologically, thereby activating the immune system (40). Other substances are
classed as pro-haptens, which need to be metabolized before they can cause an allergic
reaction. The way that is most probable regarding gold is that the Au ions bind
covalently directly to proteins, thereby changing the protein structure (40, 41). This
makes the “new” haptenated protein a target for DC, which then engulf the protein and
displays it on their MHC II molecules (36). During the sensitization phase, the DC
becomes active and migrates to the local lymph node where it presents the haptenated
protein to T-helper cells. The CD4+ T-cell then starts to proliferate and activate CD8+
cells, as well as generating hapten-specific memory cells (reviewed in (35). This
reaction can take up to 15 days, and is usually asymptomatic.
12
When the allergen is encountered a second time, the memory cells react faster, and an
elicitation phase takes place (fig. 3) (42, 43). Cytokines secreted from activated DCs,
including IL-1β and TNF-α, promptly activates surrounding cells, including
keratinocytes and residing lymphocytes (36, 44). Cells of a Th1 type secrete IFN-γ and
IL-2, which also activates keratinocytes (KC). These active KC also secrete cytokines
and chemokines, and recruit more cells from the circulation (45). Active CD8+ cytotoxic
T-cells target the activated KCs, and induce apoptosis through Fas-FasL interaction.
There is also evidence that Natural Killer cells (NK-cells) are involved in the pathogenic
mechanism, as they have been shown to infiltrate skin during the elicitation phase of
ACD (46). The damaged KCs are the central feature of the reaction, but other cells in the
epidermis and dermis are also involved. The reaction is then controlled by Tregs
secreting TGF-β, IL-10 and IL-4 (47).
The symptoms of ACD are classically erythema, papules and vesicles, but the
appearance can also include weeping and crusted to lichenified, scaling rashes,
depending on the extent and timing of the exposure (48). Since the reaction can take up
to 5 days to develop, detailed attention to the clinical history together with extensive
patch testing is needed, to elucidate whether a particular allergen caused the rash. Since
the visual symptoms can be similar to several other skin dermatoses, including atopic
dermatitis, fungal infections, and a long list of less common inflammatory disorders,
these need to be ruled out in the diagnostic process as well (48).
The distribution of the rash is dependent on the type of exposure, and sometimes this
can be an aid in diagnosis (49). For example, allergy towards cosmetics and hair dyes
frequently result in rashes where these are applied (face and hands).
13
Figure 3. Schematic of the Type IV hypersensitivity reaction. When an allergen (red dots) is
encountered and enters the skin, it is bound to protein (olive lines) and engulfed by DC (blue cells)
expressing PRRs. The DC then migrates to the lymph node and activates T-cells. If the antigen is
present for a sufficiently long time, a rash develops even after the sensitization phase, when the
activated T-cells arrive at the exposed site. If the antigen has been encountered before, there are
circulating and skin-residing memory T-cells (pink) that immediately recognise the antigen-MHC
complex. The activated T-cell then proliferates, and the armed T-cells then migrate back to the skin to
exert their actions. The CD4+ T-cell activates phagocytic cells (yellow) and further stimulates cytotoxic
CD8+ T-cells. The CD8+ T-cells exert their effects on the KCs (light blue), inducing these to undergo
apoptosis (blurred KC) through the Fas – FasL interaction. Meanwhile, Regulatory T-cells expressing
CD4 and CD25 secrete inhibiting cytokines (IL-10 and TGF-β) to control the reaction. DC: Dendritic
cell. PRR: Pattern recognition receptor. MHC: Major Histocompatibility Complex. KC: Keratinocyte.
IL: Interleukin. TGF: Tumour growth factor. IFN: Interferon. CLA: Cutaneous Lymphocyte-associated
antigen. FasL: Fas Ligand.
14
Examples of allergens and exposure
Depending on the type of allergen, different exposure routes are available. One of the
most common allergens in western societies is nickel (Ni), and the symptoms from this
type of allergy often occur after wearing Ni-containing jewellery (50). Some coins also
contain Ni, which can be seen on the hands of Ni-allergic cashier workers. It is
suggested that up to 20 % of the general population suffer from Ni allergy (50).
Other common allergens include fragrances and preservatives (51). These can often
be pinpointed as the causative agent, but the difficult thing is to discern which of the
many ingredients in for example a topical lotion that is responsible for the rash. This is
important to know, for future avoidance.
Another group of chemicals that often causes ACD in exposed workers are different
plastics and rubbers used in gloves. Among nurses, 30 % had patch tests positive to
different rubber components (52). This trend can be seen in many different industries,
where the exposed workers are more sensitized than the average population (52).
The focus of this thesis is ACD to gold. Approximately 10 % of patch tested patients
at dermatology clinics show a positive reaction to gold sodium thiosulphate (GSTS) (53,
54), the compound used to diagnose ACD to gold (53). While this might indicate
sensitisation to gold, it is uncommon for these patients to experience any clinical
symptoms from gold usage. There are however examples of patients with restorative
gold in the oral cavity suffering from blistering related to the gold exposure, and ACD to
gold is a common side effect in Rheumatoid Arthritis (RA) patients receiving gold salt
treatment.
Oxidative states of gold
Gold exists in three different oxidative states (Au [0], Au [I] and Au [III]), which
have very different effects in the body (55). Au [I] is most commonly used as jewellery,
and the increasing popularity of piercing body parts with gold has been suggested as a
15
cause for ACD to gold (54). Metallic gold (Au [0]) is also used as restorative materials
in the oral cavity (56, 57), and saliva has been shown to slowly dissolve gold and
transport it via mucous membranes into the bloodstream (54). Dental gold can be
associated with oral lesions and dermatitis, and there is a correlation between ACD and
oral lesions in patients with oral gold materials (56-58).
Metallic gold has also been used to coat coronary stents in an effort to prevent
restenosis after a coronary blockage (59, 60). There are reports stating a higher
occurrence of restenosis with gold-plated stents than with titanium ones, and a recent
thesis published in Lund, Sweden, states that ACD to gold is more common among
patients with gold-plated stents than in the general population as well (61). This has
resulted in a discontinuance of the use of gold-plated coronary stents.
Gold salts containing gold in the Au [I] oxidation state (55, 62), have been used for
treatment of RA for the last 80 years (63, 64), and while it can have positive effects, a
major drawback is adverse effects, including skin rashes, occurring in up to half of all
treated patients (55). It has been shown that Au [I] is oxidized into Au [III] in lysosomes
of macrophages (65), and Au [III] shows more prominent anti-inflammatory and toxic
effects (66).
Mechanisms in gold allergy
In medicine, gold is mostly used for its immunosuppressive functions (63, 64). The
mechanisms are not completely known, but one way might be through inhibition of the
inflammatory mediator High mobility group box chromosomal protein 1 (HMGB1) (67).
HMGB1 is translocated from the nucleus into the cytoplasm in monocytes in response to
other inflammatory mediators, such as IFN-β and nitric oxide (67). Gold is also known
to inhibit lymphocyte maturation, differentiation and function (68), as well as decrease
the production of several cytokines in vitro (69-71), including IL-1β, TNF-α and IFN-γ.
One way by which this is accomplished is through inhibition of transcription factors
16
such as Activator Protein (AP) -1 or Nuclear Factor (NF) ΚB, as well as inhibiting
specific caspases needed for post-translational modification of proteins (69). Both of
these transcription factors are heavily involved in the inflammation response, regulating
the transcription of several cytokines and signal proteins.
T-cells in ACD to metals
Although it is well known that gold and other metal haptens can cause ACD, the
details of the mechanism are still unknown (54, 72, 73). Gold bound to proteins is
digested and presented to T-cells by APCs (34, 37-39), but hapten recognition has also
been suggested to be APC independent (74). One suggestion is that gold binds directly
to the MHC class II molecules, thereby changing their peptide-binding ability (39).
ACD is a type IV hypersensitivity reaction, and both CD3+CD8+ and CD3+CD4+ Tcells are reported to be participating in the reaction (34, 75). Different compartments of
the body contain different percentages of metal-specific CD8+ T-cells in sensitized
individuals; 33 % were found in the blood of sensitized individuals, but only 15 % in the
skin (76). One theory states that both CD3+CD8+ T-cells and CD3+CD4+ Th1 cells,
secreting cytokines such as IFN-γ, IL-13 and IL-2, are the effector cells in ACD (71, 77).
Regulatory CD3+CD4+ T-cells and Th2 cells then exert negative feedback on the
immune response by secreting inhibitory cytokines such as IL-10, IL-4 and IL-5 (36, 78,
79). Other publications identify only CD3+CD4+ cells of a Th1 type to be the major
culprit in the ACD reaction (75, 80-82). Another theory states that the type of reaction
(Th1 or Th2) is dependent on the microenvironment surrounding the naïve T-cells (76).
In non-allergic donors, Ni seems to activate both naïve (CD3+CD45RA+) and
memory (CD3+CD45R0+) cells in vitro (83). However, in allergic subjects, Ni
exclusively
activates
memory
T-cells
(CD3+CD45R0+),
particularly
CD3+CD4+CD45R0+ cells, leaving naïve T-cells (CD3+CD45RA+) unstimulated (80,
83). Ni-activated CD3+CD45R0+ cells also express the skin-homing receptor CLA and
17
the chemokine receptors CXCR3, CCR4 and CR10 (80). To our knowledge, no data
regarding gold allergy in this respect have been published.
Diagnosis of ACD
Patch testing is considered the gold standard to identify ACD (84). The protocols for
testing are well known, and extensive knowledge exists for many of the approximately
3000 allergens known to induce ACD (85). There are, however, some drawbacks with
this technique: The procedure is time-consuming for both patient and physician, with
one visit for the patch placement and at least one more visit to the clinic for test reading.
The risk for a flare of allergic reactions in a previously sensitized individual is slight, but
exists (86), and there is a risk of creating new sensitivity in the subject. The results may
differ between different test occasions, and the reading of the test is subjective (86-88).
Furthermore, the correlation between dermatological symptoms and patch test outcome
relevance varies between contact allergens: In the majority of patch test positive cases,
no clinical relevance can be found. Many patients show an irritant reaction (IR), which
might be interpreted as a false positive result if the morphology is incorrectly read (85).
The IR is caused by direct damage to the skin, mainly the keratinocytes (89), and is
dependent on test substance concentration. At present, a dilution series of the test
substance can be the only way to distinguish between an allergic and irritant reaction
(IR), since decreasing concentrations of the allergen results in disappearing rashes if it is
an IR. Repeated testing increases the cost for both patients and health care systems.
Thus, interest in a blood sample based diagnosis has been, and still is, high.
One such blood-based method is the lymphocyte transformation test (LTT), which
shows a relatively high correlation to patch test to gold, although the method has so far
only proved useful at a group level (71, 90). The method relies on the reactivity of
specific memory T-cells in vitro by specific allergen exposure (71, 91-93), and has been
used as an aid in diagnosing allergy since the 1960’s.
18
Knowledge of the role of cytokines in ACD has increased markedly in the last
decade. The use of cytokine fingerprinting has hitherto been used more frequently in the
predictive setting rather than in a diagnostic situation, evaluating new chemical entities
for their possible allergenic properties (94). With the development of DNA screening
chips, protein profiles can be evaluated more easily, and one or several might surface as
a candidate diagnostic marker.
19
Aims
The general aim of this thesis was to investigate mechanisms in gold allergy, by studying
the activation of lymphocyte subsets.
Specific aims were:
1) To study mechanisms of gold stimulation and/or inhibition on lymphocytes from
both allergic and non-allergic subjects.
2) To discuss potential similarities and/or differences between the mechanisms of
action for allergic contact dermatitis to gold and what is previously known about
Ni allergy.
3) To evaluate the use of different blood markers as predictors and/or diagnostic
tools for allergic contact dermatitis to gold.
20
Materials and methods
Patients
Paper I
The subjects were selected from patients on whom epicutaneous patch tests had been
performed, at the outpatient clinics of the Departments of Dermatology at the University
Hospitals of Linköping and Örebro, Sweden. The subjects were divided into three
groups; one with subjects who had shown a morphologically positive patch test for gold
(EPI+); one which had shown no positive test to the standard screening test panel patch
test series (95, 96) (EPI-); and one which had shown an IR for gold (EPI-IR). In this way
77 subjects (63 women and 14 men) with an age range of 22-80 yrs (52.6 ± 14.8, mean ±
SD), were recruited to the study.
The subjects were asked to answer a questionnaire about demographic data and
exposure to gold, including medication with gold salts, gold jewellery usage and dental
gold.
Paper II
Five allergic subjects were recruited at the outpatient clinic of the Department of
Dermatology at Linköping University Hospital. These patch test positive subjects had
been examined in our previous study (paper I:(71)), and were selected due to their high
LTT SI values and high IFN-γ levels.
Non-allergic subjects were recruited from healthy laboratory workers with no clinical
history of allergy to gold.
21
Patch testing (paper I and II)
The allergic subjects had undergone a patch test with a standard screening panel and
shown a positive reaction to 0.5 % and/or 2.0 % gold sodium thiosulphate (Na3[SO3]2)
(GSTS), in petrolatum (Chemotechnique Diagnostics, Malmö, Sweden), applied on Finn
Chambers (Epitest, Tuusula, Finland). The patches were left on for 48 hours, and tests
were read on days 3 and 7, and graded as: (-), negative reaction; (+), weak, nonvesicular response; (++), strong oedematous vesicular reaction, and; (+++), extremely
strong reaction, according to the European Contact Dermatitis Research Group (ECDR)
guidelines (39). All reactions that achieved at least a (+) grade were considered to be
positive reactions.
In paper I, thirty-three subjects (30 women and 3 men) showed a (+) – (+++) reaction
to gold, 28 (21 women and 7 men) showed no reaction at all to gold, and 16 (12 women
and 4 men) showed a morphologically separate IR. In paper II, the allergic subjects all
showed a (+) reaction or stronger. The non-allergic subjects in paper II were not
subjected to patch test.
Blood samples were taken at the dermatology department at Linköping University
Hospital. All test subjects had given informed consent. The study was approved by the
local ethics committee in Linköping.
Cell preparation and purification
Paper I
Venous blood was obtained in vacuum tubes containing Na-Heparin (Vacuette,
Greiner Bio-One, Krems-Muenster, Austria). The cells were separated on Ficoll Paque
Plus® (Amersham, Uppsala, Sweden) to obtain peripheral blood mononuclear cells
(PBMC). The cells were then suspended in RPMI 1640 with 10 mM Hepes, 4 mM Lglutamine, gentamycin (8 mg/ml) and 10 % heat-inactivated AB+ serum (all from Gibco
22
BRL, UK), at a concentration of 1 x 106 cells/ml.
Six GSTS concentrations were used (1.56 - 50.0 µg/mL) (Chemotechnique
Diagnostics) to stimulate the cells, as well as sterile Milli-Q water as solvent control. All
samples were run in duplicate. The metal salt solution or sterile water was added with a
total of 1 x 106 cells/well to flat-bottomed 24-well plates (Costar, Cambridge,
Massachusetts, USA), and incubated for 5 days at 37 °C and 5 % CO2.
Paper II
PBMC were obtained in the same manner as described for Paper I. Cells from the
PBMC fraction were suspended in phosphate buffered saline (PBS) with 0.5 % human
AB+ heat-inactivated serum (Invitrogen, Carlsbad, CA, USA) and 2 mM EDTA. The
suspension was mixed with a magnetic bead kit for purifying T-cells (Pan T-cell kit,
Miltenyi Biotech, Bergisch Gladbach, Germany) targeting CD14, CD16, CD19, CD36,
CD56, CD123, and CD235a, leaving only CD3 cells unlabelled, and the cells were
separated according to the manufacturer’s instructions. Briefly, the cell-antibody cocktail
was incubated in room temperature (RT) for 15 minutes and then added to a magnetic
separation column (Miltenyi Biotech).
Two different cell fractions were obtained: One unlabelled T-cell fraction (henceforth
referred to as the T-cell fraction) and one labelled non-T cell fraction (henceforth
referred to as the non-T fraction). The non-T fraction was stored on ice until used as a
monocyte supply in the cultures.
The T-cell fraction was resuspended in PBS with 0.5 % human AB+ heat-inactivated
serum and labelled with CD3-APC-Cy7, CD45R0-PE-Cy7 (e-bioscience, San Diego,
CA, USA) and CD45RA-Pacific Blue (Becton Dickinson (BD), Stockholm, Sweden) for
15 minutes in RT. The cells were then washed with PBS and sorted on a FACS Aria II
Cellsorter (BD), into two different fractions, one CD3+CD45RA+ enriched fraction,
henceforth referred to as the CD45RA-EF and one CD3+CD45R0+ enriched fraction,
23
referred to as the CD45R0-EF. A summary of the separation procedure is shown in fig.4.
After separation, the different fractions obtained during the separation procedures
(PBMC-fraction, T-cell fraction, non-T fraction, CD45RA-EF and CD45R0-EF) were
analysed for purity, using the following antibodies: CD3-FITC, CD4-APC, CD45RAPE, CD14-FITC, CD19-APC, CD56-PE (all from Miltenyi Biotech) and CD45R0-PECy5 (BD). The staining procedure was the same as mentioned above, and the cells were
analyzed on a FACS Aria (BD).
Purity and enrichment
The T-cell fraction consisted on an average of 92.2 % and 94.4 % CD3+ cells in the
allergic subjects and non-allergic subjects respectively, and they had been enriched 1.43
and 1.55 times compared with the PBMC fractions. Almost all monocytes (CD14+), Bcells (CD19+) and NK-cells (CD56+) were depleted with the magnetic beads: 1.6 % of
monocytes remained in the T-cell fraction obtained from allergic subjects after depletion.
The CD45RA-EF was very pure, with 99.4 % and 98.0 % CD45RA+ cells in the
allergic group and the non-allergic group, respectively. The CD45RA+ cells had been
enriched 2.15 times in the allergic group and 1.53 times in the non-allergic group
compared with the T-cell fraction. For the CD45R0-EF, the CD45R0+ cell fractions were
98.5 % in the allergic group and 95.7 % in the non-allergic group, and the CD45R0+
cells had been enriched 3.08 times and 6.05 times, respectively, compared to the T-cell
fraction.
24
Figure 4. Summary of the cell preparation in paper II.
For culturing of the CD45RA-EF and CD45R0-EF, 48-well flat-bottomed culture
plates (BD) were coated with the non-T fraction suspended in RPMI 1640 with 10 mM
HEPES, 4 mM L-Glutamin, Gentamycin (8 mg/ml) and 30 % human AB+ heat-
inactivated serum (all from Invitrogen) at a concentration of 1 x 107 cells/ml for 4-6
hours, to obtain adherent monocytes in the wells. The plates were then washed with
medium, and the CD45RA-EF and CD45R0-EF cells were added to 48-well flatbottomed plates (BD) in RPMI 1640 with 10 mM HEPES, 4 mM L-Glutamin,
Gentamycin (8 mg/ml) and 10 % human AB+ heat-inactivated serum at a concentration
of 1 x 106 cells/ml. The PBMC cells were added directly to wells in the same
concentration, since this fraction already contained monocytes.
25
The cells were cultured for 4 - 5 days in 37 °C and 5 % CO2, with five different
concentrations of GSTS (25.0– 200 µg/ml) in sterile Milli-Q water, which was also used
as a solvent control.
LTT
Paper I
After 5 days of culturing as described above, LTT was performed according to
Nordlind and Lidén (97) with some minor modification (90). 4 - 18 h before harvesting,
1 µCi 3H-thymidine, specific activity 12.7 GBq/mg (Amersham) in 10 µl of RPMI
medium was added to each well. The cells were then harvested with an automatic cell
harvester (Inotech, Minolab, Upplands Väsby, Sweden), and the radioactivity was
measured using a 1450 Microbeta Plus (Wallac, Turkuu, Finland), and counts per minute
(CPM) was recorded.
From the LTT results, a stimulation index (SI) was calculated for each GSTS
concentration and subject, using the following formula:
SI = mean CPM (GSTS stimulated)/mean CPM (unstimulated)
The GSTS concentration yielding the highest LTT SI values was considered optimal.
Paper II
After 4 days of culturing as described above, LTT was performed on the PBMC
fraction from non-allergic subjects and the CD45RA-EF and CD45R0-EF from allergic
and non-allergic subjects according to Nordlind and Lidén (97) with some
modifications. 120 µl from each well was transferred to a 96-well, flat-bottomed plate
(BD). To each well 1 µCi 3H-thymidine, specific activity 12.7 GBq/mg (Amersham) was
26
also added. After 5-6 hours of incubation, the cells were harvested using an automatic
cell harvester (Inotech, Ninolab), and the radioactivity was measured using a 1450
Microbeta Plus (26) and CPM were recorded. The same formula for calculating SI
values as described above was used.
Cytokine assay
Paper I
Eight cytokines were measured in the cell supernatants; IL-1β, IL-2, IL-4, IL-8, IL10, IL- 12, IL-13 and IFN-γ. The cells were cultured as described above for paper I,
although only the GSTS concentrations 6.25 and 25.0 µg/ml were used. The supernatant
was collected after 3, 4, and 5 days and frozen at -70 °C until further analysis. The
multiple bead array Luminex (Linco Research Inc., Missouri, USA) was used to
quantify the cytokines, according to the manufacturer’s instruction (Linco Research Inc.,
Missouri, USA) with RPMI medium as blank. A Luminex 100 IS instrument (Biosource,
Nivelles, Belgium) with the Star Station acquisition program (v2 Applied Cytometry
Systems, Sheffield, UK) was used to process the data. All samples were run in single
wells, except the standard curve points, which were run in duplicate according to the
manufacturer’s recommendations. “Net” concentrations were then calculated by
subtracting values for unstimulated samples from the stimulated samples. Culture
conditions (culture time and GSTS concentrations) yielding the highest mean net
concentrations were considered optimal.
Flow cytometry
Paper II
Cells from the cultured PBMC fraction from non-allergic subjects were used for flow
27
cytometry analysis. Briefly, the cells were suspended in PBS with 0.5 % human AB+
heat-inactivated serum (Invitrogen) and labelled for 15 minutes in RT with the following
antibodies: CD3-FITC, CD4-APC, CD45RA-PE, CD14-FITC (all from Miltenyi
Biotech), CD8-PE-Cy5 and CD45R0-PE-Cy5 (BD). The cells were washed with PBS
and analysed on a FACS Calibur (BD), using FACS CellquestPro software (BD).
The cultured cells from the PBMC fraction were also labelled with propidium iodide
(PI) (BD) to determine viability. Briefly, the cells were stained with 2.5 % PI in PBS
with 0.5 % human AB+ heat-inactivated serum (Invitrogen), then washed with PBS and
analysed on a BD FACS Calibur (BD). The cells were plotted in a histogram, where the
cells with positive PI-staining (considered as dead cells) were selected with a gate.
These cells were then back-gated into a forward/side-scatter dot plot, to determine the
location of the dead and living cells. Due to a shortage of cell material from the
separated fractions, this procedure could not be performed on the CD45RA-EF and
CD45R0-EF. However, since the staining and localization of the dead and living PBMC
cells was highly reproducible, the above back-gating was also performed on the
separated cell fractions, where the same localization of living and dead cells were clearly
visible.
Cells from the cultured CD45RA-EF and CD45R0-EF were also analysed by flow
cytometry. The staining procedure was the same as for the PBMC fraction described
above, but included the additional antibodies CLA-PE, CD19-APC, CD56-PE
(Miltenyi), CD25-APC, CCR4-PE, CXCR3-PE-Cy5 (BD) and CCR10-APC (R&D
systems Europe Ltd., Abingdon, UK). The cells were analysed on a FACS Aria II
Cellsorter (BD) using FACS Diva software (BD).
28
Statistics
Paper I
Specificity, sensitivity and accuracy were calculated using epicutaneous patch test as
a reference, according to the following formulas:
Sensitivity = No of analysis positives (in the EPI+ group) x 100 / Total No of EPI+.
Specificity (EPI-) = No of analysis negatives (in the EPI- group) x 100 / Total No of EPI-.
Specificity (EPI-IR) = No of analysis negatives (in the EPI-IR group) x 100 / Total No of EPI-IR.
Accuracy = (No of analysis positives in the EPI+ group + No of analysis negatives in the EPIgroup + No of analysis negatives in the EPI-IR group) / Total No of subjects.
To evaluate whether the methods used were able to identify the EPI-IR subjects as
non-allergic, specificity was calculated separately for the EPI- and EPI-IR groups. All
concentrations and SI values were used in the cut-off determinations. The cut off value
(expressed as cytokine concentration and LTT SI) that yielded the highest accuracy was
defined as the point which resulted in the highest simultaneous sensitivity and
specificity. A prerequisite for these calculations was that both sensitivity and specificity
each had to be > 50.0 %.
Fisher’s exact test was used to compare scores from the questionnaires. Correlations
were calculated with Spearman’s non-parametric test. When correlating the cytokines to
LTT, the GSTS concentration 25.0 µg/ml was used for both the cytokines and the LTT.
When correlating the cytokines to each other, the same GSTS concentration and day was
used for each calculation. Linear regression was calculated to evaluate the dose-response
relationship for the LTT SI values and GSTS concentrations.
Results from the cytokine quantifications are presented for day 5 at GSTS
concentrations of 6.25 or 25.0 µg/ml, depending on which concentrations caused the
29
highest net cytokine production. The non-parametric Kruskal-Wallis test and
Bonferroni’s post hoc test were used for comparisons between the three subject groups.
Friedman’s test was used to compare the SI response of the LTT at the different GSTS
concentrations.
The analyses were performed using GraphPad Prism 3.0 (GraphPad Software, San
Diego, California, USA) and MINITAB (Minitab Ltd., www.minitab.com).
Logistic regression
Logistic regression was calculated to evaluate the combined effect of detecting all the
cytokines and LTT. The formula achieved looked as follows:
k1 + (k2 x LTT) + (k3 x IFN-) + (k4 x IL-13) + (k5 x IL-2) + (k6 x IL-10) = K;
eK / 1+ (eK) = Kp
Where k1 - 6 represents constants given in the calculations, and Kp is the predictive
value. The value attained is between 0 - 1, where 1 = truly allergic, and 0 = not allergic.
Depending on the chosen cut-off, the accuracy varies. The analysis was performed on
the EPI+ and the EPI-groups with patch test results as reference, and the predictive
values were calculated for all subjects. The analysis was performed using MiniTab.
Paper II
To compare results between the subject groups, the non-parametric Kruskal-Wallis
test was used, and unadjusted exact p values were calculated. To compare between the
different concentrations of GSTS, Friedman’s test was used, and unadjusted p values
were calculated. Special regard was taken to missing values. To help determine the
effect of GSTS, linear regression was calculated for all the parameters as well. Statistical
analyses were performed using GraphPad Prism 5.0, SPSS for Windows (SPSS Sweden
AB, Kista, Sweden) and MiniTab.
30
Results
Subject data
Paper I
There were no differences between the three subject groups, EPI+, EPI- and EPI-IR,
regarding jewellery usage and presence of dental gold. No patients had been treated with
gold-containing medications.
Paper II
The allergic subjects were aged 49 ± 7.8 years, all were female, and 6 - 10 years had
passed since patch testing. The non-allergic subjects were aged 27 ± 2.9 years (which
was significantly different from the allergic subjects, p < 0.05), and all were female.
Viability
Paper II
The PBMC viability from non-allergic subjects showed an inverse dose-response
relationship to the GSTS dose (r2 = 0.81, p < 0.001) (fig. 5). There was a significant
decrease in cell viability in the CD45RA-EF and CD45R0-EF from both allergic and
non-allergic subjects after exposure to 50.0 µg/ml GSTS compared with unstimulated
cells (p < 0.01 for all four groups) (fig. 5). The inverse dose-response relationship
between viability and GSTS dose was significant for both the CD45RA-EF (r2 = 0.62, p
< 0.01) and the CD45R0-EF (r2 = 0.53, p < 0.05) from the non-allergic subjects and for
the CD45R0-EF (r2 = 0.7, p < 0.01) from the allergic subjects.
31
Figure 5. Viability in the PBMC fraction from non-allergic subjects and in the CD45RA-EF and
CD45R0-EF from both allergic and non-allergic subjects, from paper II. Briefly, cells were stained with
propidium iodide and analyzed with a FACS Aria Flow Cytometer, to evaluate living and dead cell
populations. GSTS: Gold sodium thiosulphate. **: p < 0.01. $: significant linearity, p < 0.05. $$:
significant linearity, p < 0.01. $$$: significant linearity, p < 0.001. Significance levels were calculated
using Friedman's testt
LTT results
Paper I
The optimal GSTS concentration for LTT was 50.0 µg/ml. The EPI+ group had
significantly higher SI values than subjects with a negative patch test did, at all GSTS
concentrations (p < 0.05 or lower, data not shown), which was most significant at GSTS
concentration 50.0 µg/ml (fig. 6A). There were no significant differences between the
EPI+ group and the EPI-IR group at any GSTS concentration, with the single exception
at GSTS concentration 3.13 µg/ml, where EPI+ subjects showed higher SI values (p <
0.05, data not shown). There were no significant differences between the EPI- group and
32
the EPI-IR group at any GSTS concentrations.
The SI values for all subjects showed a significant dose-response relationship to
GSTS (r = 0.43, p < 0.001), with the strongest linearity in the EPI- group (r = 0.50, p <
0.001) (fig. 6A). The highest rise in SI in response to increased GSTS concentration
was, however, found in the EPI+ group.
Maximal accuracy for diagnosing ACD with LTT, 75.3 %, was obtained using the SI
cut-off 7.9 at GSTS concentration 50.0 µg/ml. The sensitivity was 54.5 % and the
specificities for the EPI- and the EPI-IR groups were 92.9 % and 87.5 %, respectively.
(Table 2)
Paper II
While the cells from non-allergic subjects showed a decreased proliferation after
GSTS exposure, the cells from allergic subjects showed an increased proliferation
compared to the unstimulated cultures (fig. 6B). The CD45R0-EF and CD45RA-EF
from non-allergic subjects showed a significant decrease in SI with increased doses of
GSTS, with a significant inverse dose-response relationship (r2 = 0.5, p = 0.0003 for the
CD45RA-EF and r2 = 0.39, p = 0.003 for the CD45R0-EF) (fig. 6B). The PBMC
fraction from non-allergic subjects showed a slight increase in proliferation at 25.0 and
50.0 µg/ml GSTS, but this increase was not significant (fig. 6B). The CD45R0-EF from
the allergic subjects showed a significant dose-response reaction (r2 = 0.39, p = 0.002),
with increasing SI following increasing GSTS exposure (fig. 6B).
33
Figure 6: LTT results. In A, the LTT results from paper I are shown, for the three subject groups (EPI+, EPI- and EPI-IR). In B,
the results from paper II are shown, with all culture variants (PBMC from non-allergic subjects, CD45RA-EF and CD45R0-EF
from both allergic and non-allergic subjects). The CD45RA-EF is plotted on the right axis due to the large variations in this group.
*: p < 0.05. **: p < 0.01. ***: p < 0.001. $$: significant linearity, p < 0.01. $$$: significant linearity, p < 0.001. Significance
levels were calculated using Kruskal-Wallis test and Friedman’s test. GSTS: Gold sodium thiosulphate. PBMC: Peripheral blood
mononuclear cells. LTT: Lymphocyte transformation test. SI: Stimulation index.
34
Table 2. Maximal accuracy, sensitivity and specificity for the different cytokines and LTT assays.
Included
Accuracy Sensitivity Specificity Specitivity
Cut-off
variables
(%)
(%)
(%)
EPI-IR (%)
LTT*
75.3
54.5
92.9
87.5
7.9₤
IFN-ㆧ
IL-13‡§
IL-2†¥
IL-10†¥
83.1
76.6
74.0
64.9
81.8
78.8
60.6
60.6
82.1
71.4
89.3
71.4
87.5
81.2
75.0
62.5
0.0#
0.0#
3.41#
0.0#
LTT*, IFN-ㆧ
80.5
66.7
92.9
87.5
0.55
‡§
‡§
80.5
72.7
89.3
81.3
0.55
LTT*, IFN-γ , IL-13
*Values obtained at a GSTS concentration of 50.0 µg/ml. †Values obtained at a GSTS concentration of
6.25 µg/ml. ‡Values obtained at a GSTS concentration of 25.0 µg/ml.§ Values obtained at day 5. ¥Values
obtained at day 4. ₤Value shown is Stimulation index. #Values shown are pg/ml. Values shown from
the logistic regression calculations have no unit. EPI-IR, Epicutaneous patch tested irritant reactive
subject group. GSTS: Gold sodium thiosulfate. LTT, lymphocyte transformation test. SI, Stimulation
index. IL, Interleukin. IFN, Interferon.
Cytokine assay results
Paper I
IFN-γ
Optimal culture conditions for the IFN-γ measurement were obtained at day 5, at
GSTS concentration 6.25 µg/ml. The level of IFN-γ was significantly higher in the EPI+
group compared to the EPI- group and the EPI-IR group (fig. 7A), but no significant
difference was found between the EPI- group and the EPI-IR group. A modest but
significant correlation was found between IFN-γ for all days and LTT SI (Table 3).
The maximum accuracy for diagnosing ACD with IFN-γ assessment was 83.1 %, at
the cut-off value 0.0 pg/ml, (GSTS concentration 6.25 µg/ml at day 5). The
corresponding sensitivity was 81.8 % and the specificity 82.1 %. The specificity for the
EPI-IR group was 87.5 % (Table 2).
35
IL-13
Optimal culture conditions for the IL-13 measurement were obtained at day 5, and
GSTS concentration 25.0 µg/ml. The level of IL-13 was significantly higher in the EPI+
group at day five, compared to both the EPI- and the EPI-IR groups (fig. 7B). No
differences in IL-13 secretion were found at any day between the EPI- group and the
EPI-IR group. A modest but significant correlation was found at all days between IL-13
and LTT SI (Table 3).
When using IL-13 measurement to detect ACD, the maximum accuracy was 76.6 %,
with a sensitivity of 78.8 %, and specificity of 71.4 % and 81.3 % for the EPI- and the
EPI-IR groups, respectively (Table 2). The cut-off value was 0.0 pg/ml (obtained at
GSTS concentration 25.0 µg/ml, at day 4).
IL-2
Optimal culture conditions for the IL-2 measurement were obtained at day 4, at
GSTS concentration 6.25 µg/ml. The IL-2 level was significantly higher in the EPI+
group at all time points investigated, as compared with the EPI- group (fig. 7C). The
same applied for the difference between the EPI+ group and the EPI-IR group after 4
and 5 days. There was no significant difference in IL-2 secretion between the EPI- group
and the EPI-IR group. A relatively high, significant correlation existed between LTT SI
and the IL-2 levels after 3, 4, and 5 days (Table 3).
The maximum accuracy when using IL-2 measurement to identify ACD was 74.0 %
when using the cut-off value of 3.41 pg/ml. The corresponding sensitivity was 60.0 %
and the specificity for the EPI- group and the EPI-IR group was 89.3 % and 75.0 %,
respectively (Table 2). These values were obtained at GSTS concentration 6.25 µg/ml, at
day 4.
36
Figure 7. Results from the Cytokine Assay. A shows the results for the IFN-γ assay, B shows the results
from the IL-13 assay, C shows the results from the IL-2 assay, and D shows the results from the IL-10
assay. The significance levels were calculated using Kruskal-Wallis. *; p < 0.05. **: p < 0.01. ***: p <
0.001. IL: Interleukin. IFN: Interferon. EPI: Epicutaneous Patch test subject group (+: positive, -:
negative, IR: irritant reaction).
37
IL-10 levels
Optimal culture conditions for the IL-10 measurement were obtained at day 4, and a
GSTS concentration of 6.25 µg/ml. There were no significant differences in IL-10
secretion between any of the groups (Fig 7D). There was a weak correlation between IL10 and LTT at day 5 (Table 3), but not when means or sums were calculated.
The maximum accuracy was lower for IL-10 than for the other cytokines, 64.9 %,
with a sensitivity of 60.6 %, and a specificity of 71.4 % and 62.5 %f or the EPI- and the
EPI-IR groups, respectively (Table 2). These values were obtained using the cut-off
value of 0.0 pg/ml, at GSTS concentration 25.0 µg/ml, at day 5.
IL-1β, IL-4, IL-8 and IL-12
For IL-1β, IL-4 and IL-12, almost all values were below detection limit (data not
shown). For IL-8, more than half of the values were above detection limit. Due to lack
of extra material, a second trial using diluted supernatants could not be performed, and
these results are therefore not presented.
Correlation between the different cytokines
The most significant correlations were found using cytokine values at GSTS
concentration 25.0 µg/ml at day 5, where all the cytokines correlated significantly to
each other (p < 0.05, Table 3). The highest correlation was found between IL-13 and
IFN-γ (r = 0.6744, p < 0.001).
38
Table 3. Correlation between the different cytokines and LTT.
LTT
IFN-γγ
IL-13
Il-2
IL-10
LTT
X
0.41***
0.44***
0.24*
0.56***
IFN-γγ
0.41***
X
0.67***
0.40***
0.58***
IL-13
0.44***
0.67***
X
0.32**
0.59***
IL-2
0.24*
0.40***
0.32**
X
0.42***
IL-10
0.56***
0.58***
0.59***
0.42***
X
Cytokine values were included GSTS concentration 25 µg/ml and day 5, and LTT SI values were
included at GSTS concentration 25 µg/ml. GSTS: Gold sodium thiosulphate. LTT: Lymphocyte
transformation test. IFN: Interferon. IL: Interleukin*: p < 0.05. **: p < 0.01. ***: p < 0.001.
Correlation was calculated using Spearman’s non-parametric test.
Logistic regression
This analysis was performed to evaluate whether the sensitivity and specificity could
be improved by using the different cytokines simultaneously. Different combinations
using cytokines and LTT were used to find the optimal combinations. The cytokines
were included at the same GSTS concentration and culture day, and LTT was included at
GSTS concentration 50.0 µg/ml. The conditions that yielded the highest accuracy at
GSTS concentration 6.25 µg/ml, at day 5, yielded the following formula:
(-1,0258 + (0,15346 x LTT) + (0,02545 x IFN-))
e
(-1,0258 + (0,15346 x LTT) + (0,02545 x IFN-))
/ 1+ (e
)
The values obtained from this formula were 0 - 1. The highest accuracy, 80.5 %, was
obtained when using 0.55 as a cut-off; the sensitivity was 66.7 %, the specificity was
92.9 %, and the sensitivity for the EPI-IR group was 87.5 % (Table 4). The conditions
that yielded the highest accuracy when using the cytokines at GSTS concentration 25.0
µg/ml, at day 5, yielded the following formula:
(-1,0257 + (0,12575 x LTT) + (0,01533 x IFN-)) + (0,04829 x IL-13))
e
(-1,0257 + (0,12575 x LTT) + (0,01533 x IFN-))
/ 1 + (e
)
The highest accuracy, 80.5 %, was obtained when using 0.55 as a cut-off; the
sensitivity was 72.7 %, the specificity was 89.3 %, and the sensitivity for the EPI-IR
39
group was 81.3 % (Table 2).
Flow cytometry results
Paper II
CD3+ cell fraction
In the PBMC fraction from non-allergic subjects, the CD3+ fraction of cells decreased
at GSTS concentrations above 50.0 µg/ml (fig. 8), and was significantly reduced at 200
µg/ml GSTS (p < 0.05). The fraction of CD3+ cells in the CD45RA-EF and CD45R0-EF
from both the allergic and non-allergic subjects (data not shown) was largely unchanged
(mean range 73.4 %) within the GSTS dose range used (0.0 – 50.0 µg/ml).
CD3+CD4+ and CD3+CD8+ cell fractions
The fraction of CD3+CD4+ cells in the PBMC fraction from the non-allergic subjects
decreased at a GSTS concentration of 200.0 µg/ml, while the fraction of CD3+CD8+
cells started to decrease at concentrations above 50.0 µg/ml (fig. 8). Thus the ratio
between the CD3+CD4+ and CD3+CD8+ cells clearly increased at GSTS concentrations
above 50.0 µg/ml (fig. 8).
In the CD45RA-EF from both allergic and non-allergic subjects, the fraction of
CD3+CD4+ cells and CD3+CD8+ cells ranged from 49.5 % – 55. 5 % and 33.6 % – 49.6
%, respectively, and did not change within the GSTS dose range 0.0 – 50.0 µg/ml (data
not shown). In the CD45R0-EF from both allergic and non-allergic subjects (fig. 9), the
fraction of CD3+CD4+ cells tended to increase after GSTS exposure, while the fraction
of CD3+CD8+ cells tended to decrease, both in a dose-dependent manner. In the
CD45R0-EF from the allergic subjects, this trend was statistically significant (p < 0.01).
Thus the ratio between the mean fraction of CD3+CD4+ and CD3+CD8+ cells in the
CD45R0-EF from both allergic and non-allergic subjects increased with the GSTS dose,
40
although the differences were not significant.
Figure 8. CD3+, CD4+ and CD8+ cell fractions in PBMC from non-allergic subjects in paper II. GSTS:
Gold sodium thiosulphate. *: p < 0.05. $$: Significant linearity, p < 0.01. Significances were calculated
using Friedman’s test.
CD3+CD45RA+ and CD3+CD45R0+ cell fractions
In the PBMC fraction from non-allergic subjects, the CD3+CD45RA+ cell fraction
showed a significant decrease at 200 µg/ml GSTS (significant from GSTS concentration
50.0 µg/ml, p < 0.05) while the fraction of CD3+CD45R0+ cells started to decrease at
50.0 µg/ml GSTS, and the inverse dose-response relationship was significant (r2 = 0.28,
p < 0.05) (fig. 10). Thus, the ratio between the CD3+CD45RA+ cells and the
CD3+CD45R0+ cells increased with increasing GSTS concentrations (fig. 10).
41
Figure 9. CD4+ and CD8+ cell fractions in the CD45R0-EF from both allergic and non-allergic subjects
in paper II. Plotted on the right axis is the ratio between CD4+ and CD8+, for both subject groups.
thiosulphate. **: p < 0.01. Significances were calculated using Spearman’s test.
GSTS: Gold sodium thiosulphate.
In the CD45RA-EF from the allergic subjects, the minute CD3+CD45R0+ cell
fraction decreased significantly (p < 0.05) with GSTS exposure (0.9 % at 0.0 µg/ml - 0.1
% at 50 µg/ml GSTS) (data not shown). The fraction of CD3+CD45R0+ cells remained
unchanged regardless of GSTS dose (0.0 - 50.0 µg/ml) in the CD45R0-EF from allergic
subjects (47.4 - 56.0 %) and the CD45RA-EF (0.2 - 4.5 %) and CD45R0-EF (74.8 - 78.9
%) from the non-allergic subjects (data not shown). The fraction of CD3+CD45RA+ cells
remained unchanged in response to GSTS in the CD45RA-EF (89.4 - 90.9 %) and
allergic subjects and in the CD45RA-EF (91.4 - 94.1
CD45R0-EF (2.8 - 7.7 %) from the allergic
42
%) and CD45R0-EF (1.8 - 9.3 %) from the non-allergic subject group (data not shown).
Figure 10. CD45RA+, CD45R0+ and double positive CD45RA+CD45R0+ cell fractions in PBMC from
non-allergic subjects in paper II. Plotted on the right axis is the ratio between CD45RA+ and CD45R0+
cell fractions. GSTS: Gold sodium thiosulphate. *: p < 0.05. $: Significant linearity, p < 0.05.
Significances were calculated using Friedman’s test.
CD3+CD45RA+CD45R0+ double positive cell fraction
The
CD45RA-EF
from
both
subject
groups
had
a
small
fraction
of
CD3+CD45RA+CD45R0+ double positive cells after culturing, which remained
unchanged (4.1 - 10.4 %) after GSTS exposure. In the CD45R0-EF from both the
allergic and non-allergic subjects, the fraction of CD45RA+CD45R0+ cells increased
after GSTS exposure, which was significant for the CD3+CD4+CD45RA+CD45R0+ cells
from the allergic subjects (p < 0.01 between GSTS concentrations 0.0 and 50.0 µg/ml)
(Table 4).
43
Table 4. CD45RA+, CD45R0+ and CD45RA+CD45R0+ cells in the CD45R0-EF from allergic and nonallergic subjects.
Allergic CD45R0-EF
0.0 µg/mla 25.0 µg/mla 50.0 µg/mla
CD3+CD4+CD45RA+CD45R0+ 22.4 ± 23.2 26.2 ± 20.8 30.7 ± 20.2**
2.2 ± 1.1 5.7 ± 3.6 3.7 ± 3.2
CD3+CD4+CD45RA+
+
+
+
68.6
CD3 CD4 CD45R0
± 28.7 60.8 ± 22.6 60.9 ± 23.0
Non-allergic CD45R0-EF
0.0 µg/mla 25.0 µg/mla 50.0 µg/mla
CD3+CD4+CD45RA+CD45R0+ 9.4 ± 11.3 10.1 ± 7.1 10.9 ± 6.9
1.2 ± 1.1 2.8 ± 2.5 0.5 ± 0.5
CD3+CD4+CD45RA+
+
+
+
80.6 ± 13.4 67.8 ± 7.3 61.1 ± 22.5
CD3 CD4 CD45R0
**: p < 0.01 from CD3+CD4+CD45RA+CD45R0+ from allergic subjects at GSTS concentration 0.0
µg/ml, calculated using Friedmans repeated measurement ANOVA test. a: GSTS concentration. GSTS:
Gold sodium thiosulphate.
The fraction of CD3+CD45RA+CD45R0+ cells was larger in the CD45R0-EF (14.7 23.2 %) than in the CD45RA-EF (4.1 - 5.7 %) from the non-allergic subjects (the
difference was significant at GSTS concentration 50.0 µg/ml, p < 0.05). The same
relationship between the CD45R0-EF (38.5 - 49.3 %) and CD45RA-EF (8.2 - 10.4 %)
was evident for the allergic subjects, but here the differences were not significant. The
CD3+CD8+CD45RA+CD45R0+ cell fraction remained unchanged in the CD45RA-EF
and CD45R0-EF from both the allergic and non-allergic subject groups (data not
shown).
In the PBMC fraction from non-allergic subjects, the CD3+CD45RA+CD45R0+ cell
fraction remained unchanged (3.5 - 7.1 %) regardless of GSTS dose (0.0 – 200.0 µg/ml,
fig. 10).
CLA expression
CLA was not expressed on unstimulated CD3+CD45RA+ cells (mean fluorescence
44
intensity, MFI, 0 – 301), which did not change with GSTS exposure (fig. 11). The
expression of CLA was significantly higher in the CD45R0-EF than in the CD45RA-EF
from both allergic and non-allergic subjects in the GSTS dose range 0.0 - 50.0 µg/ml (p
< 0.05, data not shown). There was a dose-dependent down-regulation of CLA
expression in the CD45R0-EF from non-allergic subjects in response to GSTS exposure,
which was significant for the CD3+CLA+ (r2 = 0.46, p < 0.05) and CD3+CD4+CLA+ (r2 =
0.6, p < 0.05) (fig. 11). The same trend could be seen for CD3+CD8+CLA+, but was not
significant (data not shown).
Figure 11. CLA expression on CD45RA-EF and CD45R0-EF cells from both allergic and non-allergic
subjects in paper II. GSTS: Gold sodium thiosulphate. CLA: Cutaneous Lymphocyte-associated
Antigen. MFI: Mean fluorescence intensity. **: p < 0.01. Significances were calculated using
Spearman’s test.
The CD45R0-EF from allergic subjects behaved somewhat differently regarding CLA
expression. The CLA expression in the CD45R0-EF from allergic subjects remained
unchanged at GSTS concentration 25.0 µg/ml compared to unexposed cells, but was
45
significantly decreased at GSTS concentration 50.0 µg/ml (p < 0.01) (fig. 11).
Chemokine receptor-expressing cells
Of the CD3+ cells, 1.6 – 46.6 % in the CD45RA-EF and 36.3 – 58.4 % in the
CD45R0-EF from both allergic and non-allergic subjects expressed the CXCR3 receptor,
but no significant differences were found between the CD45RA-EF and CD45R0-EF
from the allergic or the non-allergic subject groups, or between the subject groups, for
CXCR3. The expression was also not affected by GSTS exposure.
For CCR10, there was a weak trend of increasing CD3+CCR10+ cells after GSTS
exposure in the CD45RA-EF and CD45R0-EF from both the allergic and non-allergic
subjects (fig. 12A). A minimum of 3 % of the cells showed CCR10 without GSTS, to a
maximum of 25 % of the CD3+ cells expressing this receptor at 50.0 µg/ml GSTS in
both subject groups. This trend did not, however, reach statistical significance.
The mean fraction of CD3+CCR4+ cells was visibly higher in the CD45R0-EF than in
the CD45RA-EF in both allergic and non-allergic subjects (fig. 12B), but the difference
was only significant in the allergic subjects (p < 0.05). The fraction of CD3+CCR4+ cells
in the CD45R0-EF from both subject groups was unaffected by the GSTS exposure. In
contrast, there was a trend towards increased CD3+CCR4+ cell fractions after GSTS
stimulation in the CD45RA-EF from both allergic and non-allergic subjects, but the
dose-response relationship was only significant for the non-allergic subjects (r2 = 0.48, p
< 0.05).
46
47
Figure 12. Chemokine receptor-expressing cells in the CD45RA-EF and CD45R0-EF from both allergic and non-allergic subjects
in paper II. A shows CCR10, and B shows CCR4. GSTS: Gold sodium thiosulphate. *: p < 0.05. Significances were calculated
using Kruskal-Wallis test.
Discussion
Many studies have investigated the toxicology of different gold salts in vivo, both in
animals and in humans (98-101), but few studies have reported the in vitro effects of
gold salts. Our findings show that GSTS has a cytotoxic effect on lymphocytes in
concentrations higher than 50.0 µg/ml, (102 µM). Approximately 40 % (40.8 µM) of the
salt consists of Au [I]. RA patients receiving either gold sodium thiomalate (GSTM) or
auranofin, the oral gold salt treatment, obtain blood levels ranging between 0.1 – 0.4
µg/ml when in steady state (57, 59, 102), which for GSTM equals 0.13 - 0.51 µM active
Au [I], and for Auranofin equal 0.045 - 0.18 µM Au [I]. These concentrations are more
than a 100-fold less than the concentrations found to be toxic in the in vitro study in
paper II. To compare with mercuric chloride HgCl2, a highly toxic metal salt, toxic in
vitro levels range from 1-20 µM (0.74 - 14.8 µM pure Hg) (reviewed in (103)), while
NiCl2 levels of up to 1 mM (0.45 µM pure Ni) has been proven non-toxic in vitro (104).
Auranofin has proven to be toxic in the 0.3 - 3 µM (active Au [I]) range in vitro, but
many other gold salts have been regarded as virtually non-toxic in vitro (105). The
differences in toxicity might be explained by different properties of the molecule
carrying the gold ion, i.e. that different structures release the gold at different rates,
leaving different concentrations of available gold in the culture medium.
Furthermore, the in vitro environment is limited in simulating the in vivo conditions,
where individual differences in carrier-protein levels (such as albumin and globulins for
gold) can contribute. Individual properties of monocyte lysosomal enzymes influence
the oxidation rate of the Au [I] salt into the more reactive oxidizer Au [III], which also
affects the concentration at which different gold salts cause toxic effects.
We have shown that on a group level, LTT can be used to distinguish between
subjects allergic (EPI+) and non-allergic (EPI-) to gold. In paper I we used SI cut-off 7.9
48
to gain maximal sensitivity and specificity of 54.5 % and 92.9 %, respectively. These
results are not completely in agreement with an older study showing a sensitivity of 70
% and a specificity of 58 %, but there another cut-off (2.0), and different GSTS
concentrations were used (90). Many publications have used cut-off values of 2-3 when
calculating sensitivity and specificity for LTT (90, 106-108), but since this is just an
arbitrary value, there is no golden standard for this.
Using the lower GSTS concentration in paper I (6.25 µg/ml), yielded an accuracy of
67.5 %, a sensitivity of 54.5 % and a specificity of 78.5 % (cut-off 1.97). It has
previously been shown with NiSO4 that higher concentrations in test culture results in an
unspecific activation of T-cells, not unlike mitogens (109). To our knowledge, no similar
results have been reported for gold. Our results show the largest difference in SI between
allergic and non-allergic subjects at a high GSTS concentration. Therefore, we suggest
that the GSTS used in paper I did not evoke any unspecific proliferation.
When looking at the LTT results in paper II, we saw that both CD3+CD45RA+ and
CD3+CD45R0+ cells from the allergic subjects proliferated in response to GSTS, with
maximal mean SI values of 8.0 for the CD45RA-EF and 3.3 for the CD45R0-EF. In this
study only one SI value in the separated cell fractions reached above the 7.9 cut-off
limit, but it is not surprising that the separated cells might proliferate at a different rate
than a complete lymphocyte population.
The SI values for the unseparated PBMC cell fractions from the non-allergic subjects
proliferated at a rate clearly below the 7.9 limit. All GSTS exposed, separated cells from
the non-allergic subjects had SI below 1.0, indicating a suppressive effect of GSTS. As
to why both the CD45RA-EF and CD45R0-EF from the allergic subjects proliferated,
we can only speculate. It is however plausible to hypothesise that the CD45R0 cells
included most of the regulatory T-cells as well (22), leaving the CD45RA-EF without a
suppressing cell cohort.
Even though the LTT method could predict the EPI-IR group as non allergic with
49
rather high accuracy (87.5%), there was no significant difference between this subject
group and the group with positive patch test in paper I. The p-value was, however, very
close to significant (p = 0.059, data not shown). Taken together with the non-significant
p-value between the EPI- and the EPI-IR groups (p = 1, data not shown), it can be
postulated that the EPI-IR group is more similar to the EPI- group than to the EPI+
group. To our knowledge, this has not been tested before. The observation opens the
possibility for LTT to be used as a complement to patch testing where the morphological
outcome has been uncertain. Confirmation of negativity could be equally as valuable as
confirmation of positivity
To evaluate which cell types had proliferated, we examined the cell cultures in paper
II with flow cytometry. We saw that neither the CD45RA-EF nor CD45R0-EF cultures
from the allergic subjects changed their CD3+ cell fractions in response to the GSTS
exposure. The discrepancy between the LTT and flow cytometry might result from the
two methods measuring two different aspects of cell proliferation. LTT provides a view
of the actual proliferation during the 4 - 5 hours of labelled thymidin incorporation after
4 - 5 days of culturing, while flow cytometry shows the accumulated proliferation after 4
- 5 days of culture, including the net effect of cell proliferation and death. The reason
that the CD3+ cell fractions did not change in the flow cytometry analysis might thus be
due to a balance between cell death and cell proliferation.
In the CD45R0-EF from both allergic and non-allergic subjects, the ratio between the
CD3+CD4+ and CD3+CD8+ cells increased in a GSTS-dose-dependent manner. This
might be due to either an increase in CD3+CD4+ cell number, or a decrease in
CD3+CD8+ cell number, or a combination of both. Some studies indicate CD3+CD4+
cells as the main culprit involved in ACD to various haptens (77, 80, 106), while others
state that both CD3+CD4+ and CD3+CD8+ cells work as effector cells in ACD to Ni, but
that non-allergic patients also express Ni-specific CD3+CD4+ T-cell clones (75, 79, 110,
50
111), but not CD3+CD8+ cells. We saw that the CD3+CD8+ cells did not react at all
when exposed to GSTS, suggesting that CD3+CD8+ proliferation might not be a general
phenomenon in ACD, but occurring specifically in Ni allergy, or that gold has additional
immunomodulatory mechanisms.
The cells that responded to GSTS were almost exclusively of a CD3+CD4+CD45R0+
phenotype originating from the allergic subjects, responding by changing their
expression to include both CD45RA and CD45R0. This can plausibly be interpreted as
being in a transition state, since it has been shown that the expression of different
CD45R isoforms on T-cells in vitro is cyclic rather than unidirectional (25-28), and that
reactivated CD45R0+ T-cells express CD45RA as well (112, 113).
CLA was almost exclusively expressed on CD3+CD45R0+ cells, equally distributed
among the CD3+CD4+ and the CD3+CD8+ cells. Both of the latter cell types from the
allergic subjects retained their expression of CLA at the lowest GSTS concentration
used, while the cells from the non-allergic subjects down-regulated their expression even
at the lowest GSTS dose. This is in keeping with what has been found regarding Ni
allergy, where several studies have shown that CLA+ cells are necessary for Ni-specific
proliferation (11, 80, 81, 83, 114-116). CD3+CD4+CLA+ and CD3+CD8+CLA+ levels are
increased after metal hapten stimulation in vitro, including AuCl4 (114), but this study
did not investigate memory status of the cells analysed. Since we saw no proliferation of
CD3+CD8+ cells in response to GSTS, we conclude that the CD3+CD4+CD45R0+CLA+
cells that are retained by GSTS exposure are the cells specific for gold allergy.
The chemokine receptor CCR4 seemed to be more expressed on CD3+CD45R0+ cells
than CD3+CD45RA+ cells, from both the allergic and non-allergic subjects, which did
not change with GSTS exposure. Ni-responsive CD3+CD4+CD45R0+CLA+ cells express
51
the chemokine receptors CCR4, CXCR3 and CCR10 (80, 117). CCR4 is normally coexpressed with CLA, and also directs cells to the skin (118, 119). Unfortunately, due to
technical circumstances, this receptor could not be co-analysed with CLA in our study
(paper II), but since a fairly large fraction of CD3+CD45R0+ cells expressed CCR4 (up
to 50 %, fig 12), it seems reasonable to hypothesize that a substantial fraction of these
cells expressed CLA as well.
CXCR3+ cells have been shown to be infiltrating skin patch tested with allergens, but
not irritants (118). In paper II, 40 – 60 % of all T-cells expressed this receptor, but we
found no differences between the allergic and non-allergic subjects. However, since we
were unable to co-analyse this receptor with CD4 and CD8 (also due to technical
circumstances), we can not be certain that this is not due to a balance between
CD3+CD4+ cell proliferation and CD3+CD8+ cell death, similar to the CD3+ cell results.
We saw a trend towards an increase of CD3+CCR10+ cells after GSTS exposure in all
separated cell fractions from both subject groups in paper I, but the increase was not
significant. The trend supports what has previously been reported for Ni (80, 117),
namely that CCR10 is mostly associated with skin homing (119), and CCR10expressing cells have been associated with patch tested skin even a long time after Ni
exposure (117, 119).
Previous studies using PBMC from gold-treated arthritic patients reported a decrease
in mitogen-induced IFN-γ secretion (120) after gold salt exposure. However, another
study using blood samples from gold-allergic subjects indicated an increased secretion
of IFN-γ by gold salt-exposed lymphocytes (121). In the allergic subjects in paper I,
IFN-γ levels were found to be elevated, which tallies with previous suggestions that
ACD is mainly a Th1 response (37, 122, 123). IFN-γ detection discriminates the allergic
subject group from both the negative and the irritant group, with a sensitivity and
52
specificity of 83.8 % and 81.8 %, respectively. Vamnes et al (121) showed maximum
sensitivity 89 % and specificity 73 % of IFN-γ as assessment method after 4 days of cell
culturing, but it is possible that cell culturing for 5 days could have increased the
sensitivity and specificity in that study. Assessment of IFN-γ in paper I was also able to
correctly identify 87.5 % of the EPI-IR subjects as non-allergic, which is the highest
discriminatory value obtained in this study for EPI-IR.
In paper I, a significant increase was found in the IL-13 secretion in the EPI+ subjects
compared to the other two subject groups. IL-13 has been shown to be increased in
blood cultures from Ni-allergic patients when exposed to Ni2+ (124). One theory is that
the elicitation phase of ACD is mainly maintained by a Th1 response, while the
containment and inhibition of the reaction is attained by Th2 or Treg cytokines such as
IL-4, IL-5 or IL-10 (36, 75, 79). This might explain the increased secretion in the
allergic subjects in the present study. The IL-13 assay was quite good at diagnosing
ACD to gold, with a sensitivity and specificity of 78.8 % and 71.4 % respectively, but
this was not quite as effective as the IFN-γ assay.
IL-2 is a cytokine primarily associated with Th1 responses, causing antigen-specific
proliferation in memory T-cells, and is a key driver in T-cell proliferation (125). The
findings in paper I of elevated IL-2 levels in allergic subjects were in concordance with
the concept that gold exposure on memory lymphocytes causes specific proliferation,
which is also reflected in the correlation with the LTT SI values. The IL-2 levels were
significantly higher in the EPI+ group than in both the EPI- and EPI-IR groups, which
points to a specific reactivity towards gold. Previous studies have shown that different
gold salts decrease secretion of IL-2 in both blood samples from arthritic patients and in
normal blood cell lines (126, 127). However, none of these studies included patch tested
patients or patients with adverse effects to treatment, so it is possible that none of these
patients were allergic.
The sensitivity and specificity for IL-2 measurement in diagnosing gold allergy were
53
both quite high, but not as high as for IFN-γ or IL-13. They are similar to the values of
LTT alone, and there was a significant correlation to the LTT SI values.
IL-10 is a cytokine that has mainly immunosuppressant properties, and functions by
downregulating expression of cytokines and co-stimulatory molecules (128). Some
studies show that IL-10 secretion is increased upon epicutaneous allergen stimulation,
which in turn downregulates Th1 cytokines, thereby limiting the immune reaction (59).
One study showed that in Ni allergy, IL-10 production was increased in the allergic
patients’ PBMC’s in vitro (106). Interestingly, in we found no significant differences
between any of the subject groups, suggesting that Ni induces IL-10 secretion in a
manner that gold does not.
One interesting find is that the cut-offs for all three cytokines are low, for IFN-γ and
IL-13 it was 0.0 pg/ml, and for IL-2 3.41 pg/ml. Also, many of the net values are
negative, mostly in the EPI- and the EPI-IR groups. However, since gold is known to
have suppressive effects on T-cells, then it is to be expected that without gold-reactive Tcells, which should be the case in the non-allergic subjects, there will be an inhibition of
cytokine production after gold exposure. Since the cells can be disturbed, and thereby
slightly activated, by the purification procedure, as well as from being in an in vitro
environment, the cultures without GSTS will secrete a base level of cytokines; thus the
GSTS-exposed cultures from the non-allergic subjects turn out with a negative net value.
In the cultures from the allergic subjects, the specific activated T-cells secrete enough
cytokines to compensate for the inhibitory effect on the non-specific T-cells; therefore
the net values from the allergic subjects come close to 0. High accuracy in testing can
thus be achieved due to the pharmacologically inhibitory effect of gold on T-cells in
non-allergic subjects.
54
Th1 and Th2 cytokines are known to inhibit one another (129), which might explain
why the maximum sensitivities and specificities are achieved at different GSTS
concentrations and different days for the different cytokines. To evaluate whether Th1 or
Th2 cytokines were most prominent in ACD to gold, correlations between the different
cytokines were calculated. There was a high degree of correlations between all
cytokines, with the highest found between IL-13 and IFN-γ. Possibly, the early T-cell
response is to secrete Th1 cytokines such as IFN-γ and IL-2, which also correlates well
with IL-13. To contain and stop the reaction, other T-cells not specific for gold allergy
then respond by producing IL-13 to inhibit the immunological response. If the cytokine
assay had been performed at closer time intervals and/or for a longer time, an increase in
IL-13 might have been detected, with a subsequent decline in IFN-γ and IL-2
production.
To evaluate whether any or all of the in vitro methods could be combined to increase
the accuracy of diagnosis, logistic regression was performed. First, correlations between
the different cytokines and LTT were calculated, with the hypothesis that if the cytokines
correlated well to LTT, they might not provide any improvement for diagnostic accuracy.
The cytokines correlating the least to LTT (which turned out to be IL-10) would then
yield a higher accuracy when included in the logistic regression calculation. The
approach that yielded the highest accuracy did not include IL-10, however, but rather
consisted of LTT, IFN-γ and IL-13. This yielded an accuracy of 80.5 %, which was very
close to the one achieved with only IFN-γ, 83.1 %.
Another aspect to consider is that of cost-benefit. One might consider the use of IFNγ detection as a single diagnostic tool, using a simple ELISA method instead of the
rather costly Luminex assay. Removing LTT from the procedure would also remove the
55
need for radioactive materials, and reduce number of culture plates. The IFN-γ
assessment could then be performed by any routine diagnostic laboratory. This method
could preferably be used to verify irritant epicutaneous patch test reaction in conjunction
with, or as an alternative to, repeated patch tests with serial dilution of antigens.
Conclusions
When we compared our findings to what has been published on Ni, we found that the
main similarity to gold allergy was that the T-cells from allergic individuals, when
proliferating in response to relevant metal salt, are of the CD3+CD4+CD45R0+CLA+
phenotype. In contrast to Ni allergy, however, the chemokine receptors CCR4, CXCR3
and CCR10 were not triggered in gold allergic subjects in response to GSTS in vitro. But
since the clinical outcomes of these two allergies differ significantly, different
mechanisms of action may perhaps be expected.
It is also very possible that we would be able to discern differences if we collected
cells at different time points in the development of ACD, and followed them over an
extended time period. When culturing cells it is always difficult to accurately pinpoint
the timing of protein expression and secretion.
Our findings in paper I indicate that both Th1 and Th2 cells are involved in the
mechanisms of ACD to gold. This is in keeping with some publications on Ni (82),
while others state that it is mostly Th1 cells that are involved in the Ni reaction (82,
130). Thus, this might be another reason why the clinical outcome for Ni allergy and
gold allergy are so different.
We also suggest that a blood test followed by IFN-γ assessment with a simple ELISA
assay could be used as a complement to patch testing, especially to rule out an IR. This
could make the diagnostic process easier for both patient and physician.
In summary, contact allergy to gold seems to involve mainly memory CD4+CLA+ T56
cells, of both Th1 and Th2 type. Further studies are warranted, to examine whether
different cell subsets are in effect at different time points, and whether other allergens
compare to Ni or to gold. The differences between Ni and gold allergy, particularly
regarding the receptors guiding T-cells towards the skin, could help explain the different
clinical outcomes of the different allergens. Possibly this could also be extended to other
allergens in the future, helping to explain the different allergenicity of different haptens.
57
Acknowledgements
I would like to thank my supervisor, professor Per Hultman, for giving me the
opportunity to make this project. Since I began my university studies, I have
always wanted to work in the immunology field, so this was the perfect chance
for me. Thank you so much for inspiring me and always being there to answer
questions, sometimes even in the middle of the night. Thanks also to my cosupervisors Karin Cederbrant and Chris Anderson. You’ve both helped me a
lot, and you’ve really stepped up to the plate during the last difficult months.
Thank you also to Said Havarinasab, Christer Bergman and Marie-Louise
Eskilsson, who always help out with everything you can, whether it be putting
up shelves or helping me with technical stuff.
I would also like to thank dr Klara Martinsson, my office-buddy and shoefriend. You make it fun to come to the office, and thank you for introducing
me to “pralin-kvällar” and pyssel! Thank you also to Jenny Mjösberg, who is
the greatest discussion partner on lab-related and non-lab-related things, and
also the best hairdresser in the world! If your research should unexpectedly
turn sour, you know you can always fall back on that. Thank you also to Marie
Rubér, who introduced me to my favourite hobby: Knitting! You also helped
me so much when I first began at AIR with my very first Luminex assay!
Thanks also to Jimmy Ekstrand, for always being so positive and willing to
discuss anything both research and everything else. We sure miss you at the
office when you’re away in Umeå!
Thanks also to all present and past, co-workers at AIR, none mentioned and
none forgotten! I have felt welcome from the beginning, and it’s always easy to
find someone to ask if I wonder something. It seems we have experts on almost
everything in our department.
Thanks also to my co-writers at Örebro University, Gunilla Färm and Ruth
Eid-Forest. You helped a great deal with patient recruiting and data
interpretation. Also thanks to Inga-Lill Erikssohn for helping with interpreting
patient journals.
I also want to thank Kristina Karlsson, who was the one who started the project
and made significant laboratory work for the first paper. And thanks to Barbro
58
Gunnarsson, who has gathered all patients in Linköping and organized all
patient data.
Thanks also to the statistician at Linköping University, Olle Eriksson. You
helped me so much, and I am so grateful that you even made some of the
analyses when you were on paternity leave.
Thank you also to all my friends who don’t work with me: Christine, Martin &
the boys, Jonas, Anders, Fredrik, Martin & Gunilla, Marcus, Micke, Mackan &
Micke and Elna. Thank you for taking my mind off research for a while, and
always being supportive and helpful. You’ve all really helped me through this
long and winding process and helped me find the light at the end of the tunnel
when I sometimes felt like I had lost the way. I love you all!
Thanks also to my family, who although they don’t have a clue of what I’m
working on, always support me and seem proud of me. Thank you so much,
mom, dad, Sanna, mormor & Micael, and morfar. I couldn’t have done it
without you.
Also, thanks to my biggest stress-reliever, Hobbe. When you curl up in my lap,
everything feels a little better. I just wish your brother was still around to keep
us company.
Finally, thank you Thomas, my wonderful husband. Thank you for always
being there and picking up the slack when I have intensive periods where I
don’t have time to clean and do laundry. Thank you for loving me and taking
care of me and Hobbe. I love you so much.
59
References
1
Romagnani S. Regulation of the T cell response. Clin Exp Allergy 2006: 36: 1357-66.
2
Starr T K, Jameson S C, Hogquist K A. Positive and negative selection of T cells. Annu Rev
Immunol 2003: 21: 139-76.
3
Blander J M. Phagocytosis and antigen presentation: a partnership initiated by Toll-like
receptors. Ann Rheum Dis 2008: 67 Suppl 3: iii44-9.
4
Iwasaki A, Medzhitov R. Toll-like receptor control of the adaptive immune responses. Nat
Immunol 2004: 5: 987-95.
5
Janeway C A, Travers P, Walport M, Shlomchik M. Immunobiology, 5 edn. New york
London, Garland Science, 2001.
6
Aderem A, Underhill D M. Mechanisms of phagocytosis in macrophages. Annu Rev Immunol
1999: 17: 593-623.
7
Morrissette N, Gold E, Aderem A. The macrophage--a cell for all seasons. Trends Cell Biol
1999: 9: 199-201.
8
Cavaillon J M. Cytokines and macrophages. Biomed Pharmacother 1994: 48: 445-53.
9
Ebert L M, Schaerli P, Moser B. Chemokine-mediated control of T cell traffic in lymphoid and
peripheral tissues. Mol Immunol 2005: 42: 799-809.
10
Schaerli P, Moser B. Chemokines: control of primary and memory T-cell traffic. Immunol Res
2005: 31: 57-74.
11
Santamaria-Babi L F. Skin-homing T cells in cutaneous allergic inflammation. Chem Immunol
Allergy 2006: 91: 87-97.
12
Ainslie M P, Mcnulty C A, Huynh T, Symon F A, Wardlaw a J. Characterisation of adhesion
receptors mediating lymphocyte adhesion to bronchial endothelium provides evidence for a
distinct lung homing pathway. Thorax 2002: 57: 1054-9.
13
Agace W W. T-cell recruitment to the intestinal mucosa. Trends Immunol 2008: 29: 514-22.
14
Mosmann T R, Coffman R L. TH1 and TH2 cells: different patterns of lymphokine secretion
lead to different functional properties. Annu Rev Immunol 1989: 7: 145-73.
15
Romagnani S. Type 1 T helper and type 2 T helper cells: functions, regulation and role in
protection and disease. Int J Clin Lab Res 1991: 21: 152-8.
16
Sallusto F, Lanzavecchia A, Mackay C R. Chemokines and chemokine receptors in T-cell
priming and Th1/Th2-mediated responses. Immunol Today 1998: 19: 568-74.
17
Abbas a K, Murphy K M, Sher A. Functional diversity of helper T lymphocytes. Nature 1996:
383: 787-93.
18
Hsieh C S, Macatonia S E, Tripp C S, Wolf S F, O'garra A, Murphy K M. Development of TH1
CD4+ T cells through IL-12 produced by Listeria-induced macrophages. Science 1993: 260:
547-9.
19
Chavez-Galan L, Arenas-Del Angel M C, Zenteno E, Chavez R, Lascurain R. Cell death
mechanisms induced by cytotoxic lymphocytes. Cell Mol Immunol 2009: 6: 15-25.
60
20
Brombacher F. The role of interleukin-13 in infectious diseases and allergy. Bioessays 2000: 22:
646-56.
21
Romagnani S. Cytokines and chemoattractants in allergic inflammation. Mol Immunol 2002:
38: 881-5.
22
Ozdemir C, Akdis M, Akdis C A. T regulatory cells and their counterparts: masters of immune
regulation. Clin Exp Allergy 2009: 39: 626-39.
23
Korn T, Bettelli E, Oukka M, Kuchroo V K. IL-17 and Th17 Cells. Annu Rev Immunol 2009:
27: 485-517.
24
Ye P, Rodriguez F H, Kanaly S, Stocking K L, Schurr J, Schwarzenberger P, Oliver P, Huang W,
Zhang P, Zhang J, Shellito J E, Bagby G J, Nelson S, Charrier K, Peschon J J, Kolls J K.
Requirement of interleukin 17 receptor signaling for lung CXC chemokine and granulocyte
colony-stimulating factor expression, neutrophil recruitment, and host defense. J Exp Med
2001: 194: 519-27.
25
Bell E B. Function of CD4 T cell subsets in vivo: expression of CD45R isoforms. Semin
Immunol 1992: 4: 43-50.
26
Beverley P C, Daser A, Michie C A, Wallace D L. Functional subsets of T cells defined by
isoforms of CD45. Biochem Soc Trans 1992: 20: 184-7.
27
Bell E B, Yang C P, Sarawar S R, Sparshott S M. The cyclic expression of CD45R isoforms on
CD4 T cells. Biochem Soc Trans 1992: 20: 198-202.
28
Rothstein D M, Yamada A, Schlossman S F, Morimoto C. Cyclic regulation of CD45 isoform
expression in a long term human CD4+CD45RA+ T cell line. J Immunol 1991: 146: 1175-83.
29
Gell P G H, Coombs R a A. Clinical Aspects of Immunology, 2 edn., Blackwell Science Ltd,
1963.
30
Averbeck M, Gebhardt C, Emmrich F, Treudler R, Simon J C. Immunologic principles of
allergic disease. J Dtsch Dermatol Ges 2007: 5: 1015-28.
31
Cousin F, Philips K, Favier B, Bienvenu J, Nicolas J F. Drug-induced urticaria. Eur J Dermatol
2001: 11: 181-7.
32
Dixon F J, Cochrane C G. The pathogenicity of antigen-antibody complexes. Pathol Annu
1970: 5: 355-79.
33
Black C A. Delayed type hypersensitivity: current theories with an historic perspective.
Dermatol Online J 1999: 5: 7.
34
Budinger L, Hertl M. Immunologic mechanisms in hypersensitivity reactions to metal ions: an
overview. Allergy 2000: 55: 108-15.
35
Cavani A. Immune regulatory mechanisms in allergic contact dermatitis and contact
sensitization. Chem Immunol Allergy 2008: 94: 93-100.
36
Girolomoni G, Gisondi P, Ottaviani C, Cavani A. Immunoregulation of allergic contact
dermatitis. J Dermatol 2004: 31: 264-70.
37
Kapsenberg M L, Bos J D, Wierenga E A. T cells in allergic responses to haptens and proteins.
Springer Semin Immunopathol 1992: 13: 303-14.
38
Martin S F. T lymphocyte-mediated immune responses to chemical haptens and metal ions:
61
implications for allergic and autoimmune disease. Int Arch Allergy Immunol 2004: 134: 186-98.
39
Sinigaglia F. The molecular basis of metal recognition by T cells. J Invest Dermatol 1994: 102:
398-401.
40
Schnyder B, Pichler W J. Mechanisms of drug-induced allergy. Mayo Clin Proc 2009: 84: 26872.
41
Pichler W J. Modes of presentation of chemical neoantigens to the immune system. Toxicology
2002: 181-182: 49-54.
42
Bos J D, Teunissen M B, Kapsenberg M L. Immunology of contact dermatitis. Acta Derm
Venereol Suppl (Stockh) 1989: 151: 84-7; discussion 106-10.
43
Grabbe S, Schwarz T. Immunoregulatory mechanisms involved in elicitation of allergic contact
hypersensitivity. Immunol Today 1998: 19: 37-44.
44
Sebastiani S, Albanesi C, De P O, Puddu P, Cavani A, Girolomoni G. The role of chemokines in
allergic contact dermatitis. Arch Dermatol Res 2002: 293: 552-9.
45
Gober M D, Gaspari a A. Allergic contact dermatitis. Curr Dir Autoimmun 2008: 10: 1-26.
46
Gober M D, Fishelevich R, Zhao Y, Unutmaz D, Gaspari a A. Human natural killer T cells
infiltrate into the skin at elicitation sites of allergic contact dermatitis. J Invest Dermatol 2008:
128: 1460-9.
47
Cavani A. T regulatory cells in contact hypersensitivity. Curr Opin Allergy Clin Immunol 2008:
8: 294-8.
48
Beck M H, Wilkonson S M. Contact Dermatitis: Allergic. In: Rook's Textbook of Dermatology,
6 edn, T Burns, S Breathnach, N Cox and C Griffiths (ed)^(eds): Oxford, Blackwell Scientific
Publications, 2004.
49
Edman B. Sites of contact dermatitis in relationship to particular allergens. Contact Dermatitis
1985: 13: 129-35.
50
Thyssen J P, Johansen J D, Carlsen B C, Menne T. Prevalence of nickel and cobalt allergy
among female patients with dermatitis before and after Danish government regulation: A 23year retrospective study. J Am Acad Dermatol 2009.
51
De Groot a C, White I R. Cosmetics and skin care products. In: Textbook of Contact Dermatitis,
3 edn, R J G Rycroft, T Menné, P J Frosch and J-P Lepoittevin (ed)^(eds): Berlin, Springer,
2001: 661-685.
52
Smit H A, Burdorf A, Coenraads P J. Prevalence of hand dermatitis in different occupations. Int
J Epidemiol 1993: 22: 288-93.
53
Fowler J, Jr., Taylor J, Storrs F, Sherertz E, Rietschel R, Pratt M, Mathias C G, Marks J,
Maibach H, Fransway A, Deleo V, Belsito D. Gold allergy in North America. Am J Contact
Dermat 2001: 12: 3-5.
54
Hostynek J J. Gold: an allergen of growing significance. Food Chem Toxicol 1997: 35: 839-44.
55
Merchant B. Gold, the noble metal and the paradoxes of its toxicology. Biologicals 1998: 26:
49-59.
56
Ahlgren C, Ahnlide I, Bjorkner B, Bruze M, Liedholm R, Moller H, Nilner K. Contact allergy
to gold is correlated to dental gold. Acta Derm Venereol 2002: 82: 41-4.
62
57
Ahnlide I, Ahlgren C, Bjorkner B, Bruze M, Lundh T, Moller H, Nilner K, Schutz A. Gold
concentration in blood in relation to the number of gold restorations and contact allergy to gold.
Acta Odontol Scand 2002: 60: 301-5.
58
Mallo Perez L, Diaz Donado C. Intraoral contact allergy to materials used in dental practice. A
critical review. Med Oral 2003: 8: 334-47.
59
Ekqvist S, Svedman C, Lundh T, Moller H, Bjork J, Bruze M. A correlation found between gold
concentration in blood and patch test reactions in patients with coronary stents. Contact
Dermatitis 2008: 59: 137-42.
60
Ekqvist S, Svedman C, Moller H, Kehler M, Pripp C M, Bjork J, Gruvberger B, Holmstrom E,
Gustavsson C G, Bruze M. High frequency of contact allergy to gold in patients with
endovascular coronary stents. Br J Dermatol 2007: 157: 730-8.
61
Ekqvist S. Clinical and Experimental Studies of Contact Allergy to Stent Metals. PhD.
Occupational and Environmental Dermatology Lund University 2008. Malmö.
62
Schuppe H C, Ronnau a C, Von Schmiedeberg S, Ruzicka T, Gleichmann E, Griem P.
Immunomodulation by heavy metal compounds. Clin Dermatol 1998: 16: 149-57.
63
Kean W F, Forestier F, Kassam Y, Buchanan W W, Rooney P J. The history of gold therapy in
rheumatoid disease. Semin Arthritis Rheum 1985: 14: 180-6.
64
Panayi G S. Immunological and immune-mediated toxic effects of gold compounds used in the
treatment of Rheumatoid Arthritis. In: Immunotoxicity of Metals and Immunotoxicology, 1 edn,
A D Dayan, R F Hertel, E Heseltine, G Kazantzis, E M Smith and M T Van Der Venne
(ed)^(eds): New York, London, Plenum Press, 1990: 155-161.
65
Goebel C, Kubicka-Muranyi M, Tonn T, Gonzalez J, Gleichmann E. Phagocytes render
chemicals immunogenic: oxidation of gold(I) to the T cell-sensitizing gold(III) metabolite
generated by mononuclear phagocytes. Arch Toxicol 1995: 69: 450-9.
66
Shaw J L, Wolowska J, Collison D, Howard J A, Mcinnes E J, Mcmaster J, Blake a J, Wilson C,
Schroder M. Redox non-innocence of thioether macrocycles: elucidation of the electronic
structures of mononuclear complexes of gold(II) and silver(II). J Am Chem Soc 2006: 128:
13827-39.
67
Zetterstrom C K, Jiang W, Wahamaa H, Ostberg T, Aveberger a C, Schierbeck H, Lotze M T,
Andersson U, Pisetsky D S, Erlandsson Harris H. Pivotal advance: inhibition of HMGB1
nuclear translocation as a mechanism for the anti-rheumatic effects of gold sodium thiomalate. J
Leukoc Biol 2008: 83: 31-8.
68
Littman B H, Hall R E. Effects of gold sodium thiomalate on functional correlates of human
monocyte maturation. Arthritis Rheum 1985: 28: 1384-92.
69
Seitz M, Valbracht J, Quach J, Lotz M. Gold sodium thiomalate and chloroquine inhibit
cytokine production in monocytic THP-1 cells through distinct transcriptional and
posttranslational mechanisms. J Clin Immunol 2003: 23: 477-84.
70
Kumar Mangalam A, Aggarwal A, Naik S. Gold sodium thiomalate (GSTM) inhibits
lipopolysaccharide stimulated tumor necrosis factor-alpha through ceramide pathway. Cell
Immunol 2002: 219: 1-10.
71
Christiansen J, Farm G, Eid-Forest R, Anderson C, Cederbrant K, Hultman P. Interferon-gamma
secreted from peripheral blood mononuclear cells as a possible diagnostic marker for allergic
63
contact dermatitis to gold. Contact Dermatitis 2006: 55: 101-12.
72
Garner L A. Contact dermatitis to metals. Dermatol Ther 2004: 17: 321-7.
73
Moller H. Dental gold alloys and contact allergy. Contact Dermatitis 2002: 47: 63-6.
74
Nasorri F, Sebastiani S, Mariani V, De Pita O, Puddu P, Girolomoni G, Cavani A. Activation of
nickel-specific CD4+ T lymphocytes in the absence of professional antigen-presenting cells. J
Invest Dermatol 2002: 118: 172-9.
75
Saint-Mezard P, Berard F, Dubois B, Kaiserlian D, Nicolas J F. The role of CD4+ and CD8+ T
cells in contact hypersensitivity and allergic contact dermatitis. Eur J Dermatol 2004: 14: 1318.
76
Werfel T, Hentschel M, Kapp A, Renz H. Dichotomy of blood- and skin-derived IL-4-producing
allergen-specific T cells and restricted V beta repertoire in nickel-mediated contact dermatitis. J
Immunol 1997: 158: 2500-5.
77
Koga T, Imayama S, Hashizume T, Hori Y. Interferon-gamma and interleukin-2 production by
peripheral blood mononuclear cells from a patient with gold contact allergy. Br J Dermatol
1993: 128: 227-9.
78
Saint-Mezard P, Rosieres A, Krasteva M, Berard F, Dubois B, Kaiserlian D, Nicolas J F.
Allergic contact dermatitis. Eur J Dermatol 2004: 14: 284-95.
79
Watanabe H, Unger M, Tuvel B, Wang B, Sauder D N. Contact hypersensitivity: the mechanism
of immune responses and T cell balance. J Interferon Cytokine Res 2002: 22: 407-12.
80
Moed H, Boorsma D M, Stoof T J, Von Blomberg B M, Bruynzeel D P, Scheper R J, Gibbs S,
Rustemeyer T. Nickel-responding T cells are CD4+ CLA+ CD45RO+ and express chemokine
receptors CXCR3, CCR4 and CCR10. Br J Dermatol 2004: 151: 32-41.
81
Blanca M, Leyva L, Torres M J, Mayorga C, Cornejo-Garcia J, Antunez-Rodriguez C,
Santamaria L F, Juarez C. Memory to the hapten in non-immediate cutaneous allergic reactions
to betalactams resides in a lymphocyte subpopulation expressing both CD45RO and CLA
markers. Blood Cells Mol Dis 2003: 31: 75-9.
82
Kapsenberg M L, Wierenga E A, Stiekema F E, Tiggelman a M, Bos J D. Th1 lymphokine
production profiles of nickel-specific CD4+T-lymphocyte clones from nickel contact allergic
and non-allergic individuals. J Invest Dermatol 1992: 98: 59-63.
83
Lisby S, Hansen L H, Menn T, Baadsgaard O. Nickel-induced proliferation of both memory and
naive T cells in patch test-negative individuals. Clin Exp Immunol 1999: 117: 217-22.
84
Belsito D V. Patch testing: after 100 years, still the gold standard in diagnosing cutaneous
delayed-type hypersensitivity. Arb Paul Ehrlich Inst Bundesamt Sera Impfstoffe Frankf A M
1997: 195-202.
85
Belsito D V. Patch testing with a standard allergen ("screening") tray: rewards and risks.
Dermatol Ther 2004: 17: 231-9.
86
Fischer T. The art of patch testing. Contact Dermatitis 1990: 23: 221-3.
87
Hindsen M, Bruze M, Christensen O B. Individual variation in nickel patch test reactivity. Am J
Contact Dermat 1999: 10: 62-7.
88
Bruze M, Isaksson M, Edman B, Bjorkner B, Fregert S, Moller H. A study on expert reading of
patch test reactions: inter-individual accordance. Contact Dermatitis 1995: 32: 331-7.
64
89
Beltrani V S, Beltrani V P. Contact dermatitis. Ann Allergy Asthma Immunol 1997: 78: 160-73;
quiz 174-6.
90
Cederbrant K, Hultman P, Marcusson J A, Tibbling L. In vitro lymphocyte proliferation as
compared to patch test using gold, palladium and nickel. Int Arch Allergy Immunol 1997: 112:
212-7.
91
Silvennoinen-Kassinen S, Niinimaki A. Gold sensitivity blast transformation. Contact
Dermatitis 1984: 11: 156-8.
92
Denman E J, Denman a M. The lymphocyte transformation test and gold hypersensitivity. Ann
Rheum Dis 1968: 27: 582-9.
93
Romagnoli P, Spinas G A, Sinigaglia F. Gold-specific T cells in rheumatoid arthritis patients
treated with gold. J Clin Invest 1992: 89: 254-8.
94
Dearman R J, Warbrick E V, Skinner R, Kimber I. Cytokine fingerprinting of chemical
allergens: species comparisons and statistical analyses. Food Chem Toxicol 2002: 40: 1881-92.
95
Axell T, Bjorkner B, Fregert S, Niklasson B. Standard patch test series for screening of contact
allergy to dental materials. Contact Dermatitis 1983: 9: 82-4.
96
Lachapelle J M, Bruynzeel D P, Ducombs G, Hannuksela M, Ring J, White I R, Wilkinson J,
Fischer T, Billberg K. European multicenter study of the TRUE Test. Contact Dermatitis 1988:
19: 91-7.
97
Nordlind K, Liden S. In vitro lymphocyte reactivity to heavy metal salts in the diagnosis of oral
mucosal hypersensitivity to amalgam restorations. Br J Dermatol 1993: 128: 38-41.
98
Blodgett R C, Jr., Pietrusko R G. Long-term efficacy and safety of auranofin: a review of
clinical experience. Scand J Rheumatol Suppl 1986: 63: 67-78.
99
Payne B J, Arena E. The subacute and chronic toxicity of SK&F 36914 and SK&F D-39162 in
dogs. Vet Pathol Suppl 1978: 15: 9-12.
100
Payne B J, Arena E. The subacute and chronic toxicity of SK&F 36914, SK&F D-39162 and
gold sodium thiomalate in rats. Vet Pathol Suppl 1978: 15: 13-22.
101
Mirabelli C K, Johnson R K, Hill D T, Faucette L F, Girard G R, Kuo G Y, Sung C M, Crooke S
T. Correlation of the in vitro cytotoxic and in vivo antitumor activities of gold(I) coordination
complexes. J Med Chem 1986: 29: 218-23.
102
Gottlieb N L. Pharmacology of auranofin: overview and update. Scand J Rheumatol Suppl
1986: 63: 19-28.
103
Berlin M, Zalups K R, Fowler B F. Mercury. In: Handbook on the Toxicology of Metals, 3 edn,
G F Nordberg, B a Fowler, M Nordberg and L T Friberg (ed)^(eds), 2007: 675-729.
104
Davidson T, Salnikow K, Costa M. Hypoxia inducible factor-1 alpha-independent suppression
of aryl hydrocarbon receptor-regulated genes by nickel. Mol Pharmacol 2003: 64: 1485-93.
105
Crooke S T, Snyder R M. The cellular and molecular pharmacology of auranofin and related
gold complexes. Scand J Rheumatol Suppl 1986: 63: 1-18.
106
Cederbrant K, Anderson C, Andersson T, Marcusson-Stahl M, Hultman P. Cytokine production,
lymphocyte proliferation and T-cell receptor Vbeta expression in primary peripheral blood
mononuclear cell cultures from nickel-allergic individuals. Int Arch Allergy Immunol 2003: 132:
373-9.
65
107
Cederbrant K, Gunnarsson L G, Marcusson J A. Mercury intolerance and lymphocyte
transformation test with nickel sulfate, palladium chloride, mercuric chloride, and gold sodium
thiosulfate. Environ Res 2000: 84: 140-4.
108
Van Bever H P, Bridts C H, Moens M M, De Rijck T E, Mertens a V, De Clerck L S, Stevens W
J. Lymphocyte transformation test with house dust mite (Dermatophagoides pteronyssinus) in
normal children, asthmatic children and asthmatic children receiving hyposensitization. Clin
Exp Allergy 1993: 23: 661-8.
109
Al-Tawil N G, Marcusson J A, Moller E. Lymphocyte transformation test in patients with nickel
sensitivity: an aid to diagnosis. Acta Derm Venereol 1981: 61: 511-5.
110
Cavani A, Mei D, Guerra E, Corinti S, Giani M, Pirrotta L, Puddu P, Girolomoni G. Patients
with allergic contact dermatitis to nickel and nonallergic individuals display different nickelspecific T cell responses. Evidence for the presence of effector CD8+ and regulatory CD4+ T
cells. J Invest Dermatol 1998: 111: 621-8.
111
Xu H, Diiulio N A, Fairchild R L. T cell populations primed by hapten sensitization in contact
sensitivity are distinguished by polarized patterns of cytokine production: interferon gammaproducing (Tc1) effector CD8+ T cells and interleukin (Il) 4/Il-10-producing (Th2) negative
regulatory CD4+ T cells. J Exp Med 1996: 183: 1001-12.
112
Hoy M D, O'donnell J L, Hart D N. Dual CD45RA, CD45RO positive T-lymphocytes within
rheumatoid arthritic joints. Pathology 1993: 25: 167-73.
113
Young J L, Ramage J M, Gaston J S, Beverley P C. In vitro responses of human
CD45R0brightRA- and CD45R0-RAbright T cell subsets and their relationship to memory and
naive T cells. Eur J Immunol 1997: 27: 2383-90.
114
Nokiba K. [Immunological studies on the peripheral blood mononuclear cells in metal allergy
patients]. Kokubyo Gakkai Zasshi 2005: 72: 159-71.
115
Santamaria Babi L F, Picker L J, Perez Soler M T, Drzimalla K, Flohr P, Blaser K, Hauser C.
Circulating allergen-reactive T cells from patients with atopic dermatitis and allergic contact
dermatitis express the skin-selective homing receptor, the cutaneous lymphocyte-associated
antigen. J Exp Med 1995: 181: 1935-40.
116
Jensen C S, Lisby S, Larsen J K, Veien N K, Menne T. Characterization of lymphocyte
subpopulations and cytokine profiles in peripheral blood of nickel-sensitive individuals with
systemic contact dermatitis after oral nickel exposure. Contact Dermatitis 2004: 50: 31-8.
117
Moed H, Boorsma D M, Tensen C P, Flier J, Jonker M J, Stoof T J, Von Blomberg B M,
Bruynzeel D P, Scheper R J, Rustemeyer T, Gibbs S. Increased CCL27-CCR10 expression in
allergic contact dermatitis: implications for local skin memory. J Pathol 2004: 204: 39-46.
118
Flier J, Boorsma D M, Bruynzeel D P, Van Beek P J, Stoof T J, Scheper R J, Willemze R,
Tensen C P. The CXCR3 activating chemokines IP-10, Mig, and IP-9 are expressed in allergic
but not in irritant patch test reactions. J Invest Dermatol 1999: 113: 574-8.
119
Homey B, Alenius H, Muller A, Soto H, Bowman E P, Yuan W, Mcevoy L, Lauerma a I,
Assmann T, Bunemann E, Lehto M, Wolff H, Yen D, Marxhausen H, To W, Sedgwick J,
Ruzicka T, Lehmann P, Zlotnik A. CCL27-CCR10 interactions regulate T cell-mediated skin
inflammation. Nat Med 2002: 8: 157-65.
120
Lampa J, Klareskog L, Ronnelid J. Effects of gold on cytokine production in vitro; increase of
monocyte dependent interleukin 10 production and decrease of interferon-gamma levels. J
66
Rheumatol 2002: 29: 21-8.
121
Vamnes J S, Gjerdet N R, Morken T, Moe G, Matre R. In vitro lymphocyte reactivity to gold
compounds in the diagnosis of contact hypersensitivity. Contact Dermatitis 1999: 41: 156-60.
122
Kapsenberg M L, Jansen H M, Bos J D, Wierenga E A. Role of type 1 and type 2 T helper cells
in allergic diseases. Curr Opin Immunol 1992: 4: 788-93.
123
Cher D J, Mosmann T R. Two types of murine helper T cell clone. II. Delayed-type
hypersensitivity is mediated by TH1 clones. J Immunol 1987: 138: 3688-94.
124
Jakobson E, Masjedi K, Ahlborg N, Lundeberg L, Karlberg a T, Scheynius A. Cytokine
production in nickel-sensitized individuals analysed with enzyme-linked immunospot assay:
possible implication for diagnosis. Br J Dermatol 2002: 147: 442-9.
125
Gaffen S L, Liu K D. Overview of interleukin-2 function, production and clinical applications.
Cytokine 2004: 28: 109-23.
126
Sfikakis P P, Souliotis V L, Panayiotidis P P. Suppression of interleukin-2 and interleukin-2
receptor biosynthesis by gold compounds in in vitro activated human peripheral blood
mononuclear cells. Arthritis Rheum 1993: 36: 208-12.
127
Lewandowicz J, Dabkowska B, Nowak D. Influence of gold salts treatment on the serum
concentration of IL-1 and IL-2 in patients with rheumatoid arthritis. Arch Immunol Ther Exp
(Warsz) 1995: 43: 195-8.
128
Mocellin S, Panelli M C, Wang E, Nagorsen D, Marincola F M. The dual role of IL-10. Trends
Immunol 2003: 24: 36-43.
129
Grassegger A, Hopfl R. Significance of the cytokine interferon gamma in clinical dermatology.
Clin Exp Dermatol 2004: 29: 584-8.
130
Cavani A, Nasorri F, Prezzi C, Sebastiani S, Albanesi C, Girolomoni G. Human CD4+ T
lymphocytes with remarkable regulatory functions on dendritic cells and nickel-specific Th1
immune responses. J Invest Dermatol 2000: 114: 295-302.
67