* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Licentiate thesis from the Department of Immunology,
DNA vaccination wikipedia , lookup
Infection control wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Molecular mimicry wikipedia , lookup
Immune system wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Duffy antigen system wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Hepatitis B wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Social immunity wikipedia , lookup
Schistosoma mansoni wikipedia , lookup
Schistosomiasis wikipedia , lookup
Globalization and disease wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Neonatal infection wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
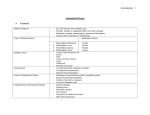
Licentiate thesis from the Department of Immunology, Wenner-Gren Institute, Stockholm University, Sweden Human genetic factors in relation to Plasmodium falciparum infection Manijeh Vafa Stockholm 2007 Summary The first study aimed at investigating if there were any correlations between the IL-10 -1087 A/G and IL-4 -590 C/T polymorphisms and inter-ethnic differences in susceptibility to malaria observed between two sympatric ethnic tribes, the Fulani and the Dogon, living in Mali. The genotypes were correlated to both ethnicity and malariometric indexes. A statistically significant inter-ethnic difference in the allele frequency and genotype inheritance pattern for both loci was noted. The prevalence of infection was associated with the IL-4 -590 T allele within the Fulani. Inter-ethnic differences in spleen rates were seen between the T allele carriers (TT and CT) of both groups. The Fulani CC genotype carriers had significantly lower parasite densities than those carrying the same genotype in the Dogon. No significant differences in parasite prevalence, density and diversity between different IL-4 -590 C/T genotypes were found within the Dogon. No associations between the IL-10 genotypes and P. falciparum prevalence, density and diversity were observed in any of the listed communities. These results suggest an association between; the IL-4 -590 T allele and parasite prevalence and the CC genotype and control of parasitaemia within the Fulani. Individuals living in malaria endemic areas generally harbour multiple parasite strains. Multiplicity of infection (MOI) is known as an indicator of immune status. However, whether high or low MOI are good or bad for the development of immunity to malaria is still not clear. Our second study aimed to examine the MOI in asymptomatic children aged 2-10 years and to relate it to the transmission levels, clinical attacks, erythrocyte variants and other parasitological indexes. MOI was defined as the number of concurrent Plasmodium falciparum clones per individual using PCR method. Sixty four and 87 percent of PCR positive cases had multiple infections before and after the transmission season, respectively. MOI was not age-dependent. A significant association between MOI and parasite density was observed. No correlation between MOI and malaria attacks was noted. The ABO system and HbAS did not affect MOI at any time points, indicating that these factors are involved in the severity of the disease but do not affect asymptomatic infections. α-thalassaemic children did not show an increase in MOI at the end of the transmission season. This might suggest a role for α-thalassaemia in protection against certain parasite strains. G6PD deficiency also protected against an increase in MOI after the transmission season, probably through clearance of the malaria parasite at early stages of infection. ii اى ﻧﺎم ﺗﻮ ﺑﻬﺘﺮﻳﻦ ﺳﺮﺁﻏﺎز ﺗﻘﺪﻳﻢ ﺑﻪ ﻋﺰﻳﺰﺗﺮﻳﻨﻢ ﻣﺤﻤﺪ اﺳﻤﺎﻋﻴﻞ وﻓﺎ و ﺳﺎرا ﻣﺪدى To my dearest, Mohammad E. Vafa and Sara Madadi iii ﺑﻰ ﻧﺎم ﺗﻮ ﻧﺎﻣﻪ آﻰ آﻨﻢ ﺑﺎز List of papers This thesis is based on the following original papers, which will be referred to by their roman numerals. I. Manijeh Vafa, Bakary Maiga, Klavs Berzins, Masashi Hayano, Sandor Bereczky, Amagana Dolo, Modibo Daou, Charles Arama, Bourema Kouriba, Anna Färnert, Ogobara K. Doumbo and Marita Troye-Blomberg, Associations between the IL-4 590 T allele and Plasmodium falciparum infection prevalence in asymptomatic Fulani of Mali. Submitted. II. Manijeh Vafa, Marita Troye-Blomberg, Judith Anchang, Andre Garcia and Florence Migot-Nobias, Multiplicity of Plasmodium falciparum infection in asymptomatic children in a malaria mesoendemic area in Senegal; its relation to transmission, age and erythrocyte variants. Preliminary manuscript. iv TABLE OF CONTENTS SUMMARY .......................................................................................................................................................... II LIST OF PAPERS .............................................................................................................................................. IV ABBREVIATIONS ................................................................................................................................................1 INTRODUCTION..................................................................................................................................................2 GLOBAL INCIDENCE OF MALARIA ........................................................................................................................ 2 MALARIA PARASITE ............................................................................................................................................ 2 Parasite life cycle .......................................................................................................................................... 2 MALARIA DISEASE .............................................................................................................................................. 3 IMMUNITY TO MALARIA ...................................................................................................................................... 4 The RBC polymorphisms ............................................................................................................................... 4 Blood group antigens.................................................................................................................................................. 5 The haemoglobinopathies........................................................................................................................................... 5 Enzyme deficiencies................................................................................................................................................... 6 Innate immunity ............................................................................................................................................. 7 Acquired immunity......................................................................................................................................... 8 Cell-mediated immunity ............................................................................................................................................. 8 Antibody-mediated immunity..................................................................................................................................... 9 Cytokines ..................................................................................................................................................... 10 IFN-γ ........................................................................................................................................................................ 10 TNF-α ...................................................................................................................................................................... 11 IL-4........................................................................................................................................................................... 11 TGF-β....................................................................................................................................................................... 12 IL-10......................................................................................................................................................................... 12 Regulation of immune response to malaria ................................................................................................. 13 RELATED BACKGROUND ..............................................................................................................................14 HUMAN GENETIC FACTORS................................................................................................................................ 14 PARASITE GENETIC DIVERSITY .......................................................................................................................... 14 PRESENT STUDY...............................................................................................................................................16 OBJECTIVES ...................................................................................................................................................... 16 METHODOLOGY ................................................................................................................................................ 17 RESULTS AND DISCUSSIONS .............................................................................................................................. 18 CONCLUDING REMARKS AND FUTURE PERSPECTIVES.....................................................................21 ACKNOWLEDGMENT .....................................................................................................................................22 REFERENCES.....................................................................................................................................................23 Abbreviations APC Antigen-presenting cell CR1 Complement receptor 1 CTL Cytotoxic-T lymphocyte DC Dendritic cell G6PD Glucose-6-phosphate dehydrogenase GPI Glycosylphosphatidylinositol Hb Haemoglobin IFN Interferon Ig Immunoglobulin IL Interleukin IPP Isopentenylpyrophosphate iRBC Infected-Red-Blood Cell MHC Major-histocompatability complex MOI Multiplicity of infection MSP Merozoite-surface protein NK Natural killer PCR Polymerase-chain reaction RBCs Red-blood cells SNP Single-nucleotide polymorphism TCR T-cell receptor TGF Transforming-growth factor Th T helper TLR Toll-like receptor TNF Tumor-necrosis factor Treg Regulatory T cell 1 Introduction Global incidence of malaria Malaria is one of the most important causes of child mortality worldwide. About half a billion episodes of clinical malaria is estimated to occur each year by Plasmodium falciparum infection which results in deaths of more than one million children in sub-Saharan Africa alone 1. Malaria parasite Malaria is caused by an obligate, intracellular protozoan parasite of the genus Plasmodium, transmitted to the vertebrate host by the female Anophele mosquitoes. Of the four species that infect humans (P. falciparum, P. vivax, P. ovale and P. malariae), P. falciparum is responsible for virtually all deaths. Parasite life cycle The malaria parasite has a complex life cycle, including sexual and asexual developmental stages in the mosquito vector and in the human host, respectively. Malaria infection in humans begins when an infected female Anopheles mosquito takes a blood meal and injects 5 to 20 infective sporozoites into the peripheral circulation (Fig. 1). Within minutes (about 30 min) the sporozoites invade hepatocytes in the liver and undergo asexual multiplication for a period of 5 to 10 days, producing liver schizontes. When the infected hepatocyte ruptures, thousands of merozoites are released into the bloodstream that invade red blood cells (RBCs), where they complete another round of asexual multiplication within 48– 72 hours depending on the species of Plasmodium. Infected RBC (iRBC) ruptures and releases 15 to 30 merozoites ready to invade new RBCs and carry on the cycle. This synchronous release of merozoites is thought to be responsible for the periodic fevers associated with malaria. Some invading merozoites do not divide, but differentiate into male and female sexual forms or gametocytes which are ingested by a mosquito when she takes a blood meal. Gametocytes mature into male and female gametes in the gut of mosquito and fertilise to form 2 zygotes. These zygotes further differentiate, migrate through the mosquito gut wall and divide to form thousands of sporozoites. The infective sporozoites move to the salivary gland, where they await injection into another human host, thus completing the life cycle. Figure 1: Adapted from TR Jones and SL Hoffman 2. Malaria disease Infection with P. falciparum has a wide spectrum of manifestations classified as asymptomatic infection or clinical malaria. In malaria endemic areas, a significant proportion of individuals harbour parasites without presenting signs of clinical malaria. Clinical manifestations of malaria range from mild uncomplicated to severe malaria. Fever accompanied by nausea, headache, malaise, cough, diarrhoea and muscular pain are characterized as uncomplicated malaria. 3 While uncomplicated malaria is caused by all four Plasmodium infections, complicated malaria is restricted to P. falciparum. Severe anaemia, cerebral malaria, renal failure, hypoglycaemia, pulmonary oedema, convulsion and shock are the common complications of severe malaria. Immunity to malaria Immunity to malaria is complex and is both stage and species specific. The liver-stage specific antigens have been suggested to be processed and presented on the surface of infected hepatocytes in combination with MHC class I and then presented to T cells. This presentation results in killing of infected cells by cytotoxic T lymphocytes (CTLs) or through IFN-γ produced by NK and CD4+ T cells which triggers a cascade of immune reactions that ultimately leads to the death of the infected cells. During a blood stage infection, parasite antigens released into the bloodstream at the time of erythrocyte rupture, or merozoite-derived antigens expressed on the surface of infected RBCs are the targets of immune response, particularly antibody response 3. Since my studies focus mainly on the blood stage of malaria infection, only factors, cells and components involved in immunity against this stage are overviewed in this thesis. The generation and maintenance of clinical immunity to malaria requires repeated infections over the lifetime. Individuals living in malaria endemic areas eventually develop clinical immunity to P. falciparum which is usually defined as the ability to control parasite replication to a level at which they fail to reach the critical threshold needed for the induction of clinical symptoms. The development of clinical immunity is influenced by age, genetic background of host, pregnancy, nutritional status and co infections 4. Both innate and adaptive immune effector mechanisms are involved in immunity to malaria. However, in most instances the immune response fails to eliminate the infection completely. The RBC polymorphisms The human red blood cell is a central element in malaria life cycle. It provides the parasite with both food and shelter. Moreover, the pathogenic features of the disease are consequences of the interaction between infected RBCs, uninfected RBCs and other tissues. 4 Therefore, it is not surprising that many of the known malaria-protective polymorphisms are related to genes which affect the structure or function of RBCs. Blood group antigens Blood groups A and B are more likely to form rosettes 5, i.e. binding of parasitized red blood cells to uninfected ones which results in severe pathology. Thus, individuals having these blood groups are more prone to experience cerebral malaria as compared to individuals carrying blood group O 6. In the case of P. vivax, the RBC Duffy antigen is important in the merozoite invasion into RBC. P. vivax merozoites are completely dependent on the Duffy/DARC chemokine receptor for RBC invasion 7. RBCs with Duffy negative phenotype are resistant to invasion by P. vivax merozoites 8, 9. The haemoglobinopathies The haemoglobinopathies, conditions affecting the structure and synthesis of haemoglobin, are classified into two categories. The first group results from the production of structurally variable forms of haemoglobin (including haemoglobin S, C and E). The second group is caused by the reduced production of normal α- or β-globin, resulting in α- and βthalassemia, respectively. The clinical effects of these conditions are highly variable (Reviewed by Thomas N Williams) 10 . Haemoglobinopathy provides up to 90% protection against death due to malaria 11. Haemoglobin S (HbS), known as sickle cell disease, in the homozygous state (HbSS) causes severe sequel and is lethal in young children. The sickle cell trait (HbAS) confers a strong protection against P. falciparum malaria as shown in several studies conducted in various countries 11-13 . Despite this the precise mechanisms behind the protection remain incompletely understood. To some extent it relates to particular physical or biochemical properties of HbAS red blood cells. Reduced parasite growth 14, 15 and enhanced removal of parasitized cells through innate 16 or acquired 17, 18 immune responses, have also been proposed to be the mechanisms involved in this protection. Although HbAS protects against severe and lethal malaria, it does not affect asymptomatic parasitaemia 19. 5 In the homozygous form, haemoglobin C (HbCC) and E (HbEE) have mild clinical effects including haemolysis and splenomegaly. The distributions of these polymorphisms in malaria-endemic areas support their malaria-protective effects 10 . The protective effect of HbC is probably due to impaired growth and multiplication of P. falciparum in these RBCs 20. In vitro studies showed that RBCs from subjects with HbE trait are relatively resistant to invasion by P. falciparum merozoites 21 . HbE was associated with reduced malaria severity in adults admitted to hospital in Thailand 22. It is evident that α-thalassemia protects from both severe and fatal malaria 23, 24. Few data also suggest a protective role for it against mild malaria thalassemia does not protect against asymptomatic parasiteamia 10 24, 25 . However, α- and has no effect on parasite densities in individuals that go on to develop the disease 23-25. In 1994, Carlson et al. 26 proposed that the impaired ability of red blood cells to form rosettes is the major mechanism by which α-thalassemia protects against severe malaria. α-thalassemia has also been associated with the reduced expression of the red cell complement receptor 1 (CR1), an essential receptor for rosetting 27. Therefore, α-thalassemia may protect against severe malaria through impaired CR1-mediated resetting. Enzyme deficiencies Glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common enzymopathy in humans. High prevalence of this X-linked disorder in malaria endemic communities suggests its natural selection by malaria 28, 29 . The most common G6PD deficiency allele in sub-Saharan Africa is G6PD A-, which confers about 50% reduction in the risk of developing severe malaria in both heterozygous females and hemizygous males 30. However, the mechanisms behind the protection are still uncertain; Cappadoro et al. showed that it probably involves early phagocytosis of iRBCs. Ring stage infected G6PD deficient RBCs are phagocytosed 2.3 times more intensely than infected normal RBCs 31. Gerbich blood group antigen negativity, CR1 polymorphism and Southeast Asian Ovalocytosis (SAO) are additional examples of malaria resistance genes which involve structure or function of RBCs. 6 Innate immunity Macrophages, DCs, NK, γδ and NKT cells are important effectors of innate immunity against malaria. The importance of macrophages in innate immunity to malaria is due to their ability to phagocytose infected erythrocytes in the absence of cytophilic or opsonizing malaria-specific antibodies. Studies by Serghides et al. indicated that CD36 is involved in this opsonin-independant phagocytosis of P. falciparum-infected erythrocytes by monocytes from non-immune individuals 32. Dendritic cells are important in amplifying the innate immune response, in particular, in stimulating NK cells activation 33, 34 . Although studies have revealed a role of DCs in immune response to many intracellular pathogens, relatively little is known concerning the role of DCs in immunity to malaria. Urban et al. have shown that P. falciparum infected red blood cells suppressed the maturation of DCs ability to activate T cells 36 35 and reduced their . However, studies using experimental animals have shown that DCs from infected mice are fully functional APCs 37. Rapid induction of IFN-γ is essential to control malaria parasitemia in mice 38-40, and NK cells play a crucial role in this early response 38, 41. Similarly, in humans the ability to mount a robust IFN-γ response is associated with reduced susceptibility to infection 42, 43 . Artavanis-Tsakonas et al. showed that IFN-γ is produced by human NK cells in response to P. falciparum-infected RBC within 24 hours 44, suggesting a key role for NK cells in the initial control of blood-stage malaria infections. Polyclonal expansion of γδT-cells during the first few days of P. falciparum infection has been reported 45. Phosphorylated non-peptide antigens, such as IPP, synthesized by P. falciparum have been identified as ligands for human γδT-cells activated γδT-cells produce large amount of IFN-γ 49 47, 48 46 . P. falciparum – and inhibits parasite growth in vitro . Parasite growth inhibition exerted by γδT-cells has been shown to occur at the time of reinvasion, suggesting that extracellular merozoites or late schizonts are the targets for γδTcells 50 . Studies by Farouk et al. revealed that γδT-cells require contact with iRBCs to exert their P. falciparum inhibition/killing activities and that γδT-cells kill the parasite via a granule-exocytosis cytotoxic pathway involving granulysin 51. A granule-exocytosis cytotoxic 7 pathway is a way in which the killing of target cell is mediated by the release of cytolytic molecules such as perforin and granulysin released from cytotoxic granules in the cytolytic cells. γδT-cells have also been correlated to the pathogenesis of cerebral malaria in P. berghei ANKA infected mice 52. NKT cells are mainly involved in pre-erythrocytic anti-malarial immunity. Upon activation through TCR, NKT cells produce high levels of IFN-γ and IL-4 53 . This capacity may contribute them to exert anti-malarial immunity during blood stage where IFN-γ and IL-4 are involved in parasite clearance. Toll-like receptors (TLR) are membrane glycoproteins which recognize components and structures of pathogenic and non-pathogenic microoorganisms. They are involved in the induction of innate immune response to microbial ligands 54. Of the 13 TLR known in mammalian so far 55, TLR2, TLR4 56, 57 and TLR9 58 have been shown to recognize malarial antigens. Hemozoin, a hydrophobic heme polymer, a result from digestion of haemoglobin by P. falciparum, is released into the bloodstream at the time of RBC rupture. Hemozoin has been shown to interact with TLR9 58 . P. falciparum glycosyl- phosphatidylinositols (GPIs) bind to TLR2 and to some extent to TLR4 in both mouse and human macrophages giving rise to TNF-α secretion by these cells 56, 57 which in turn starts inflammatory reactions (see cytokines). Acquired immunity Acquired immunity to malaria involves both cell- and antibody-mediated immunity. Cell-mediated immunity CD4+ T cells play a crucial role in immunity against the asexual blood stages of the malaria parasite. CD4+ T cells produce cytokines which amplify innate immune response and down-regulate this response later on to avoid immunopathology. CD4+ T cells are also required to help B cells to produce anti-malarial antibodies which are key components for parasite clearance. Protective immunity to blood stage of malaria infection is dependent on CD4+ T cells together with antibodies and B cells (Reviewed in reference 59). 8 Naïve CD4+ T cells can differentiate into two distinct subsets during an immune response, T helper (Th) 1 and Th 2, with different profiles of cytokine production. Th 1 cells secrete IFN-γ and are responsible for cell-mediated immunity, whereas Th 2 cells produce IL4 and regulate humoral immunity. Cytokines produced by each of these subsets inhibit the induction of response mediated by the reciprocal subset 60 . IFN-γ production by Th1 cells initiates inflammatory reactions needed for parasite clearance which in excess can lead to immunopathology 3. Th 2 cells control B-cell growth and induce isotype switching from IgM and IgG to IgE 61. Antibody-mediated immunity Antibodies and B cells are critical in immunity against malaria. They play crucial role during blood stage of infection. B cell-deficient mice infected with Plasmodium chabaudi chabaudi AS have been shown to fail to eliminate the infection and instead developed chronic parasitaemias 62. A protective role for antibodies has long been suggested by passive transfer of IgG from immune donors which gave rise to reduction of parasitaemia and clinical disease 63. P. falciparum infected Thai patients treated with IgG purifed from sera of African immune subjects controlled parasitaemias and reduced clinical symptoms, indicating that protective antibodies are raised against conserved antigens shared by P. falciparum parasites worldwide 64, 65 . An infection with P. falciparum parasite induces elevated levels of both polyclonal 66 and anti-malaria specific antibodies. It is evident that antibodies are important in blood stage parasite clearance 67 . Protective anti-malarial antibodies belong to certain Ig classes and subclasses, with IgG being the most important isotype in this respect. Cytophilic IgG1 and IgG3 are considered as protective subclasses, whereas IgG2 and IgG4 are known as non-protective ones. However, IgG2 may also be associated with protection under certain conditions 68 . While IgG has generally been associated with protection against malaria infection, antibodies of the IgE isotype seem to be involved in both protection and pathogenesis of malaria. Elevated levels of total and anti-malarial IgE in Plasmodium infected humans and experimental models have been reported 69, 70 . Total and anti-malarial IgE have been shown to be higher in cerebral malaria patients than those with uncomplicated malaria 69, 71 . However, high levels of anti-P. falciparum IgE have also been associated with a reduced risk of acute malaria in a malaria endemic area in Tanzania 72. 9 Malaria-specific antibodies mediate a number of anti-parasitic effector functions including: inhibition of cytoadherence and thus preventing sequestration of iRBCs and instead letting them be removed by spleen 73; inhibition of RBC invasion 74 and antibody-dependent cytotoxicity 75. Anti-malarial antibodies are involved in the antibody-dependent cell-mediated inhibition (ADCI) mechanism where the parasite growth in inhibited by antibodies bound to Fc receptors on phagocytes 64 . Antibodies may also facilitate parasite clearance by opsonization and phagocytosis by macrophages 76. Cytokines Cytokines induced in response to a malaria infection may play both protective and pathogenic roles. An early pulse of pro-inflammatory cytokines such as TNF-α, IFN-γ, IL-12 and others may mediate protective immunity by inducing parasite killing, while late pro-inflammatory responses might contribute to excessive inflammatory reactions and pathology. Inflammatory response may be down-regulated by anti-inflammatory cytokines, including IL-4, IL-10 and TGF-β. The timing of the anti-inflammatory response seems to be critical. Thus high levels of anti-inflammatory cytokines early during infection are generally believed to suppress mechanisms involved in the resolution of infection, while low levels later during infection lead to a failure to control the inflammatory cytokine cascade with subsequent development of severe pathology. The balance between pro- and antiinflammatory responses may determine the outcome of the disease. A large group of cytokines are involved in immunity and pathogenesis of malaria infection hence only cytokines of our interest and those mentioned in this thesis are more introduced here. IFN-γ Interferon γ is a key inducer of the immune effector mechanisms which are critical to control both pre-erythrocytic and blood-stage of malaria infection 77, 78 . IFN-γ, a macrophage-activating factor, is produced by CD8+ and CD4+ T cell as well as NK cells in response to the malaria parasite. IFN-γ production by T cells may also induce production of the cytophilic IgG1 and IgG3 antibodies in humans 3. Serum IFN-γ levels have been associated with resistance to P. falciparum reinfection 79. Studies in mice have revealed a role 10 for IFN-γ in both protection and pathogenesis of malaria. Although IFN-γ is essential for control of parasitaemias, elevated levels of IFN-γ are also correlated with the onset of cerebral malaria (CM). Similarly, in humans, hyperparasitaemia has been shown to be associated with lower frequencies of IFN-γ producing CD4+ T cells in Gabonese patients suffering from acute P.falciparum malaria. On the other hand, higher plasma levels of IFN-γ were found in symptomatic cases than individuals without clinical pathology, indicating a correlation between disease severity and corresponding IFN-γ levels (reviewed in reference 80). TNF-α Plasmodium-infected erythrocytes and parasite products including parasite pigments and GPI induce TNF-α production in macrophages. TNF-α can increase the expression of Fc-receptors on monocytes resulting in increased phagocytic capacity of these cells. TNF-α has a regulatory effect on IL-12 production by macrophages. Thus TNF-α is an important co-factor for IL-12 to induce IFN-γ production in NK cells (Reviewed by Malaguarnera et al.) 3. TNF-α has been associated with fever resolution and parasite clearance 81, 82 . TNF-α synergises with IFN-γ to induce production of nitric oxide (NO) and thus parasite killing TNF-α 83 . However, risk of death from cerebral malaria correlates with circulating levels of 84 . It has also been shown that high plasma ratios of TNF-α to IL-10 are linked to severe anaemia 85. IL-4 Interleukin (IL)-4 is produced by Th2 and activated mast cells. IL-4 activates CTL, NK cells and macrophages. Together with Th2 cells, IL-4 is important in regulating the antibody response induced by the Plasmodium parasite 3. IL-4 production by CD4+ T cell from malaria exposed donors has been associated with elevated levels of serum antibodies specific for the antigen used to stimulate T cells in vitro 86 . IL-4 has also been shown to suppress IFN-γ production 87 and macrophage-mediated killing of P. falciparum parasite 88. IL-4 is involved in the antibody isotype switching from IgM and IgG to IgE 89. The ratio of mitogen-induced IL-4/IFN-γ producing cells has been correlated with plasma levels of anti-P.falciparum IgE antibodies 90. 11 TGF-β TGF-β, produced by a wide range of cells such as macrophages, NK, T and B cells, has a pivotal role in the control of transition of a Th1 response towards a Th2 response. TGF-β suppresses TNF-α production by macrophages as well as TNF-α and IFN-γ production by NK cells. TGF-β up-regulates IL-10 production. In low concentrations, TGF-β stimulates secretion of Ig subclasses by B cells 91 , while at higher concentrations antibody production is inhibited 92. In mouse models, at the time of peak parasitaemia, a strong TGF-β response was associated with resolution of infection and abrogated mortality. Administration of neutralizing antibody to TGF-β led to 100% mortality in BALB/c mice infected with P. chabaudi chabaudi A/J 93. However, a very early (within 24 hours) burst of TGF-β production leads to a more rapid parasite growth and early death from anaemia. Similar effects were observed after administration of exogenous TGF-β (Reviewed by Artavanis-Tsakonas et al.) 80. IL-10 IL-10 is produced by monocytes, T and B cells. IL-10 induces B-cell proliferation and antibody production. Hence IL-10 plays an important role in the development of immune response against blood stage of malaria infections. IL-10 inhibits IFN-γ, TNF-α and IL-6 production and thus inhibits the cascade of pro-inflammatory reactions and their pathogenic consequences 3. Thus, IL-10 plays a key role in the regulation of the immune response 94. P. chabaudi chabaudi AS infection has been shown to be more lethal in IL-10deficient mice than in their wild type counterparts reported in African children with anaemia 96 95 . Low serum levels of IL-10 have been . The ratio of IL-10/TNF-α concentrations determines the severity of anaemia in infected children 85. High ratios of IFN-γ, TNF-α and IL-12 to TGF-β or IL-10 are associated with decreased risk of malaria infection but increased risk of clinical disease in those who get infected 43. 12 Regulation of immune response to malaria The regulation of anti-malarial specific immune responses is as important as the induction of immune responses that determines the outcome of the infection. Accumulating evidence suggest a central role for regulatory T cells (Treg) in the regulation of immune-mediated pathology of malaria. Treg comprise 5-10% of peripheral CD4+ T cells in humans and are characterized by the expression of the IL-2Rα chain (CD25). Treg mediate the suppression of T-cell activities by inhibiting the IL-2 production and thereby inhibition of the lymphoproliferation, cytotoxicity and cytokine secretion. Treg is not antigen specific and can suppress cells of any TCR specificity. The cytotoxic T lymphocyte Ag-4 (CTLA-4), Foxp3, TLR4, CD25, IL-10 and TGF-β are potential mediators of Treg activities. Antigen-specific, CD25- and Foxp3- T cells can acquire the ability to express Foxp3 and thus differentiate into inducible regulatory cells. TGF-β is known as a physiological inducer of Foxp3. Peripheral CD4+ T cells can be converted to CD4+ CD25+ regulatory T cells by TGF-β and mediate their effects through the release of IL-10 (Tr1 and CD8+ Treg) or TGF-β (Th3 and CD8+ Treg). The role of IL-10 and TGF-β has been demonstrated in the regulation of immune response to malaria (see cytokines). A direct evidence for the role of Treg in the outcome of malaria infection comes from studies in mice. CD4+ CD25+ depletion of naïve mice, infected with P. berghei NK65 led to a significant delay in parasite growth, indicating the enhanced effector responses in the absence of Treg. So far there is no report on the role of Treg on malariainduced mortality. Also in P. yoelli 17XL infected mice the T-cell responses to parasite antigens were amplified after depletion of CD4+ CD25+ T cells, and a normally lethal infection was controlled. Optimally, it looks as if Treg activation and/or Treg-derived cytokine (IL-10 and TGF-β) production are needed to be triggered at the time that proinflammatory cytokines have brought parasite replication under control (Reviewed by Riley et al.) 97. 13 Related background Human genetic factors A range of genetic factors might explain the inter-individual variation in susceptibility/resistance to malaria. Ethnic differences in susceptibility to malaria have been evident during the last decade. Identifying the genes involved in host-parasite relationship, and uncovering how they affect this interaction, offer approaches to the prevention and treatment of malaria. One way to achieve this goal is to uncover the mechanisms involved in protection offered by known malaria resistance genes such as sickle cell trait (HbAS), αthalassaemia, G6PD deficiency and others which are selected in malaria endemic areas. Genetic comparisons of populations living in similar environmental conditions and infection but differing in susceptibility to malaria are other approaches to define the genetic variations making some individuals vulnerable and others resistant to malaria. Studies on susceptibility to malaria in sympatric ethnic groups in Mali 98 and Burkina Faso have indicated that despite exposure to the same parasite and living under the same transmission intensity, the Fulani tribe is less susceptible to malaria infection as defined by fewer malaria attacks, lower parasite densities and higher anti-malarial antibody levels as compared to their neighbouring ethnic tribes, the Mossi and Rimaibe in Burkina Faso and the Dogon in Mali 99-102 . Known anti-malarial-protective genetic disorders; α-thalassaemia, G6PD and HbC, were found to be more frequent in Mossi and Rimaibe as compared to Fulani tribe, while similar frequencies of HbS were noted amongst all tribes 103. Studies in Mali also showed higher frequency of HbC in the Dogon group than the Fulani and a similar, low HbS prevalence in both tribes 98. Parasite genetic diversity The Plasmodium parasite has the ability to change the expression of several surface proteins and consequently alter the antigen profile which the parasite exposes to the host immune system. The extensive repertoires of hyper variable gene families encoding the merozoite surface proteins, enables the Plasmodium parasite to evade the host immune response, particularly to avoid antibody-mediated immunity against parasite-derived surface proteins. This results in strain specific immune response that may explain the need of long 14 term exposure (10-15 years) to a pool of variable parasite strains for naturally acquired immunity to the Plasmodium parasite to develop. In experimental malaria in humans, a primary infection by certain strain resulted in protective immunity against the same strain but not against infection by other strains 104. The Merozoite surface protein 2 (MSP2) also called the merozoite surface antigen 2 (MSA2), encoded by a single-copy gene, is located on the surface of the merozoite and is considered as a blood stage vaccine candidate. The location on the merozoite surface and the fact that a specific monoclonal anti-MSP2 antibody can inhibit the parasite growth 105 are evidences that MSP2 is a target of host protective immune responses. Anti-MSP2 antibodies have been detected in sera from 90% of individuals living in a malaria endemic area 106 . MSP2 consists of highly conserved N (43 residues) and C (74 residues) termini flanking a central variable region (Fig. 2). This central region consists of a series of variable repeat motifs flanked by dimorphic sequences of one of the two major types, the 3D7 and FC27 (also known as type A and type B, respectively). The central repeats vary in number, length and sequence among isolates. Individual MSP2 alleles are defined by the central repeats 107-109. FC27 3D7 Conserved regions Family specific non-repetetive regions Allelic specific repetetive regions Figure 2: Modified from Damon Eisen 110 15 Present study Objectives Study I Ethnicity has a great impact on susceptibility/resistance to malaria. Studies in Burkina Faso 99-102 and Mali 98 have shown that the Fulani tribe are less susceptible against malaria as defined by having less malaria attacks, less P. falciparum prevalence and higher anti-malarial antibodies than their sympatric ethnic groups. IL-4 and IL-10 are two cytokines with critical roles in response to blood stages of the malaria parasite. Cytokine-gene polymorphisms have been shown to influence susceptibility/resistance to a broad range of diseases. Here we investigated the associations between the IL-4 -590 T/C and the IL-10 1087 A/G polymorphisms and inter-ethnic differences in malariometric indexes observed between the Fulani and their neighbouring tribe, the Dogon. Study II Individuals living in malaria endemic areas generally harbour multiple Plasmodium falciparum strains. Multiplicity of malaria infection (MOI) is an indicator of transmission intensity and immune status. MOI has been shown to influence the risk of clinical attack and to be affected by age, seasonal variation and transmission intensity. Erythrocyte polymorphisms are known to confer protection against severe malaria. Studies on the impact of RBC variants on MOI are limited. This study examined MOI in asymptomatic children in a malaria mesoendemic area and its relationship with age, transmission, malaria morbidity, erythrocyte variants and other parasitological indexes. 16 Methodology Materials and methods used in this work are summarised in the text below but described in details in the respective manuscripts. Study I This study included 426 age-matched asymptomatic individuals of the Fulani (214) and the Dogon (212) sympatric tribes living in the Mopti area, Mali. Thick blood films were prepared to determine parasite density. Spleen enlargement was graded according to the Hackett score (1-4). Finger-prick blood was collected on filter papers. Human and parasite DNA were extracted using the Chelex- and TE buffer-based methods, respectively. PCR was performed for both human (IL-4 T/C and IL-10 A/G SNPs) and parasite (msp2/3D7 and msp2/FC27) genotyping. IL-10 and IL-4 genotypes were related to P. falciparum prevalence, density and diversity, as well as to spleen rate. Study II A cohort of 372 asymptomatic subjects (2 -10 years old), living in the Niakhar area, where malaria is mesoendemic, was included in this study. Parasite densities were measured in June and in December 2002. An active survey of malaria attacks was conducted during the transmission period of 2002 for the a sub-group of 154 children. Venous blood was collected in June 2002. ABO blood groups were determined by serology, and the other red blood cell polymorphisms were detected using genomic DNA. Parasite DNA was extracted from blood on filter papers and analysed for the number of msp2 (FC27 and 3D7) clones per infection. Multiplicity of infection was correlated to age, seasonal variation, erythrocyte variants and other parasitological indexes. 17 Results and Discussions Study I Studies performed in Burkina Faso have suggested a distinctly differing genetic background between the Fulani and their sympatric ethnic groups, the Mossi and Rimaibe, using HLA markers 111. In accord to this, we observed a significant difference in IL-4 T/C and IL-10 A/G allele and genotype frequencies between the Fulani and their neighbours, the Dogon, living in Mali. Using the IL-4 -590 T/C SNP as a marker, we found that the Fulani from Mali and Burkina Faso 112 represented almost the same allele and genotype frequencies, while the non-Fulani from the two countries showed very different distribution of the mentioned SNPs. Previous studies on inter-ethnic differences in anti-malarial responses have shown that the Fulani have higher spleen rate than their neighbours 113, 114, are less infected 98, 101, 102 and more immunologicaly responsive to malaria infection 99, 100 . We observed higher numbers of the Fulani individuals presenting enlarged spleen than the Dogon. This was in contrast to other parasitological indexes (prevalence, density and diversity) where there were no statistically significant differences between the two groups. Spleen enlargement was associated with the presence of P. falciparum infection only in the Fulani, suggesting a different role of spleen in response to malaria infection amongst these communities. IL-4 and IL-10 have been shown to play roles in parasite clearance 115 . Thus, polymorphisms in their genes which can lead to variable production of the respective cytokines 116, 117 could affect the parasite counts and other related malariometric indexes. Infection prevalence was higher in Fulani individuals carrying the IL-4 T allele than the CC genotype carriers. The IL-4 T allele has been associated with higher anti-malarial antibody levels in the Fulani. This might indicate that the presence of low grade infections in T allele carriers may induce a constitutive production of antibodies. However, further studies are needed to confirm this. The Fulani IL-4 CC genotype carriers had significantly lower parasite counts as compared to Dogon individuals carrying the same genotype. In a study performed in Burkina Faso 112 , the allele and genotype frequency of IL-4 -590 T/C in the Fulani and two sympatric tribes (Mossi and Rimaibe) was determined and related to anti-malarial antibody levels. It was found that the IL-4 T allele was related to higher anti-malarial antibodies only in the Fulani and not in the other two tribes. This was interpreted as the IL-4 -590 SNP was not functional and probably linked to an unknown 18 factor(s) which is the actual element regulating susceptibly/resistance to malaria. A pronounced difference in IL-4 T/C allele frequency was noted between non-Fulani from Mali (present study) and Burkina Faso 112. Here we observed a significantly lower parasite density amongst the CC genotypes in the Fulani as compared to Dogon individuals having the same genotype. All together, these data suggest that the resistance factor(s) may be linked to the C allele and might be polymorphic in the non-Fulani. The malaria transmission intensity varies between the study areas in Burkina Faso and Mali. This may contribute to the variable selection of certain genetic traits involved in immune response to malaria. When correlating malariametric indexes to the IL-10 -1087 A/G genotypes, we did not observe any significant differences in malariometric indexes between the different genotype carriers in any of the studied groups. Study II Multiplicity of infection (MOI) is the average numbers of different P. falciparum strains simultaneously infecting a single host. MOI can be determined using the polymorphic genes as markers. Genotyping of the highly polymorphic merozoite surface protein 2 (msp2) gene is the standard to define MOI 118. MOI increases as the transmission level increases 119, 120 . In line with this, we found higher MOI at the end of the transmission season as compared to dry season. Previous studies have suggested that high parasite counts increases the probability of detecting higher number of different parasite strains co-infecting an individual 121, 122 . As expected we noted a positive correlation between MOI and parasite density. Individuals living in malaria endemic areas eventually develop immunity to malaria. The age at which the clinical immunity is acquired, depends on the level of exposure and thus differs according to the transmission intensity. The peak MOI is usually seen at this age 123. Studies in holoendemic areas have suggested that MOI is age-dependent 119, 123-126. In contrast to this and in line with studies conducted in a mesoendemic area in Senegal 127 , we found that MOI was not being influenced by age. In areas with intense transmission, antimalaria specific immunity is achieved faster and at younger ages 128 , whereas in areas with less intense malaria transmission the age of peak MOI (development of immunity) is higher. Hence, the lack of age-dependence of MOI observed here could perhaps be because of the low transmission intensity in our study area. Some studies have suggested that a high MOI protects against malaria 129-131 , while others have correlated a high MOI to a higher risk to succumb to clinical malaria 132, 133 . 19 Our observation contradicts with both these suggestions, as we did not find any relation between MOI and malaria morbidity. These discrepancies may in part be due to the different genotyping protocols (with variable sensitivity and accuracy) used in the different studies. RBC variants have long been known to confer protection against severe malaria. The influences of these genetic disorders on the MOI have so far not been well investigated. Here we reported that the MOI did not increase in α-thalassaemic children, indicating that MOI is influenced by α-thalassaemia. Mockenhaupt et al. have shown that α-globin genotype did not affect the MOI in symptomatic subjects 134 . This suggests that α-thalassaemic RBCs may protect against invasion by certain parasite strains but when infection is established, αthalassaemia does not protect against malaria disease. G6PD deficiency showed a similar effect on MOI as α-thalassaemia. G6PD deficient iRBC are known to be removed from circulation at early stage of infection 31. This results in a better control of parasite growth which might lead to a lower increase in MOI at the end of transmission season. This suggests that the protective effects on MOI seen in G6PD deficient- and α-thalassaemic children act through different mechanisms. Blood group O has been known to protect against cerebral malaria 5. However, no reports are available on the influence of the ABO blood group system on MOI. No impact of the different blood groups on MOI was noted in this study. This indicates that ABO antigens may be involved in clinical outcome of malaria but do not affect the MOI. Our data on the impact of sickle cell trait on MOI are in line with those reported by Konate et al. 135 . Both studies did not observe any effect of this trait on the MOI. This contradicts with reports from Gabon 136 , where asymptomatic AS subjects had higher MOI than individuals with normal Hb. This suggests that the effects of HbAS on MOI might be influenced by other factors such as transmission intensity or age of the study groups. 20 Concluding remarks and future perspectives Study I In conclusion, our results revealed that; the Fulani and the Dogon are genetically distinct, spleen enlargement was associated with the presence of parasite only within the Fulani, the Fulani CC genotype carriers had significantly lower parasite density as compared to the Dogon individuals carrying the same genotype, IL-4 -590 T allele was correlated with higher parasite prevalence within the Fulani tribe, the difference in spleen rate amongst the groups was seen only between the IL-4 T allele carriers of the two communities, IL-10 -1087 A/G SNP was not associated with malariometric indexes in any of the tribes. To better clarify the association between the IL-4 -590 T/C SNP and malariometric indexes and also to confirm its role in susceptibility/resistance to malaria, we will determine the allele and genotype distribution amongst symptomatic and asymptomatic subjects; relate it to clinical presentations, parasitological indexes, splenomegaly and antimalarial IgG antibodies. Samples were collected at the end of rainy season year 2005. Study II Taken together our data revealed that MOI; was not age-dependent, was correlated with parasite density, increased after the transmission season, was not influenced by ABO system and HbAS. However, both α-thalassaemia and G6PD deficiency affected the MOI. To further investigate the associations between MOI and development of clinical immunity, we will relate the MOI to the level of anti-MSP2 antibody (total IgG and IgG subclasses) before and after the transmission season in the same study population. 21 Acknowledgment I would like to express my sincere gratitude to: Professor Marita Troye-Blomberg for all your supports, always having time for me and being patient with my non-stop confusions and questions. All seniors and colleagues at the department especially Margareta Hagstedt and Gelana Yadet for always being ready to help. Former and present PhD students especially; Nina-Maria, Salah, Anna-Karin and Petra for nice time we shared in and out of university. Shanie, Camilla, Lisa and Halima for being very good friends. Mohammad E. Vafa and Sara Madadi; my first and best teachers, the most precious treasures one could ever have. Without your love and support I would be nothing. Mehri Vafa and Ali Nadjafi, for simply being the best friends, and being there anytime I need you. All my dear siblings, for being with me through all my way, despite miles of distance. Shiva, for all tears and smiles we shared during years. ﺑﺎ ارزﺷﺘﺮﻳﻦ, اوﻟﻴﻦ و ﺑﻬﺘﺮﻳﻦ ﻣﻌﻠﻤﻴﻨﻢ, واﻟﺪﻳﻦ ﻋﺰﻳﺰم.ﺑﺎ ﻗﺪر داﻧﻰ ازﻣﺤﻤﺪ اﺳﻤﺎﻋﻴﻞ وﻓﺎ و ﺳﺎرا ﻣﺪدى . هﻤﻪ وﺟﻮد ﻣﻦ از ﻋﺸﻖ و ﺣﻤﺎﻳﺖ ﺷﻤﺎ ﺳﺖ.ﺳﺮﻣﺎﻳﻪ ام ﻣﺤﺒﺘﺸﺎن هﻤﻮارﻩ هﻤﺮاﻩ ﻣﻦ ﺑﻮدﻩ,ﺑﺎ ﺗﺸﻜﺮ ﻓﺮاوان از هﻤﺮاهﻰ ﺧﺎﻧﻮادﻩ ﻋﺰﻳﺰم آﻪ ﻋﻠﻴﺮﻏﻢ ﻓﺎﺻﻠﻪ ﻣﻜﺎﻧﻰ .وهﺴﺖ ﺑﻪ ﺁﺧﺮ ﻗﺪم ﻧﻴﺰ ﺑﻨﻤﺎى را ﺑﻪ اول ﺳﺨﻦ دادﻳﻢ دﺳﺘﻜﺎﻩ 22 References 1. Snow, R. W., Guerra, C. A., Noor, A. M., Myint, H. Y. & Hay, S. I. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature 434, 214-217 (2005). 2. Jones, T. R. & Hoffman, S. L. Malaria vaccine development. Clin. Microbiol. Rev. 7, 303310 (1994). 3. Malaguarnera, L. & Musumeci, S. The immune response to Plasmodium falciparum malaria. Lancet Infect. Dis. 2, 472-478 (2002). 4. Fortin, A., Stevenson, M. M. & Gros, P. Susceptibility to malaria as a complex trait: big pressure from a tiny creature. Hum. Mol. Genet. 11, 2469-2478 (2002). 5. Carlson, J. & Wahlgren, M. Plasmodium falciparum erythrocyte rosetting is mediated by promiscuous lectin-like interactions. J. Exp. Med. 176, 1311-1317 (1992). 6. Hill, A. V. Molecular epidemiology of the thalassaemias (including haemoglobin E). Baillieres Clin. Haematol. 5, 209-238 (1992). 7. Chitnis, C. E. & Miller, L. H. Identification of the erythrocyte binding domains of Plasmodium vivax and Plasmodium knowlesi proteins involved in erythrocyte invasion. J. Exp. Med. 180, 497-506 (1994). 8. Miller, L. H., Mason, S. J., Clyde, D. F. & McGinniss, M. H. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. N. Engl. J. Med. 295, 302-304 (1976). 9. Spencer, H. C. et al. The Duffy blood group and resistance to Plasmodium vivax in Honduras. Am. J. Trop. Med. Hyg. 27, 664-670 (1978). 10. Williams, T. N. Human red blood cell polymorphisms and malaria. Curr. Opin. Microbiol. 9, 388-394 (2006). 11. Hill, A. V. et al. Common west African HLA antigens are associated with protection from severe malaria. Nature 352, 595-600 (1991). 23 12. Aidoo, M. et al. Protective effects of the sickle cell gene against malaria morbidity and mortality. Lancet 359, 1311-1312 (2002). 13. Willcox, M. et al. A case-control study in northern Liberia of Plasmodium falciparum malaria in haemoglobin S and beta-thalassaemia traits. Ann. Trop. Med. Parasitol. 77, 239-246 (1983). 14. Friedman, M. J. Erythrocytic mechanism of sickle cell resistance to malaria. Proc. Natl. Acad. Sci. U. S. A. 75, 1994-1997 (1978). 15. Pasvol, G., Weatherall, D. J. & Wilson, R. J. Cellular mechanism for the protective effect of haemoglobin S against P. falciparum malaria. Nature 274, 701-703 (1978). 16. Ayi, K., Turrini, F., Piga, A. & Arese, P. Enhanced phagocytosis of ring-parasitized mutant erythrocytes: a common mechanism that may explain protection against falciparum malaria in sickle trait and beta-thalassemia trait. Blood 104, 3364-3371 (2004). 17. Abu-Zeid, Y. A. et al. Seasonal changes in cell mediated immune responses to soluble Plasmodium falciparum antigens in children with haemoglobin AA and haemoglobin AS. Trans. R. Soc. Trop. Med. Hyg. 86, 20-22 (1992). 18. Bayoumi, R. A. et al. Cell-mediated immune responses to Plasmodium falciparum purified soluble antigens in sickle-cell trait subjects. Immunol. Lett. 25, 243-249 (1990). 19. Williams, T. N. et al. Sickle cell trait and the risk of Plasmodium falciparum malaria and other childhood diseases. J. Infect. Dis. 192, 178-186 (2005). 20. Fairhurst, R. M., Fujioka, H., Hayton, K., Collins, K. F. & Wellems, T. E. Aberrant development of Plasmodium falciparum in hemoglobin CC red cells: implications for the malaria protective effect of the homozygous state. Blood 101, 3309-3315 (2003). 21. Chotivanich, K. et al. Hemoglobin E: a balanced polymorphism protective against high parasitemias and thus severe P falciparum malaria. Blood 100, 1172-1176 (2002). 22. Hutagalung, R. et al. Influence of hemoglobin E trait on the severity of Falciparum malaria. J. Infect. Dis. 179, 283-286 (1999). 24 23. Mockenhaupt, F. P. et al. Alpha(+)-thalassemia protects African children from severe malaria. Blood 104, 2003-2006 (2004). 24. Wambua, S. et al. The effect of alpha+-thalassaemia on the incidence of malaria and other diseases in children living on the coast of Kenya. PLoS Med. 3, e158 (2006). 25. Williams, T. N. et al. High incidence of malaria in alpha-thalassaemic children. Nature 383, 522-525 (1996). 26. Carlson, J., Nash, G. B., Gabutti, V., al-Yaman, F. & Wahlgren, M. Natural protection against severe Plasmodium falciparum malaria due to impaired rosette formation. Blood 84, 3909-3914 (1994). 27. Cockburn, I. A. et al. A human complement receptor 1 polymorphism that reduces Plasmodium falciparum rosetting confers protection against severe malaria. Proc. Natl. Acad. Sci. U. S. A. 101, 272-277 (2004). 28. ALLISON, A. C. Glucose-6-phosphate dehydrogenase deficiency in red blood cells of East Africans. Nature 186, 531-532 (1960). 29. MOTULSKY, A. G. Metabolic polymorphisms and the role of infectious diseases in human evolution. Hum. Biol. 32, 28-62 (1960). 30. Ruwende, C. et al. Natural selection of hemi- and heterozygotes for G6PD deficiency in Africa by resistance to severe malaria. Nature 376, 246-249 (1995). 31. Cappadoro, M. et al. Early phagocytosis of glucose-6-phosphate dehydrogenase (G6PD)deficient erythrocytes parasitized by Plasmodium falciparum may explain malaria protection in G6PD deficiency. Blood 92, 2527-2534 (1998). 32. Serghides, L., Smith, T. G., Patel, S. N. & Kain, K. C. CD36 and malaria: friends or foes? Trends Parasitol. 19, 461-469 (2003). 33. Gerosa, F. et al. The reciprocal interaction of NK cells with plasmacytoid or myeloid dendritic cells profoundly affects innate resistance functions. J. Immunol. 174, 727-734 (2005). 34. Ferlazzo, G. et al. Human dendritic cells activate resting natural killer (NK) cells and are recognized via the NKp30 receptor by activated NK cells. J. Exp. Med. 195, 343-351 (2002). 25 35. Urban, B. C. et al. Plasmodium falciparum-infected erythrocytes modulate the maturation of dendritic cells. Nature 400, 73-77 (1999). 36. Urban, B. C. & Roberts, D. J. Inhibition of T cell function during malaria: implications for immunology and vaccinology. J. Exp. Med. 197, 137-141 (2003). 37. Perry, J. A., Rush, A., Wilson, R. J., Olver, C. S. & Avery, A. C. Dendritic cells from malaria-infected mice are fully functional APC. J. Immunol. 172, 475-482 (2004). 38. De Souza, J. B., Williamson, K. H., Otani, T. & Playfair, J. H. Early gamma interferon responses in lethal and nonlethal murine blood-stage malaria. Infect. Immun. 65, 1593-1598 (1997). 39. Su, Z. & Stevenson, M. M. Central role of endogenous gamma interferon in protective immunity against blood-stage Plasmodium chabaudi AS infection. Infect. Immun. 68, 43994406 (2000). 40. Meding, S. J., Cheng, S. C., Simon-Haarhaus, B. & Langhorne, J. Role of gamma interferon during infection with Plasmodium chabaudi chabaudi. Infect. Immun. 58, 3671-3678 (1990). 41. Mohan, K., Moulin, P. & Stevenson, M. M. Natural killer cell cytokine production, not cytotoxicity, contributes to resistance against blood-stage Plasmodium chabaudi AS infection. J. Immunol. 159, 4990-4998 (1997). 42. Luty, A. J. et al. Interferon-gamma responses are associated with resistance to reinfection with Plasmodium falciparum in young African children. J. Infect. Dis. 179, 980-988 (1999). 43. Dodoo, D. et al. Absolute levels and ratios of proinflammatory and anti-inflammatory cytokine production in vitro predict clinical immunity to Plasmodium falciparum malaria. J. Infect. Dis. 185, 971-979 (2002). 44. Artavanis-Tsakonas, K. & Riley, E. M. Innate immune response to malaria: rapid induction of IFN-gamma from human NK cells by live Plasmodium falciparum-infected erythrocytes. J. Immunol. 169, 2956-2963 (2002). 45. Ho, M. et al. Polyclonal expansion of peripheral gamma delta T cells in human Plasmodium falciparum malaria. Infect. Immun. 62, 855-862 (1994). 26 46. Behr, C. et al. Plasmodium falciparum stimuli for human gammadelta T cells are related to phosphorylated antigens of mycobacteria. Infect. Immun. 64, 2892-2896 (1996). 47. Goodier, M. R., Lundqvist, C., Hammarstrom, M. L., Troye-Blomberg, M. & Langhorne, J. Cytokine profiles for human V gamma 9+ T cells stimulated by Plasmodium falciparum. Parasite Immunol. 17, 413-423 (1995). 48. Hensmann, M. & Kwiatkowski, D. Cellular basis of early cytokine response to Plasmodium falciparum. Infect. Immun. 69, 2364-2371 (2001). 49. Elloso, M. M., van der Heyde, H. C., vande Waa, J. A., Manning, D. D. & Weidanz, W. P. Inhibition of Plasmodium falciparum in vitro by human gamma delta T cells. J. Immunol. 153, 1187-1194 (1994). 50. Troye-Blomberg, M. et al. Human gamma delta T cells that inhibit the in vitro growth of the asexual blood stages of the Plasmodium falciparum parasite express cytolytic and proinflammatory molecules. Scand. J. Immunol. 50, 642-650 (1999). 51. Farouk, S. E., Mincheva-Nilsson, L., Krensky, A. M., Dieli, F. & Troye-Blomberg, M. Gamma delta T cells inhibit in vitro growth of the asexual blood stages of Plasmodium falciparum by a granule exocytosis-dependent cytotoxic pathway that requires granulysin. Eur. J. Immunol. 34, 2248-2256 (2004). 52. Yanez, D. M., Batchelder, J., van der Heyde, H. C., Manning, D. D. & Weidanz, W. P. Gamma delta T-cell function in pathogenesis of cerebral malaria in mice infected with Plasmodium berghei ANKA. Infect. Immun. 67, 446-448 (1999). 53. Yoshimoto, T. & Paul, W. E. CD4pos, NK1.1pos T cells promptly produce interleukin 4 in response to in vivo challenge with anti-CD3. J. Exp. Med. 179, 1285-1295 (1994). 54. Janeway, C. A.,Jr & Medzhitov, R. Innate immune recognition. Annu. Rev. Immunol. 20, 197-216 (2002). 55. Akira, S., Uematsu, S. & Takeuchi, O. Pathogen recognition and innate immunity. Cell 124, 783-801 (2006). 56. Krishnegowda, G. et al. Induction of proinflammatory responses in macrophages by the glycosylphosphatidylinositols of Plasmodium falciparum: cell signaling receptors, 27 glycosylphosphatidylinositol (GPI) structural requirement, and regulation of GPI activity. J. Biol. Chem. 280, 8606-8616 (2005). 57. Zhu, J., Krishnegowda, G. & Gowda, D. C. Induction of proinflammatory responses in macrophages by the glycosylphosphatidylinositols of Plasmodium falciparum: the requirement of extracellular signal-regulated kinase, p38, c-Jun N-terminal kinase and NF-kappaB pathways for the expression of proinflammatory cytokines and nitric oxide. J. Biol. Chem. 280, 8617-8627 (2005). 58. Coban, C. et al. Toll-like receptor 9 mediates innate immune activation by the malaria pigment hemozoin. J. Exp. Med. 201, 19-25 (2005). 59. Stephens, R. & Langhorne, J. Priming of CD4+ T cells and development of CD4+ T cell memory; lessons for malaria. Parasite Immunol. 28, 25-30 (2006). 60. Murphy, K. M. & Reiner, S. L. The lineage decisions of helper T cells. Nat. Rev. Immunol. 2, 933-944 (2002). 61. Lebman, D. A. & Coffman, R. L. Interleukin 4 causes isotype switching to IgE in T cellstimulated clonal B cell cultures. J. Exp. Med. 168, 853-862 (1988). 62. von der Weid, T., Honarvar, N. & Langhorne, J. Gene-targeted mice lacking B cells are unable to eliminate a blood stage malaria infection. J. Immunol. 156, 2510-2516 (1996). 63. COHEN, S., McGREGOR, I. A. & CARRINGTON, S. Gamma-globulin and acquired immunity to human malaria. Nature 192, 733-737 (1961). 64. Bouharoun-Tayoun, H., Attanath, P., Sabchareon, A., Chongsuphajaisiddhi, T. & Druilhe, P. Antibodies that protect humans against Plasmodium falciparum blood stages do not on their own inhibit parasite growth and invasion in vitro, but act in cooperation with monocytes. J. Exp. Med. 172, 1633-1641 (1990). 65. Sabchareon, A. et al. Parasitologic and clinical human response to immunoglobulin administration in falciparum malaria. Am. J. Trop. Med. Hyg. 45, 297-308 (1991). 66. McGregor, I. A. Immunology of malarial infection and its possible consequences. Br. Med. Bull. 28, 22-27 (1972). 28 67. Troye-Blomberg, M. & Perlmann, P. T cell functions in Plasmodium falciparum and other malarias. Prog. Allergy 41, 253-287 (1988). 68. Garraud, O., Perraut, R., Riveau, G. & Nutman, T. B. Class and subclass selection in parasite-specific antibody responses. Trends Parasitol. 19, 300-304 (2003). 69. Perlmann, H. et al. IgE elevation and IgE anti-malarial antibodies in Plasmodium falciparum malaria: association of high IgE levels with cerebral malaria. Clin. Exp. Immunol. 97, 284-292 (1994). 70. Helmby, H. & Troye-Blomberg, M. Differential immunoglobulin E and cytokine responses in BALB/c and C57Bl/6 mice during repeated infections with blood-stage Plasmodium chabaudi malaria. Parasite Immunol. 22, 185-190 (2000). 71. Perlmann, P. et al. Contrasting functions of IgG and IgE antimalarial antibodies in uncomplicated and severe Plasmodium falciparum malaria. Am. J. Trop. Med. Hyg. 62, 373377 (2000). 72. Bereczky, S. et al. Elevated anti-malarial IgE in asymptomatic individuals is associated with reduced risk for subsequent clinical malaria. Int. J. Parasitol. 34, 935-942 (2004). 73. David, P. H., Hommel, M., Miller, L. H., Udeinya, I. J. & Oligino, L. D. Parasite sequestration in Plasmodium falciparum malaria: spleen and antibody modulation of cytoadherence of infected erythrocytes. Proc. Natl. Acad. Sci. U. S. A. 80, 5075-5079 (1983). 74. Wahlin, B. et al. Human antibodies to a Mr 155,000 Plasmodium falciparum antigen efficiently inhibit merozoite invasion. Proc. Natl. Acad. Sci. U. S. A. 81, 7912-7916 (1984). 75. Kumaratilake, L. M., Ferrante, A., Jaeger, T. & Rzepczyk, C. GM-CSF-induced priming of human neutrophils for enhanced phagocytosis and killing of asexual blood stages of Plasmodium falciparum: synergistic effects of GM-CSF and TNF. Parasite Immunol. 18, 115123 (1996). 76. Giribaldi, G., Ulliers, D., Mannu, F., Arese, P. & Turrini, F. Growth of Plasmodium falciparum induces stage-dependent haemichrome formation, oxidative aggregation of band 3, membrane deposition of complement and antibodies, and phagocytosis of parasitized erythrocytes. Br. J. Haematol. 113, 492-499 (2001). 29 77. Good, M. F. & Doolan, D. L. Immune effector mechanisms in malaria. Curr. Opin. Immunol. 11, 412-419 (1999). 78. Plebanski, M. & Hill, A. V. The immunology of malaria infection. Curr. Opin. Immunol. 12, 437-441 (2000). 79. Deloron, P., Chougnet, C., Lepers, J. P., Tallet, S. & Coulanges, P. Protective value of elevated levels of gamma interferon in serum against exoerythrocytic stages of Plasmodium falciparum. J. Clin. Microbiol. 29, 1757-1760 (1991). 80. Artavanis-Tsakonas, K., Tongren, J. E. & Riley, E. M. The war between the malaria parasite and the immune system: immunity, immunoregulation and immunopathology. Clin. Exp. Immunol. 133, 145-152 (2003). 81. Kremsner, P. G. et al. Prediction of accelerated cure in Plasmodium falciparum malaria by the elevated capacity of tumor necrosis factor production. Am. J. Trop. Med. Hyg. 53, 532-538 (1995). 82. Kremsner, P. G. et al. High plasma levels of nitrogen oxides are associated with severe disease and correlate with rapid parasitological and clinical cure in Plasmodium falciparum malaria. Trans. R. Soc. Trop. Med. Hyg. 90, 44-47 (1996). 83. Anstey, N. M. et al. Nitric oxide in Tanzanian children with malaria: inverse relationship between malaria severity and nitric oxide production/nitric oxide synthase type 2 expression. J. Exp. Med. 184, 557-567 (1996). 84. Grau, G. E. et al. Tumor necrosis factor and disease severity in children with falciparum malaria. N. Engl. J. Med. 320, 1586-1591 (1989). 85. Othoro, C. et al. A low interleukin-10 tumor necrosis factor-alpha ratio is associated with malaria anemia in children residing in a holoendemic malaria region in western Kenya. J. Infect. Dis. 179, 279-282 (1999). 86. Troye-Blomberg, M. et al. Production by activated human T cells of interleukin 4 but not interferon-gamma is associated with elevated levels of serum antibodies to activating malaria antigens. Proc. Natl. Acad. Sci. U. S. A. 87, 5484-5488 (1990). 30 87. Vercelli, D., De Monte, L., Monticelli, S., Di Bartolo, C. & Agresti, A. To E or not to E? Can an IL-4-induced B cell choose between IgE and IgG4? Int. Arch. Allergy Immunol. 116, 14 (1998). 88. Kumaratilake, L. M. & Ferrante, A. IL-4 inhibits macrophage-mediated killing of Plasmodium falciparum in vitro. A possible parasite-immune evasion mechanism. J. Immunol. 149, 194-199 (1992). 89. Vercelli, D. Regulation of IgE synthesis. Allergy Proc. 14, 413-416 (1993). 90. Elghazali, G., Perlmann, H., Rutta, A. S., Perlmann, P. & Troye-Blomberg, M. Elevated plasma levels of IgE in Plasmodium falciparum-primed individuals reflect an increased ratio of IL-4 to interferon-gamma (IFN-gamma)-producing cells. Clin. Exp. Immunol. 109, 84-89 (1997). 91. Snapper, C. M., Waegell, W., Beernink, H. & Dasch, J. R. Transforming growth factor-beta 1 is required for secretion of IgG of all subclasses by LPS-activated murine B cells in vitro. J. Immunol. 151, 4625-4636 (1993). 92. Stavnezer, J. Regulation of antibody production and class switching by TGF-beta. J. Immunol. 155, 1647-1651 (1995). 93. Omer, F. M. & Riley, E. M. Transforming growth factor beta production is inversely correlated with severity of murine malaria infection. J. Exp. Med. 188, 39-48 (1998). 94. Mosmann, T. R. Properties and functions of interleukin-10. Adv. Immunol. 56, 1-26 (1994). 95. Linke, A. et al. Plasmodium chabaudi chabaudi: differential susceptibility of gene-targeted mice deficient in IL-10 to an erythrocytic-stage infection. Exp. Parasitol. 84, 253-263 (1996). 96. Kurtzhals, J. A. et al. Low plasma concentrations of interleukin 10 in severe malarial anaemia compared with cerebral and uncomplicated malaria. Lancet 351, 1768-1772 (1998). 97. Riley, E. M., Wahl, S., Perkins, D. J. & Schofield, L. Regulating immunity to malaria. Parasite Immunol. 28, 35-49 (2006). 98. Dolo, A. et al. Difference in susceptibility to malaria between two sympatric ethnic groups in Mali. Am. J. Trop. Med. Hyg. 72, 243-248 (2005). 31 99. Modiano, D. et al. Humoral response to Plasmodium falciparum Pf155/ring-infected erythrocyte surface antigen and Pf332 in three sympatric ethnic groups of Burkina Faso. Am. J. Trop. Med. Hyg. 58, 220-224 (1998). 100. Modiano, D. et al. Interethnic differences in the humoral response to non-repetitive regions of the Plasmodium falciparum circumsporozoite protein. Am. J. Trop. Med. Hyg. 61, 663-667 (1999). 101. Modiano, D. et al. Plasmodium falciparum malaria in sympatric ethnic groups of Burkina Faso, west Africa. Parassitologia 37, 255-259 (1995). 102. Modiano, D. et al. Different response to Plasmodium falciparum malaria in west African sympatric ethnic groups. Proc. Natl. Acad. Sci. U. S. A. 93, 13206-13211 (1996). 103. Modiano, D. et al. The lower susceptibility to Plasmodium falciparum malaria of Fulani of Burkina Faso (west Africa) is associated with low frequencies of classic malaria-resistance genes. Trans. R. Soc. Trop. Med. Hyg. 95, 149-152 (2001). 104. Jeffery, G. M. Epidemiological significance of repeated infections with homologous and heterologous strains and species of Plasmodium. Bull. World Health Organ. 35, 873-882 (1966). 105. Epping, R. J. et al. An epitope recognised by inhibitory monoclonal antibodies that react with a 51 kilodalton merozoite surface antigen in Plasmodium falciparum. Mol. Biochem. Parasitol. 28, 1-10 (1988). 106. al-Yaman, F. et al. Relationship between humoral response to Plasmodium falciparum merozoite surface antigen-2 and malaria morbidity in a highly endemic area of Papua New Guinea. Am. J. Trop. Med. Hyg. 51, 593-602 (1994). 107. Smythe, J. A. et al. Structural diversity in the 45-kilodalton merozoite surface antigen of Plasmodium falciparum. Mol. Biochem. Parasitol. 39, 227-234 (1990). 108. Thomas, A. W., Carr, D. A., Carter, J. M. & Lyon, J. A. Sequence comparison of allelic forms of the Plasmodium falciparum merozoite surface antigen MSA2. Mol. Biochem. Parasitol. 43, 211-220 (1990). 32 109. Smythe, J. A. et al. Structural diversity in the Plasmodium falciparum merozoite surface antigen 2. Proc. Natl. Acad. Sci. U. S. A. 88, 1751-1755 (1991). 110. Eisen, D., Billman-Jacobe, H., Marshall, V. F., Fryauff, D. & Coppel, R. L. Temporal variation of the merozoite surface protein-2 gene of Plasmodium falciparum. Infect. Immun. 66, 239-246 (1998). 111. Modiano, D. et al. HLA class I in three West African ethnic groups: genetic distances from sub-Saharan and Caucasoid populations. Tissue Antigens 57, 128-137 (2001). 112. Luoni, G. et al. Antimalarial antibody levels and IL4 polymorphism in the Fulani of West Africa. Genes Immun. 2, 411-414 (2001). 113. Bryceson, A. D., Fleming, A. F. & Edington, G. M. Splenomegaly in Northern Nigeria. Acta Trop. 33, 185-214 (1976). 114. Greenwood, B. M. et al. Ethnic differences in the prevalence of splenomegaly and malaria in The Gambia. Ann. Trop. Med. Parasitol. 81, 345-354 (1987). 115. Troye-Blomberg, M., Berzins, K. & Perlmann, P. T-cell control of immunity to the asexual blood stages of the malaria parasite. Crit. Rev. Immunol. 14, 131-155 (1994). 116. Turner, D. M. et al. An investigation of polymorphism in the interleukin-10 gene promoter. Eur. J. Immunogenet. 24, 1-8 (1997). 117. Rosenwasser, L. J. et al. Promoter polymorphisms in the chromosome 5 gene cluster in asthma and atopy. Clin. Exp. Allergy 25 Suppl 2, 74-8; discussion 95-6 (1995). 118. Viriyakosol, S. et al. Genotyping of Plasmodium falciparum isolates by the polymerase chain reaction and potential uses in epidemiological studies. Bull. World Health Organ. 73, 8595 (1995). 119. Arnot, D. Unstable malaria in Sudan: the influence of the dry season. Clone multiplicity of Plasmodium falciparum infections in individuals exposed to variable levels of disease transmission. Trans. R. Soc. Trop. Med. Hyg. 92, 580-585 (1998). 33 120. Babiker, H. A., Ranford-Cartwright, L. C. & Walliker, D. Genetic structure and dynamics of Plasmodium falciparum infections in the Kilombero region of Tanzania. Trans. R. Soc. Trop. Med. Hyg. 93 Suppl 1, 11-14 (1999). 121. Contamin, H. et al. PCR typing of field isolates of Plasmodium falciparum. J. Clin. Microbiol. 33, 944-951 (1995). 122. Farnert, A. et al. Genotyping of Plasmodium falciparum infections by PCR: a comparative multicentre study. Trans. R. Soc. Trop. Med. Hyg. 95, 225-232 (2001). 123. Ntoumi, F. et al. Age-dependent carriage of multiple Plasmodium falciparum merozoite surface antigen-2 alleles in asymptomatic malaria infections. Am. J. Trop. Med. Hyg. 52, 81-88 (1995). 124. Felger, I. et al. Plasmodium falciparum: extensive polymorphism in merozoite surface antigen 2 alleles in an area with endemic malaria in Papua New Guinea. Exp. Parasitol. 79, 106-116 (1994). 125. Beck, H. P. et al. Analysis of multiple Plasmodium falciparum infections in Tanzanian children during the phase III trial of the malaria vaccine SPf66. J. Infect. Dis. 175, 921-926 (1997). 126. Guerra-Neira, A. et al. Plasmodium diversity in non-malaria individuals from the Bioko Island in Equatorial Guinea (West Central-Africa). Int. J. Health. Geogr. 5, 27 (2006). 127. Zwetyenga, J. et al. No influence of age on infection complexity and allelic distribution in Plasmodium falciparum infections in Ndiop, a Senegalese village with seasonal, mesoendemic malaria. Am. J. Trop. Med. Hyg. 59, 726-735 (1998). 128. Baird, J. K. Host age as a determinant of naturally acquired immunity to Plasmodium falciparum. Parasitol. Today 11, 105-111 (1995). 129. al-Yaman, F. et al. Reduced risk of clinical malaria in children infected with multiple clones of Plasmodium falciparum in a highly endemic area: a prospective community study. Trans. R. Soc. Trop. Med. Hyg. 91, 602-605 (1997). 34 130. Farnert, A., Rooth, I., Svensson, Snounou, G. & Bjorkman, A. Complexity of Plasmodium falciparum infections is consistent over time and protects against clinical disease in Tanzanian children. J. Infect. Dis. 179, 989-995 (1999). 131. Muller, D. A. et al. Prospective risk of morbidity in relation to multiplicity of infection with Plasmodium falciparum in Sao Tome. Acta Trop. 78, 155-162 (2001). 132. Branch, O. H. et al. Plasmodium falciparum genotypes, low complexity of infection, and resistance to subsequent malaria in participants in the Asembo Bay Cohort Project. Infect. Immun. 69, 7783-7792 (2001). 133. Ofosu-Okyere, A. et al. Novel Plasmodium falciparum clones and rising clone multiplicities are associated with the increase in malaria morbidity in Ghanaian children during the transition into the high transmission season. Parasitology 123, 113-123 (2001). 134. Mockenhaupt, F. P. et al. Limited influence of haemoglobin variants on Plasmodium falciparum msp1 and msp2 alleles in symptomatic malaria. Trans. R. Soc. Trop. Med. Hyg. 98, 302-310 (2004). 135. Konate, L. et al. Variation of Plasmodium falciparum msp1 block 2 and msp2 allele prevalence and of infection complexity in two neighbouring Senegalese villages with different transmission conditions. Trans. R. Soc. Trop. Med. Hyg. 93 Suppl 1, 21-28 (1999). 136. Ntoumi, F. et al. Plasmodium falciparum: sickle-cell trait is associated with higher prevalence of multiple infections in Gabonese children with asymptomatic infections. Exp. Parasitol. 87, 39-46 (1997). 35