* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Treating heart attack with different food substrates
Survey
Document related concepts
Transcript
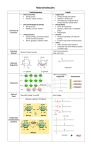
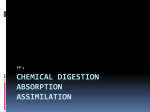
REVIEW www.nature.com/clinicalpractice/cardio Modification of myocardial substrate use as a therapy for heart failure Khalid Abozguia*, Kieran Clarke, Leong Lee and Michael Frenneaux S U M M A RY INTRODUCTION Despite advances in treatment, chronic heart failure is still associated with significant morbidity and a poor prognosis. The scope for further advances based on additional neurohumoral blockade is small. Effective adjunctive therapies acting via a different cellular mechanism would, therefore, be attractive. Energetic impairment seems to contribute to the pathogenesis of heart failure. The findings from several studies have shown that the socalled metabolic agents could have potential as adjunctive therapies in heart failure. These agents cause a shift in the substrate used by the heart away from free fatty acids, the oxidation of which normally provides around 70% of the energy needed, towards glucose. The oxygen cost of energy generation is lessened when glucose is used as the substrate. In this review we aim to draw attention to the metabolic alteration in heart failure and we present evidence supporting the use of metabolic therapy in heart failure. KEYWORDS cardiac energetic, heart failure, metabolic manipulation, myocardial energy metabolism, myocardial substrate metabolism REVIEW CRITERIA All articles were identified by searching PubMed. The search used the following key phrases in different combinations: “metabolic manipulation”, “myocardial energy metabolism”, “myocardial substrate metabolism”, “heart failure”, “perhexiline”, “trimetazidine”, “etomoxir”, “ranolazine” and “oxfenicine”. All referenced articles were full-text, English-language papers, published from 1960 to 2005. We searched the articles’ bibliographies and our own database for further relevant papers. K Abozguia is a British Heart Foundation Research Fellow in and M Frenneaux is the Head of the Department for Cardiovascular Medicine, University of Birmingham, Birmingham, UK. K Clarke is a professor of physiological biochemistry in the University Laboratory of Physiology, University of Oxford, Oxford, UK, and L Lee is a Specialist Registrar in the Department of Cardiology, Queens Medical Centre, Nottingham University Hospital, Nottingham, UK. Correspondence *Department of Cardiovascular Medicine, University of Birmingham, Edgbaston, Birmingham B15 2TT, UK [email protected] Received 5 December 2005 Accepted 12 April 2006 www.nature.com/clinicalpractice doi:10.1038/ncpcardio0583 490 NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE ©2006 Nature Publishing Group An important role for an abnormal cardiac energetic status has been indicated in the pathophysiology of heart failure, even in the absence of coronary artery disease.1 Most studies on metabolism in the heart have been done on human biopsy samples2 or in vivo by use of phosphorus31 nuclear magnetic resonance spectroscopy.3 Findings indicate that the concentration of ATP is approximately 20–30% lower in failing human hearts than in healthy hearts, although this finding has not been reported in all studies. In the rapid pacing canine model of heart failure, a progressive monotonic decay of both ATP and the total adenine nucleotide pool begins well before the onset of heart failure.4 Phosphocreatine is an important short-term reserve energy source that maintains a high phosphorylation potential under conditions of increased energy demand (e.g. exercise). The transfer of a phosphoryl group from phosphocreatine to ADP by the enzyme creatine kinase generates ATP at a rate approximately 10 times faster than the maximum rate of ATP generation via oxidative phosphorylation.5 In patients with mild to moderate heart failure, cardiac ATP flux mediated by creatine kinase is reduced by approximately 50%.6 Studies of human and animal models of heart failure have demonstrated a progressive reduction in the creatine pool of up to 60%. The magnitude of this reduction is related to the severity of heart failure,7–9 and is largely due to a decrease in the number of creatine transporters at sites of energy production and utilization.10 In healthy hearts, approximately two-thirds of the total creatine pool is phosphorylated via the creatine kinase reaction to form phosphocreatine. In heart failure, the available phosphocreatine is depleted to a greater degree than ATP, as indicated by reduced phosphocreatine-to-ATP ratios seen on phosphorus-31 nuclear magnetic resonance spectroscopy.11 The risk of death increases as this ratio decreases.12 As well as the reduced creatine pool, the reduction in SEPTEMBER 2006 VOL 3 NO 9 REVIEW www.nature.com/clinicalpractice/cardio phosphocreatine in heart failure is partly due to reduced expression of the creatine kinase isoenzymes, particularly of mitochondrial creatine kinase, leading to a reduced ratio of phosphocreatine to total creatine.10 Nitric oxide produced by inducible nitric oxide synthase might also inhibit mitochondrial creatine kinase activity.13 Short-term oral creatine supplementation in chronic heart failure has been shown to increase skeletal muscle function, but no effect was observed on left ventricular ejection fraction.14 The reduced ATP production and depletion of phosphocreatine stores in heart failure produce a short-term buffer to acute increases in ATP demand. The ability to generate ATP is normally modulated via effects on mitochondrial density, substrate use, expression and activities of mitochondrial enzymes, and adenosine 5´-monophosphate-activated protein kinase systems. Peroxisome proliferative activated receptor γ coactivator 1-α (PGC-1α) appears to be a key energy sensor in these homeostatic systems.15 Mice that are deficient in PGC-1α exhibit reduced expression of genes of oxidative metabolism in cardiac and skeletal muscle, associated with reduced levels of ATP. Young mice exhibit reduced cardiac work output in response to chemical or electrical stimulation, and resting cardiac dysfunction develops with age.15 Maneuvers that could increase ATP production even slightly might substantially improve the status of patients. In this review we aim to draw attention to the metabolic alteration in heart failure and we present evidence supporting the use of metabolic therapy for this condition. MYOCARDIAL SUBSTRATE USE IN HEART FAILURE The fetal heart uses glucose as its primary substrate, but a shift to predominant use of free fatty acids occurs soon after birth.16 In adulthood, approximately 70% of energy production in healthy hearts is derived from β-oxidation of fatty acids,17 with the balance being obtained from a mix of lactate, pyruvate and ketones. Concentrations of all these substances fluctuate because of control by metabolic mechanisms, but the heart has the ability to alter the proportions of substrates used to meet metabolic demands when oxygen availability is limited; for example, during ischemia the use of glucose increases, although that of free fatty acids typically remains at more than 50%. This consistent use of free SEPTEMBER 2006 VOL 3 NO 9 ABOZGUIA ET AL. fatty acids as the main substrate is thought to represent a particular advantage.17 Much of the data on substrate use in heart failure have been obtained from animal models of left ventricular hypertrophy or of left ventricular hypertrophy progressing to heart failure. Heart failure is a complex syndrome, and the pattern of substrate use seems to depend on species, etiology, duration, whether underlying coronary artery disease is present, endothelial dysfunction, gene expression and whether comorbid disorders, such diabetes and hypertension, are present.18 An increase in glucose use has frequently been reported19,20 and is partly a consequence of a shift in cardiac gene expression from the postnatal pattern to a fetal pattern.16 Some controversy exists as to whether the shift towards glucose use is adaptive or maladaptive. In the rapid pacing canine model of heart failure, in contrast to models of left ventricular hypertrophy, the main substrate is free fatty acids rather than glucose.21 More importantly, most studies of heart failure in humans have reported that free-fatty-acid use is either unchanged or increased compared with that in healthy controls.22,23 Taylor et al.23 noted increased uptake of free fatty acids and reduced use of glucose in a PET study of heart failure. Contributory factors to this change might include reduced transport of glucose via insulin-stimulated glucose transporter 4,21 and increased concentrations of free fatty acids in plasma. Randle24 proposed that these mechanisms lead to increased use of free fatty acids and to suppression of glucose use (Figure 1). Although PET scanning offers high sensitivity in humans, it provides no chemical specificity and cannot distinguish the various fates of a substrate (such as storage, oxidation, back diffusion, etc.). Development of technologies such as carbon-13 nuclear magnetic resonance spectroscopy and hyperpolarization might improve the yield of biochemical information, but have yet to be tested in humans.25 SUBSTRATE USE AND MYOCARDIAL OXYGEN USE Simple stoichiometry suggests that the use of fatty acids should cost approximately 12% more oxygen per unit of ATP generated than glucose. Given that use of this substrate accounts for approximately 70% of heart oxygen consumption in healthy individuals, and that interventions are unlikely to produce a complete shift to either free-fatty-acid or glucose use, NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE 491 ©2006 Nature Publishing Group REVIEW www.nature.com/clinicalpractice/cardio Insulin FFA Glucose IR Glut4 FATP1 Glucose Hexokinase → FA-CoA → G6P PFK CPT1 Glycolysis → Citrate ADP ATP Pyruvate PDH CPT2 → Acetyl-CoA Lactate IMM OMM Figure 1 The glucose–fatty acid cycle in cardiomyocyte mitochondria. The relationship between glucose and free fatty acid metabolism is thought to be reciprocal. Oxidation of free fatty acids can inhibit catabolism of glucose in muscle, and the effects are mediated by inhibition of phosphofructokinase 1 and of the pyruvate dehydrogenase complex. The mitochondrial concentration ratio of acetyl-coenzyme A to coenzyme A inhibits the pyruvate dehydrogenase complex, the rise in citrate inhibits phosphofructokinase 1, and the increase in glucose-6-phosphate inhibits hexokinase. Free fatty acid oxidation inhibits insulinstimulated accelerated glucose transport. While confirming the reciprocal relationship between metabolism of free fatty acids and glucose, however, this mechanism has not been supported by the findings of several human studies, and a cellular mechanism by which free fatty acids or their metabolites interfere with glucose metabolism involving alteration of membrane properties and glucose transport is proposed. Abbreviations: CoA, coenzyme A; CPT, carnitine palmitoyltransferase; FA-CoA, fatty acid coenzyme A; FATP1, fatty acid transporter protein 1; FFA, free fatty acid; G6P, glucose-6-phosphate; Glut4, glucose transporter 4; IMM, inner mitochondrial membrane; IR, insulin receptor; OMM, outer mitochondrial membrane; PDH, pyruvate dehydrogenase; PFK, phosphofructokinase 1. changes of less than 12% in oxygen consumption would be anticipated. Several studies have shown, however, that high concentrations of free fatty acids were associated with a decrease in cardiac mechanical efficiency of 30%.26,27 This finding suggests an oxygen-wasting effect much greater than that predicted by stoichiometry. The difference in values might be explained by the observation that activation of peroxisome proliferative activated receptor α by free fatty acids upregulates uncoupling-protein expression in the mitochondria.28 492 NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE ©2006 Nature Publishing Group Normally, the electron transport chain results in the generation of a net proton gradient across the inner mitochondrial membrane. In tightly coupled mitochondria little proton leakage occurs across this membrane and all the energy from the respiratory chain can be used to phosphorylate ADP to generate ATP. When mitochondria are uncoupled, protons leak into the mitochondrion while long-chain fatty acids from the mitochondrial matrix are transported into the soluble cytoplasm; this process dissipates the electrochemical gradient.29 The export ABOZGUIA ET AL. SEPTEMBER 2006 VOL 3 NO 9 REVIEW www.nature.com/clinicalpractice/cardio of long-chain fatty acids from the mitochondrion when fatty acid delivery exceeds oxidative capacity seems, in fact, to be the primary role of uncoupling proteins.29 Uncoupling could, therefore, be expected to occur when mitochondrial concentrations of free fatty acids are raised. The rate of this process will be increased when uncoupling-protein expression rises, for example when plasma concentrations of free fatty acids become elevated because of sympathetic activation in heart failure. Consistent with this concept, Murray and co-workers30 showed that mitochondrial uncoupling-protein expression in human cardiac muscle correlated with a rise in plasma concentrations of free fatty acids.30 An additional mechanism proposed for the extra oxygen requirement in the use of free fatty acids as the substrate is that high concentrations of free fatty acids trigger intracellular futile metabolic cycles, with wasteful cycling through intramyocardial lipolysis and re-esterification.31 METABOLIC AGENTS AS THERAPY FOR HEART FAILURE In a study in the late 1990s, intracoronary pyruvate was shown to acutely increase stroke volume and reduce pulmonary capillary wedge pressure.32 The implication of this finding is that an acute beneficial shift away from fatty acid metabolism can be achieved. Since that study was reported, several others have demonstrated similar beneficial effects of modifying substrate use in chronic heart failure. Several pharmacologic agents have been shown to inhibit the use of free fatty acids in the heart, either by inhibiting uptake into the mitochondria or by inhibiting β-oxidation. Some of these agents are used as antianginal agents because of their oxygen-sparing actions. Trimetazidine Trimetazidine (1-[2,3,4-trimethoxybenzyl] piperazine dihydrochloride) can lessen oxidation of free fatty acids via inhibition of the enzyme long-chain 3-ketoacyl coenzyme A thiolase, which is crucial in the β-oxidation pathway.33 This mechanism might not, however, be the only, or even the principal, route of action for this drug.34 Trimetazidine, an effective antianginal therapy, has a favorable side-effect profile and exhibits no notable vasodilator properties at rest or during dynamic exercise.35 Left ventricular systolic and diastolic function and quality of life improved after trimetazidine therapy in a SEPTEMBER 2006 VOL 3 NO 9 ABOZGUIA ET AL. double-blind, placebo-controlled trial involving 47 patients with coronary artery disease and a reduced left ventricular function who were limited by angina but not by heart failure.36 In an open-label study of 18 months’ duration, Di Napoli et al.37 demonstrated a significant improvement in left ventricular function in patients who had ischemic cardiomyopathy with left ventricular ejection fractions lower than 40%. Patients were excluded if they had experienced acute myocardial infarction less than 3 months previously, or had acute heart failure or cardiac decompensation, and many patients were taking suboptimum conventional therapy. Rosano and colleagues38 demonstrated improvements in left ventricular ejection fraction among patients with diabetes and coronary heart disease and left ventricular systolic dysfunction, but without frank heart failure, following 6 months of trimetazidine therapy. By contrast, another study, which assessed the effects of trimetazidine in patients with heart failure who were diabetic, demonstrated no significant effect on exercise capacity and only minor effects on left ventricular systolic function in both resting and exercise states.39 Most of the patients studied so far, however, do not have overt heart failure and findings need clarification for this indication. Ranolazine Ranolazine has been shown to partly inhibit fatty acid β oxidation,40,41 but these findings have not been reliably replicated in large experimental or human studies. The principal mechanism of action for this drug as an antianginal remains controversial, although data demonstrating blockade of the late sodium current have been published.42 Ranolazine reduces sodium entry into ischemic myocardial cells and, therefore, is thought indirectly to reduce calcium uptake via the sodium–calcium exchanger, to preserve ionic homeostasis, and to reverse ischemia-induced contractile dysfunction.42 In a study of a canine microembolization model of heart failure, intravenous ranolazine increased myocardial work without increasing myocardial oxygen use, which implies an increase in cardiac efficiency.43 Acute intravenous administration of ranolazine has also improved left ventricular systolic function in dogs with heart failure.44 The effects of ranolazine in humans with chronic heart failure have not yet been reported. In experimental studies, the drug slightly prolongs the QT interval on electrocardiograms. This effect has been associated with NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE 493 ©2006 Nature Publishing Group REVIEW www.nature.com/clinicalpractice/cardio FFA Glucose Perhexiline Etomoxir Oxfenicine ? β-blockers FATP1 Glut4 Glucose FA-CoA Trimetazidine ? ranolazine Hexokinase Malonyl-CoA G6P CPT1 Glycolysis CPT2 Acyl-CoA β-oxidation Acetyl-CoA carboxylase Acetyl-CoA PDH ADP ATP Pyruvate Lactate IMM OMM Figure 2 Effects of metabolic agents on myocardial metabolism in cardiomyocyte mitochondria. Perhexiline, oxfenicine, and etomoxir prevent uptake of free fatty acids via inhibition of carnitine palmitoyltransferase I, which is a key enzyme in this process in mitochondria. Trimetazidine and possibly ranolazine inhibit β-oxidation of free fatty acids. Evidence suggests that ranolazine acts via inhibiting late sodium entry into the cardiomyocyte. These actions shift myocardial substrate use from free fatty acids to glucose, which is more efficient in terms of energy production, leading to an oxygen-sparing effect. Abbreviations: CoA, coenzyme A; CPT, carnitine palmitoyltransferase; FA-CoA, fatty acid coenzyme A; FATP1, fatty acid transporter protein 1; FFA, free fatty acid; G6P, glucose-6-phosphate; Glut4, glucose transporter 4; IMM, inner mitochondrial membrane; OMM, outer mitochondrial membrane; PDH, pyruvate dehydrogenase. risk of ventricular tachycardia, particularly torsade de pointes polymorphic ventricular tachycardia, and with sudden cardiac death.45 The long-term safety of ranolazine remains to be established. Oxfenicine Oxfenicine is an inhibitor of carnitine palmitoyltransferase I (CPT1), a key enzyme involved in the uptake of long-chain fatty acids into the mitochondria (Figure 2). In a randomized, placebocontrolled study using the canine rapid pacing model of heart failure, oxfenicine delayed the development of terminal heart failure, attenuated adverse hemodynamic changes, prevented wall thinning, prevented the activation of matrix metalloproteinases, and resulted in the transcriptional downregulation of CPT1 and of key enzymes involved in cardiac energy metabolism.46 In animal models, oxfenicine therapy 494 NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE ©2006 Nature Publishing Group was associated with dose-related increases in cardiac weight due to uniform myocardial fiber hypertrophy involving all cardiac chambers,47 as well as an increase in liver and kidney weights.48 The mechanisms responsible for these observations are not yet clearly understood. Etomoxir Etomoxir is an oxirane carboxylic acid derivative that inhibits CPT1.49 This drug was introduced as a potential therapy for diabetes because of its hypoglycemic effects.50 Its effects on ischemia, left ventricular hypertrophy, and left ventricular impairment have been studied in animals.51,52 Therapy with this drug favorably modified ventricular mass, geometry and function in pressure-overloaded rats,51 and reduced the occurrence of ventricular failure in diabetic rat hearts.52 In a human, open-label, uncontrolled ABOZGUIA ET AL. SEPTEMBER 2006 VOL 3 NO 9 REVIEW www.nature.com/clinicalpractice/cardio Perhexiline Perhexiline seems to cause a shift in cardiac substrate use from fatty acids to carbohydrates.58 In isolated Langendorff-perfused rat hearts, perhexiline inhibited both CPT1 and carnitine palmitoyltransferase II (Figure 2).59,60 Perhexiline was frequently used as antianginal agent in the 1970s and is an effective monotherapy for relieving symptoms of angina,61 improving exercise tolerance, and increasing the workload needed to induce ischemia.62 Use declined dramatically in the late 1970s and early 1980s following reports of hepatotoxic effects63 and peripheral neuropathy.64 These effects were later demonstrated to occur in patients in whom hydroxylation is slow and who have a genetic variant of a cytochrome P450 enzyme, which SEPTEMBER 2006 VOL 3 NO 9 ABOZGUIA ET AL. 22– 20– VO2max (ml kg–1 min–1) β-blockers β-adrenoreceptor blockade improves left ventricular function and prognosis in patients with ischemic or nonischemic cardiomyopathy.54,55 The mechanisms of this beneficial effect are multifactorial and could include a shift from free fatty acid to glucose use. Wallhaus et al.56 demonstrated a 57% reduction in myocardial free fatty acid uptake following treatment with carvedilol in patients with heart failure. In this relatively small study, however, neither mean myocardial uptake of labeled glucose tracers nor the rate of glucose use increased significantly. This finding might reflect a type II error, since a marked fall in the ratio of myocardial free fatty acid to glucose use does suggest a so-called metabolic shift induced by carvedilol. The authors of the study speculated that this effect was related to CPT1 inhibition, although little supporting evidence for this effect is available. Furthermore, Al-Hesayen and colleagues57 showed that 4 months of carvedilol therapy increased myocardial lactate consumption and reduced myocardial uptake of free fatty acids in patients with chronic heart failure. This finding implies that carvedilol therapy causes a significant shift in myocardial substrate use from free fatty acids to glucose. A 18– 16– 14– 12– 10– B Before placebo After placebo Before perhexiline After perhexiline Before placebo After placebo Before perhexiline After perhexiline 40– 30– LVEF (%) trial conducted in 10 patients with NYHA class II–III heart failure, a 3-month period of etomoxir treatment in addition to standard therapy was associated with a significant improvement in left ventricular ejection fraction, cardiac output at peak exercise, and clinical status.53 Etomoxir has yet, however, to be investigated in a long-term, randomized, controlled trial in heart failure. 20– 10– 0– Figure 3 The effect of perhexiline treatment in patients with ischemic or nonischemic heart failure. (A) Effect on peak exercise oxygen consumption. (B) Effect on left ventricular ejection fraction. Reproduced, with permission, from reference 68 © (2005) Lippincott, Williams & Wilkins. Abbreviations: LVEF, left ventricular ejection fraction; VO2max, maximum volume of oxygen consumption. metabolizes the drug, resulting in drug accumulation and, subsequently, accumulation of phospholipids in the liver and nerves.65 The risk of toxic effects is virtually eliminated by maintaining plasma concentrations at between 150 and 600 ng/ml, at which level the drug remains efficacious.66 A rise in use of perhexiline as an adjunctive therapy for refractory angina has, therefore, been seen in some countries, particularly Australia, with good results.62 At plasma NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE 495 ©2006 Nature Publishing Group REVIEW www.nature.com/clinicalpractice/cardio levels within the therapeutic range, perhexiline is not negatively inotropic and does not alter systemic vascular resistance.67 We have demonstrated beneficial short-term effects of perhexiline in patients with ischemic or nonischemic heart failure in a double-blind, randomized, placebo-controlled trial.68 Patients taking optimum conventional medical therapy were randomized to perhexiline or placebo for 8 weeks, with dummy dose adjustment in the placebo group. We noted a large increase in the combined primary endpoint of peak oxygen uptake (approximate increase 3 ml kg–1 min–1) and left ventricular ejection fraction (approximate increase 10%; Figure 3), and a substantial improvement in the predefined secondary endpoint of symptomatic status as assessed by the Minnesota Living with Heart Failure Questionnaire. The study design involved separate randomization of the ischemic and nonischemic groups, permitting separate analysis of the primary endpoint in each group. Importantly, maximum oxygen uptake was similarly and significantly increased in the ischemic and nonischemic groups; therefore, the mechanism of benefit is not primarily anti-ischemic.68 This study, however, was short. Further work is required to show that the clinical benefit is maintained in the longer term, to investigate whether use of the agent leads to reverse remodeling (left ventricular end-systolic volume did not fall in this 8-week study), and, most importantly, to assess the effects on mortality and hospitalization. CONCLUSION Irrespective of cause, heart failure is associated with an energy deficit. Agents that cause a shift in the myocardial substrate used from free fatty acids towards glucose have an oxygen-sparing effect. Unsurprisingly, some of these agents are effective as antiangina therapies. A series of studies have demonstrated that the use of agents that alter substrate use might be useful in heart failure. Interestingly, perhexiline yields beneficial effects in both ischemic and nonischemic heart failure. Some of these agents are currently used in highly symptomatic patients with heart failure who are already receiving optimum medical therapy. Most of the available evidence on the use of these metabolic agents in humans is derived from small studies. Further larger-scale and longer-term human studies must be done before use of these drugs can be considered on a widespread basis. 496 NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE ©2006 Nature Publishing Group KEY POINTS ■ Emerging evidence shows that, irrespective of the etiology, an energetic impairment contributes to the pathogenesis of heart failure ■ Patterns of substrate use in heart failure are complex and depend on species, cause, duration, underlying coronary artery disease, endothelial dysfunction, and the presence of genetic and other comorbidities ■ Myocardial use of fatty acids costs more oxygen per unit of ATP generated than glucose ■ Animal models and small-scale human studies suggest benefits with the use of agents that shift myocardial substrate use from free fatty acids towards glucose, but larger human studies are needed References 1 Unverferth DV et al. (1988) Human myocardial adenosine triphosphatase activities in health and heart failure. Am Heart J 115: 139–146 2 Starling RC et al. (1998) Human myocardial ATP content and in vivo contractile function. Mol Cell Biochem 180: 171–177 3 Beer M et al. (2002) Absolute concentrations of highenergy phosphate metabolites in normal hypertrophied and failing human myocardium measured noninvasively with 31P-SLOOP magnetic resonance spectroscopy. J Am Coll Cardiol 40: 1267–1274 4 Shen W et al. (1999) Progressive loss of myocardial ATP due to a loss of total purines during the development of heart failure in dogs: a compensatory role for the parallel loss of creatine. Circulation 100: 2113–2118 5 Bittl JA and Ingwall JS (1985) Reaction rates of creatine kinase and ATP synthesis in the isolated rat heart. A 31P NMR magnetization transfer study. J Biol Chem 260: 3512–3517 6 Weiss RG et al. (2005) ATP flux through creatine kinase in the normal, stressed, and failing human heart. Proc Natl Acad Sci USA 102: 808–813 7 Tian R and Ingwall JS (1999) The molecular energetics of the failing heart from animal models—small animal models. Heart Failure Rev 4: 245–253 8 Zhang J and Bache R (1999) The molecular energetics of the failing heart from animal models—large animal models. Heart Failure Rev 4: 255–267 9 Nakae I et al. (2003) Proton magnetic resonance spectroscopy can detect creatine depletion associated with the progression of heart failure in cardiomyopathy. J Am Coll Cardiol 42: 1587–1593 10 De Sousa E et al. (1999) Subcellular creatine kinase alterations. Implications in heart failure. Circ Res 85: 68–76 11 Conway MA et al. (1991) Detection of low phosphocreatine to ATP ratio in failing hypertrophied human myocardium by 31P magnetic resonance spectroscopy. Lancet 338: 973–976 12 Neubauer S et al. (1997) Myocardial phosphocreatineto-ATP ratio is a predictor of mortality in patients with dilated cardiomyopathy. Circulation 96: 2190–2196 13 Gross WL et al. (1996) Nitric oxide inhibits creatine kinase and regulates rat heart contractile reserve. Proc Natl Acad Sci USA 93: 5604–5609 14 Andrews R et al. (1998) The effect of dietary creatine supplementation on skeletal muscle metabolism in congestive heart failure. Eur Heart J 19: 617–622 ABOZGUIA ET AL. SEPTEMBER 2006 VOL 3 NO 9 REVIEW www.nature.com/clinicalpractice/cardio 15 Arany Z et al. (2005) Transcriptional coactivator PGC-1α controls the energy state and contractile function of cardiac muscle. Cell Metab 1: 259–271 16 Sack MN et al. (2000) Coordinate regulation of metabolic enzyme encoding genes during cardiac development and following carvedilol therapy in spontaneously hypertensive rats. Cardiovasc Drugs Ther 14: 31–39 17 Stanley WC et al. (1997) Regulation of myocardial carbohydrate metabolism under normal and ischaemic conditions. Potential for pharmacological interventions. Cardiovasc Res 33: 243–257 18 Stanley WC et al. (2005) Myocardial substrate metabolism in the normal and failing heart. Physiol Rev 85: 1093–1129 19 Kagaya Y et al. (1990) Effects of long-term pressure overload on regional myocardial glucose and free fatty acid uptake in rats. A quantitative autoradiographic study. Circulation 81: 1353–1361 20 Alaoui-Talibi Z et al. (1997) Control of oxidative metabolism in volume-overloaded rat hearts: effect of propionyl-L-carnitine. Am J Physiol 272: H1615–H1624 21 Nikolaidis LA et al. (2004) The development of myocardial insulin resistance in conscious dogs with advanced dilated cardiomyopathy. Cardiovasc Res 61: 297–306 22 Lommi J et al. (1998) Free fatty acid kinetics and oxidation in congestive heart failure. Am J Cardiol 81: 45–50 23 Taylor M et al. (2001) An evaluation of myocardial fatty acid and glucose uptake using PET with [18F]fluoro-6thia-heptadecanoic acid and [18F]FDG in patients with congestive heart failure. J Nucl Med 42: 55–62 24 Randle PJ (1998) Regulatory interactions between lipids and carbohydrates: the glucose fatty acid cycle after 35 years. Diabetes Metab Rev 14: 263–283 25 Mansson S et al. (2005) 13C imaging—a new diagnostic platform. Eur Radiol 16: 57–67 26 Myrmel T et al. (1992) Triacylglycerol metabolism in hypoxic, glucose-deprived rat cardiomyocytes. J Mol Cell Cardiol 24: 855–868 27 Korvald C et al. (2000) Myocardial substrate metabolism influences left ventricular energetics in vivo. Am J Physiol Heart Circ Physiol 278: H1345–H1351 28 Boehm EA et al. (2001) Increased uncoupling proteins and decreased efficiency in palmitate-perfused hyperthyroid rat heart. Am J Physiol Heart Circ Physiol 280: H977–H983 29 Schrauwen P et al. (2003) Uncoupling protein 3 as a mitochondrial fatty acid anion exporter. FASEB J 17: 2272–2274 30 Murray AJ et al. (2004) Uncoupling proteins in human heart. Lancet 364: 1786–1788 31 Kjekshus JK and Mjos OD (1972) Effect of free fatty acids on myocardial function and metabolism in the ischemic dog heart. J Clin Invest 51: 1767–1776 32 Hermann HP et al. (1999) Haemodynamic effects of intracoronary pyruvate in patients with congestive heart failure: an open study. Lancet 353: 1321–1323 33 Kantor PF et al. (2000) The antianginal drug trimetazidine shifts cardiac energy metabolism from fatty acid oxidation to glucose oxidation by inhibiting mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res 86: 580–588 34 MacInnes A et al. (2003) The antianginal agent trimetazidine does not exert its functional benefit via inhibition of mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res 93: e26–e32 35 Szwed H et al. (2001) Combination treatment in stable effort angina using trimetazidine and metoprolol: results of a randomized, double-blind, multicentre SEPTEMBER 2006 VOL 3 NO 9 ABOZGUIA ET AL. 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 study (TRIMPOL II). TRIMetazidine in POLand. Eur Heart J 22: 2267–2274 Vitale C et al. (2004) Trimetazidine improves left ventricular function and quality of life in elderly patients with coronary artery disease. Eur Heart J 25: 1814–1821 Di Napoli P et al. (2005) Long term cardioprotective action of trimetazidine and potential effect on the inflammatory process in patients with ischaemic dilated cardiomyopathy. Heart 91: 161–165 Rosano GM et al. (2003) Trimetazidine improves left ventricular function in diabetic patients with coronary artery disease: a double-blind placebo-controlled study. Cardiovasc Diabetol 2: 16 Thrainsdottir IS et al. (2004) Effects of trimetazidine on left ventricular function in patients with type 2 diabetes and heart failure. J Cardiovasc Pharmacol 44: 101–108 McCormack JG et al. (1996) Ranolazine stimulates glucose oxidation in normoxic, ischemic, and reperfused ischemic rat hearts. Circulation 93: 135–142 Clarke B et al. (1996) Ranolazine increases active pyruvate dehydrogenase in perfused normoxic rat hearts: evidence for an indirect mechanism. J Mol Cell Cardiol 28: 341–350 McCullough PA (2005) Chronic angina: new medical options for treatment. Rev Cardiovasc Med 6: 152–161 Chandler MP et al. (2002) Short-term treatment with ranolazine improves mechanical efficiency in dogs with chronic heart failure. Circ Res 91: 278–280 Sabbah HN et al. (2002) Ranolazine, a partial fatty acid oxidation (pFOX) inhibitor, improves left ventricular function in dogs with chronic heart failure. J Card Fail 8: 416–422 Leotta G et al. (2005) Relationship between QT interval and cardiovascular risk factors in healthy young subjects. J Hum Hypertens 19: 623–627 Lionetti V et al. (2005) Carnitine palmitoyl transferase-I inhibition prevents ventricular remodeling and delays decompensation in pacing-induced heart failure. Cardiovasc Res 66: 454–461 Greaves P et al. (1984) Cardiac hypertrophy in the dog and rat induced by oxfenicine, an agent which modifies muscle metabolism. Arch Toxicol Suppl 7: S488–S493 Bachmann E and Weber E (1988) Biochemical mechanisms of oxfenicine cardiotoxicity. Pharmacology 36: 238–248 Abdel-aleem S et al. (1994) Regulation of glucose utilization during the inhibition of fatty acid oxidation in rat myocytes. Horm Metab Res 26: 88–91 Reaven GM et al. (1988) Additive hypoglycemic effects of drugs that modify free-fatty acid metabolism by different mechanisms in rats with streptozocininduced diabetes. Diabetes 37: 28–32 Turcani M and Rupp H (1999) Modification of left ventricular hypertrophy by chronic etomixir treatment. Br J Pharmacol 126: 501–507 Lopaschuk GD and Spafford M (1989) Response of isolated working hearts to fatty acids and carnitine palmitoyltransferase I inhibition during reduction of coronary flow in acutely and chronically diabetic rats. Circ Res 65: 378–387 Schmidt-Schweda S and Holubarsch C (2000) First clinical trial with etomoxir in patients with chronic congestive heart failure. Clin Sci (Lond) 99: 27–35 Bristow MR et al. (1996) Carvedilol produces doserelated improvements in left ventricular function and survival in subjects with chronic heart failure. MOCHA Investigators. Circulation 94: 2807–2816 NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE 497 ©2006 Nature Publishing Group REVIEW www.nature.com/clinicalpractice/cardio Competing interests Michael Frenneaux has applied for a patent for the use of perhexiline therapy in chronic heart failure patients. The other authors declared they have no competing interests. 55 Packer M et al. (1996) Double-blind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure. The PRECISE Trial Prospective Randomized Evaluation of Carvedilol on Symptoms and Exercise. Circulation 94: 2793–2799 56 Wallhaus TR et al. (2001) Myocardial free fatty acid and glucose use after carvedilol treatment in patients with congestive heart failure. Circulation 103: 2441–2446 57 Al Hesayen A et al. (2005) Selective versus nonselective β-adrenergic receptor blockade in chronic heart failure: differential effects on myocardial energy substrate utilization. Eur J Heart Fail 7: 618–623 58 Jeffrey FM et al. (1995) Direct evidence that perhexiline modifies myocardial substrate utilization from fatty acids to lactate. J Cardiovasc Pharmacol 25: 469–472 59 Kennedy JA et al. (1996) Inhibition of carnitine palmitoyltransferase-1 in rat heart and liver by perhexiline and amiodarone. Biochem Pharmacol 52: 273–280 60 Kennedy JA et al. (2000) Effect of perhexiline and oxfenicine on myocardial function and metabolism during low-flow ischemia/reperfusion in the isolated rat heart. J Cardiovasc Pharmacol 36: 794–801 498 NATURE CLINICAL PRACTICE CARDIOVASCULAR MEDICINE ©2006 Nature Publishing Group 61 Horowitz JD and Mashford ML (1979) Perhexiline maleate in the treatment of severe angina pectoris. Med J Aust 1: 485–488 62 Cole PL et al. (1990) Efficacy and safety of perhexiline maleate in refractory angina. A double-blind placebocontrolled clinical trial of a novel antianginal agent. Circulation 81: 1260–1270 63 Pessayre D et al. (1979) Perhexiline maleate-induced cirrhosis. Gastroenterology 76: 170–177 64 Bouche P et al. (1979) Perhexiline maleate and peripheral neuropathy. Neurology 29: 739–743 65 Morgan MY et al. (1984) Impaired oxidation of debrisoquine in patients with perhexiline liver injury. Gut 25: 1057–1064 66 Horowitz JD et al. (1986) Perhexiline maleate treatment for severe angina pectoris—correlations with pharmacokinetics. Int J Cardiol 13: 219–229 67 Klassen GA et al. (1976) Effects of perhexiline maleate on coronary flow distribution in the ischemic canine myocardium. Circulation 54: 14–20 68 Lee L et al. (2005) Metabolic modulation with perhexiline in chronic heart failure: a randomized controlled trial of short-term use of a novel treatment. Circulation 112: 3280–3288 ABOZGUIA ET AL. SEPTEMBER 2006 VOL 3 NO 9