* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cell-mediated (T cells)
DNA vaccination wikipedia , lookup
Immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adaptive immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Molecular mimicry wikipedia , lookup
Innate immune system wikipedia , lookup
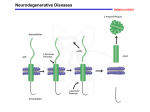
NADPH Oxidase 1 Mediates a-Synucleinopathy in Parkinson’s Disease 1 Cristovao et al., 2012 Journal of Neuroscience, 32(42):14465–14477 Accumulation of misfolded a-synuclein is the pathological hallmark of Parkinson’s disease (PD). Nevertheless, little is known about the mechanism contributing to asynuclein aggregation and its further toxicity to dopaminergic neurons. Since oxidative stress can increase the expression and aggregation levels of a-synuclein, NADPH oxidases (Noxs), which are responsible for reactive oxygen species generation, could be major players in synucleinopathy. Nox1 is expressed in dopaminergic neurons of the PD animal models as well as postmortem brain tissue of PD patients, and is responsible for oxidative stress and subsequent neuronal degeneration. Here, using paraquat (PQ)-based in vitro and in vivo PD models, we show that Nox1 has a crucial role in modulating the behavior of a-synuclein expression and aggregation in dopaminergic neurons. We observed in differentiated human dopaminergic cells that Nox1 and a-synuclein expressions are increased under PQ exposure. Nox1 knockdown significantly reduced a-synuclein expression and aggregation, supporting the role of Nox1 in this process. Furthermore, in rats exposed to PQ, the selective knockdown of Nox1 in the substantia nigra, using adenoassociated virus encoding Nox1-specific shRNA, largely attenuated the PQ-mediated increase of a-synuclein and a-synuclein aggregates. Significant reductions in oxidative stress level and dopaminergic neuronal loss were also observed. Our data reveal a new mechanism by which a-synuclein becomes a neuropathologic protein through Nox1mediated oxidative stress. This finding may be used to generate new therapeutic interventions that slow the rate of a-synuclein aggregation and the progression of PD. 2 3 HE RB I C I D E S PARAQUAT H3C + N+ N CH3 NADPH N A D P H - C Y T O C H R O M E C R E D U C R E D U C E D NADP P A R A Q U A T O2 -. O2 S U P E R O +X I D I D E + H 2O 2 +2 U T A S E S M O CH A T A L A S E H 2O P O L Y U N S A T U R A T E D S I N G 2L E T O F R E E S E L E N I L I P I D DF ER SE E R A D I V I G S H F i R E DGUS CHT AP S E E R O X I O X I NADPH g . D I 1 . Z E D L I P I G S H A L C O H O L S M e R A D I L I P I U M R E D U C E D H Y D GR SO HP E R O X I P E N T O SNADP E P A T H W A Y c h a n i s m L L I P I C A L S T A M I N C A D D E D A S E D M E M B R A N E F R E E R A D I C A L D A M A G E o f a c t i o n f o r t o x 4 Blood Cells - continued 5 • Two branches: innate/ nonspecific and adaptive/specific • In the innate system: mast cells, neutrophils and macrophages (engulf cytokines inflammation) • Within adaptive, two branches: humoral-mediated (B cells) and cell-mediated (T cells) • Macrophages have a role in both branches Source and differentiation of blood cells 7 T lymphocytes form.in b.m.& mature in thymus 1) T helper cells help B cells mature into plasma cells. CD4+T cells express CD4 protein on their surface 2)19% Cytotoxic T cells destroy viral infective & tumor cells 3)Memory Tcells CD4+(lost in AIDs) or CD8+(cytotoxic) subset of antigen T cells that persist long after infection. 4) Regulatory T cells (suppressor T cells) 5)Natural killer (NK) largest T cell.Interferons cause cytotoxic granule release 6) Antigen-presenting cell (APC) 8 B cells named from bursa of fabricius(birds) • Plasma cells are large B cells exposed to antigens which produce antibodies that bind to microbes. In tissues not plasma. • Contain rough e.r. & cell rapid apoptosis (short life) • Memory B cells formed from activ.B cells(long life) • 23% B-1 cells IgM>IgG in peritoneal & pleural cavities • B-2 cells 9 Immunosuppressants and anti-inflammatories RA • B cell depleting agents like rituximab • human monoclonal antibody against IL-6R cytokine 10 Biomarkers for determining oxidative stress associated with inflammation diseases • • • • • • • • • 1) Plasma lipid hydroperoxide 2) Oxidative DNA damage DNA 8-OHdQ Urinary 8-OHdQ Thymine oxidation HMdU DNA strand breaks (Comet assay) 3) Protein carbonyls using dinitrophenylhydrazine Protein oxidation - cysteine, methionine, histidine Protein AGEs 4) Fructose oxidation forms toxic glyoxal 11 • When a pathogen (can be self in this case) is ingested by a macrophage, pathogen proteins attach it to class II MHC • Macrophage activated to deliver signals to T-cells which produces autocrines and stimulate their own production • Helper T cells activate B cells which produce antibodies that inhibit the pathogens 12 • Results from a loss of immunological tolerance – which is the ability to ignore self-antigens • T and B lymphocytes that recognize self-antigens are usually destroyed in the Thymus and Bone marrow, respectively, preventing autoimmunity. • Infection and overstimulation of APCs can break tolerance and induce priming of T-cells • A combination of genetics and environment are responsible for autoimmune disease • Human Lymphocyte Antigen (HLA/MHC) is the best predictor as it enhances antigen presentation resulting in increased T-cell activation 13 Antibody-mediated (B cells) • • Binding of antigens on the surfaces of B-cells produces antibodies • • Autoantibodies: – Bind to self-tissue, and activates the complement cascade which targets the self-antigen to be phagocytosed (opsonized) by Macrophages Cell-mediated (T cells) Immune cells both kill cells directly and indirectly via cytokines (PG, NO, etc.) Macrophages: – INITIATE the response as antigen presenting cells – kill cells through antibody dependent cell-mediated cytotoxicity and by releasing cytokines (TNF and IL-1) – PRESENT SELF-TISSUE TO T CELLS 14 Biomarkers for inflammatory disease Pro-inflammatory cytokines • Elevated cytokines CRP,IL-1B,IL-1B,IL-6,IL-8 • Tumor necrosis factor alpha Autoimmune: • c-ANCA anti-neutrophil cytoplasmic stain (cytoplasmic) Proteinase 3 is the target antigen; Wegener’s granulomatosis • p-ANCA anti-neutrophil perinuclear stain; myeloperoxidase is the primary target antigen; vasiculitis, ulcerative colitis, RA • x-ANCA chronic inflammatory bowel disease