* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 投影片 1 - National Cheng Kung University
Monoclonal antibody wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Innate immune system wikipedia , lookup
Major urinary proteins wikipedia , lookup
Rheumatic fever wikipedia , lookup
DNA vaccination wikipedia , lookup
Molecular mimicry wikipedia , lookup
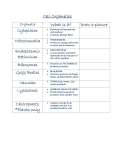
INFECTIOUS DISEASES Group A Streptococcus: Host Aspect Yee-Shin Lin, Ph.D. December 19, 2007 Outlines Introduction Pathogenesis and host responses Host-streptococcus interactions Innate immune responses Induction of inflammation and apoptosis Autoimmunity: post-infectious sequelae Autophagy Vaccinology Introduction A wide spectrum of diseases in humans Mild illness: pharyngitis / tonsillitis / otitis media / impetigo / scarlet fever Severe illness: necrotizing fasciitis / bacteremia / streptococcal toxic shock syndrome (STSS) Post-streptococcal sequelae: acute glomerulonephritis / rheumatic fever / reactive arthritis Pathogenesis and host responses Host-streptococcus interactions Effect of lactoferrin on up-regulation of expression of streptococcal pyrogenic exotoxin (Spe) A. Ability of HL-1 medium or its fraction with proteins ≧10 kDa to induce up-regulation of expression of streptococcal pyrogenic exotoxin (Spe) A and down-regulation of expression of SpeB. Graham et al. Group A Streptococcus transcriptome dynamics during growth in human blood reveals bacterial adaptive and survival strategies. Am J Pathol 2005, 166:456-465. Shelburne et al. Growth characteristics of and virulence factor production by group A Streptococcus during cultivation in human saliva. Infect Immun 2005, 73:4723-4731. Graham et al. Analysis of the transcriptome of group A Streptococcus in mouse soft tissue infection. Am J Pathol 2006, 169:927-942. Innate immune responses J. Allergy Clin. Immunol., 2007;120:13-22 Inhibition of PMN recruitment and phagocytosis (I) C5a peptidase (ScpA): Inhibit PMN recruitment IL-8 protease (ScpC) (Scp: streptococcal chemokine protease): Inhibit PMN recruitment M and M-like proteins: Bind to complement-regulating proteins (such as C4bp, factor H) and other plasma proteins (such as fibrinogen) (*) Inhibit C3b-mediated PMN binding Help to survive inside PMN or in NET (**) Streptococcal inhibitor of complement Sic: Bind to C5b-C7 to inhibit the formation of membrane attack complex (MAC) Bind to ezrin and alter PMN cytoskeleton function to inhibit phagocytosis Inactivate antibacterial peptides Inhibition of PMN recruitment and phagocytosis (II) IdeS/CD11b homolog Mac (cysteine protease): Bind to FcR and cleave IgG to inhibit PMN phagocytosis and killing SpeB (cysteine protease): Release C5a peptidase from the surface of GAS Cleave IgG and properdin to inhibit opsonophagocytosis EndoS (endoglycosidase): Hydrolyze the conserved asparagine-linked glycan on IgG to inhibit IgGmediated opsonophagocytosis Hyaluronic acid capsule: Act as a physical barrier to prohibit interaction of PMN with opsonins on bacterial surface Fig. 7. Working model for the inhibition of complement deposition by M proteins. Complement is activated via the classical pathway by S. pyogenes, potentially resulting in surface deposition of C3b. However, M protein (a dimeric coiled-coil protein) inhibits this deposition of C3b by recruiting a human plasma protein, which acts by reducing the formation or activity of the classical pathway C3 convertase. Some M proteins, such as M5, bind fibrinogen (Fg), while other M proteins, such as M22, recruit the ~570 kDa C4b-binding protein (C4BP), an inhibitor of the classical pathway. Importantly, the inhibition of complement deposition promotes resistance to phagocytosis. As indicated, the M22 protein (and many other M proteins) also binds IgA, which contributes to phagocytosis resistance by an unknown mechanism (Carlsson et al., 2003). Note that other S. pyogenes surface structures, not shown here, may also affect complement deposition and phagocytosis resistance. Induction of inflammation and apoptosis Inflammation, endothelial damage, multi-organ failure and shock M protein and SPE superantigen The Journal of Immunology, 2006, 177: 1221–1228. Autoimmunity: post-infectious sequelae Considerable insight has been gained into the etiopathogenesis of poststreptococcal glomerulonephritis since the landmark theoretical construct of Clemens von Pirquet postulated that disease-causing immune complexes were responsible for the nephritis that followed scarlet fever. Over the years, molecular mimicry between streptococcal products and renal components, autoimmune reactivity and several streptococcal antigens have been extensively studied. Recent investigations assign a critical role to both in situ formation and deposition of circulating immune complexes that would trigger a variety of effector mechanisms. Glomerular plasmin-binding activity of streptococcal glyceraldehyde-3-phosphate-dehydrogenase may play a role in nephritogenicity and streptococcal pyrogenic exotoxin B and its zymogen precursor may be the long-sought nephritogenic antigen. Kidney International (2007) 71, 1094–1104. Streptococcal pyrogenic exotoxin B is an extracellular cysteine protease. Only nephritis-associated strains of group A streptococci secrete this protease and this may be involved in the pathogenesis of post-streptococcal glomerulonephritis. Mice were actively immunized with a recombinant protease inactive exotoxin B mutant or passively immunized with exotoxin B antibody.Characteristics of glomerulonephritis were measured using histology, immunoglobulin deposition, complement activation, cell infiltration, and proteinuria. None of the mice given bovine serum albumin or exotoxin A as controls showed any marked changes. Immunoglobulin deposition, complement activation, and leukocyte infiltration occurred only in the glomeruli of exotoxin B-hyperimmunized mice. One particular anti-exotoxin B monoclonal antibody, 10G, was cross-reactive with kidney endothelial cells and it caused kidney injury and proteinuria when infused into mice. This cross-reactivity may be involved in the pathogenesis of glomerulonephritis following group A streptococcal infection. Kidney International (2007) 72, 716–724; doi:10.1038/sj.ki.5002407; Autophagy Vaccinology Vaccine development has emerged as a compelling example of the benefits of genomics. In the last five years, the traditional, linear process of testing antigens one at a time has been revolutionized by genome-scale, parallel strategies for discovering candidate antigens — an approach commonly referred to as “reverse vaccinology”. We describe a proteomic approach for identifying bacterial surface-exposed proteins quickly and reliably for their use as vaccine candidates. Whole cells are treated with proteases to selectively digest protruding proteins that are subsequently identified by mass spectrometry analysis of the released peptides. When applied to the sequenced 1_SF370 group A Streptococcus strain, 68 PSORT-predicted surface-associated proteins were identified, including most of the protective antigens described in the literature. The number of surface-exposed proteins varied from strain to strain, most likely as a consequence of different capsule content. The surface-exposed proteins of the highly virulent 23_DSM2071 strain included 17 proteins, 15 in common with M1_SF370. When 14 of the 17 proteins were expressed in E. coli and tested in the mouse for their capacity to confer protection against a lethal dose of M23_DSM2071, one new protective antigen (Spy0416) was identified. This strategy overcomes the difficulties so far encountered in surface protein characterization and has great potential in vaccine discovery.