* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Myasthenia gravis
Anti-nuclear antibody wikipedia , lookup
Germ theory of disease wikipedia , lookup
Behçet's disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Complement system wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Autoimmunity wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Myasthenia
gravis
אפידמיולוגיה
prevalence - 20 per 100,000
population-between 53,000 and 60,000
cases /USA
Pathophysiology of Myasthenia
Gravis
Pathophysiology of Myasthenia
Gravis
85% of patients with MG have detectable
serum antibodies against AChRs
20% to 40% of the remaining patients are
positive for anti-MuSK antibodies
about 10% of patients are doubleseronegative MG
anti-LRP4 autoantibodies exist in serum
samples of patients with doubleseronegative MG.
Autoantibodies in Myasthenia Gravis
Antigen
Anti-AChR
MG
Control
Human 85-90%
0
TE671 80%
Anti-Musk
2-5% of all MG, >20%
of AChR-SNMG
0
Anti-striated
muscle
Anti-thyroid
40%
4%
44%
14%
Anti-nuclear
14-39%
4%
Anti-titin (MGT30) 85% (MG+thymoma)
0
50% (MG+thymoma)
0
Anti-ryanodine
receptor
Evidence that MG is autoimmune
disease
MG Patients have increased incidence of other immunemediated diseases, such as rheumatoid arthritis
A transitory neonatal form of the disease occurs in MG.
Immunosuppressive treatment, including plasma
exchange, produces improvement in most patients
An animal model of MG can be produced by
immunization with purified AChR
Antibodies against human AChR are found in the serum
of most patients
Evidence that MG is autoimmune
disease
Myasthenic serum or IgG produces abnormal
neuromuscular transmission when injected into animals
IgG and complement components are attached to the
postsynaptic endplate membrane in myasthenic
Antibody-Mediated
Mechanisms
Accelerated degradation of AChRs
Complement-Mediated AChR-loss
Blockade of AChRs
Possible Origin of Autoimmunity in
MG
Cross reacting epitope
Idiotypic dysregulation
Abnormal antigen
Drug related antigen
Helper T-cell defect
Regulatory T-cell defect
AChR Seronegative Myasthenia
Gravis
10-15% of MG patients
Clinical presentation similar to
seropositive generalized MG
Thymus usually “normal”
Reduced-AChRs probably due to
antibodies, to another NMJ antigen, or
signal transduction effect on AChR
function
Autoimmune disorders applied to seropositive
and seronegative MG
Seropositive MG
Yes
Seronegative MG
No
Improvement after
plasma exchange
Yes
Yes
Defect transferable to
mice by Ig
Yes
Yes
NMT defect
Yes
Yes
AChR reduction
Yes
No
Antibody attached to AChR
Yes
No
Immunization against
antigen(s)
Produces disease
Not yet clear
AChR antibodies
Transfer features
AChR-positive MG (85-90%)
AChR-negative MG:
– MuSK positive (around 20-40%)
– MuSK negative (double negative)
Clinical Presentation
Ptosis or diplopia was the initial symptom
in two thirds
Almost all have both within 2 years of
disease onset
Difficulty chewing, swallowing, or talking is
the initial symptom in one sixth of patients
and limb weakness in one tenth.
Weakness typically fluctuates during
the day .
Clinical Presentation:
Disease course
MG is variable but usually progressive
Restricted to the ocular muscles in 10%-40% of
patients
Maximum weakness occurs during the first year
in two thirds of patients.
Before corticosteroids were used for
treatment, approximately one third of patients
had spontaneous improvement, one third had
progressive disease, and one third died of the
disease.
Factors that worsen myasthenic
symptoms
Emotional upset,
Systemic illness (especially viral
respiratory infections).
Hypothyroidism / hyperthyroidism.
Pregnancy, the menstrual cycle,
Drugs affecting neuromuscular
transmission
Fever.
Physical Findings
Ocular Muscles -Asymmetrical weakness
of several muscles in both eyes is typical.
Ptosis is usually asymmetrical and varies
during sustained activity
Oropharyngeal Muscles changes in the
voice, difficulty chewing and swallowing
Limb Muscles Neck flexors are usually
weaker than neck extensors, deltoids,
triceps, and wrist/fingers extensors are
often weaker than other muscles.
OCCULAR SYMPTOMES
Weakness usually involves one or more ocular muscles
without overt pupillary abnormality
Weakness is typically variable, fluctuating, and fatigable
After down gaze, upgaze produces lid overshoot ("lid
twitch").
Pseudo-internuclear ophthalmoplegia-limited adduction
is present, with nystagmoid jerks in abducting eye.
In asymmetrical ptosis, covering the eye with the ptotic
lid may relieve contraction of the opposite frontalis.
Passively lifting a ptotic lid may cause the opposite lid to
fall.
Cold applied to the eye may improve lid ptosis.
קקליניקה
• חולשת שרירים
מתקדמת:
העפעפיים
והעיניים ,פנים,
דיבור ,בליעה,
צוואר ,גפיים,
נשימה
• myasthenic
crisis
• תימומה
Clinical association of MuSK abs
Distinct population
Age at onset around third decade
More women than men
More bulbar patients
Response to plasma exchange
Incidence 20-40% of AChR negative MG
(Possible additional plasma factor involved ?)
The Thymus in Myasthenia
Gravis
Breakdown in immune tolerance toward selfantigens in the thymus.
10% of patients with MG have a thymic tumor
most are benign.
70% have hyperplastic changes (germinal
centers) that indicate an active immune response
Virtually all patients with MG and thymoma have
elevated concentrations of AChR-binding
antibodies
Diagnostic Procedures-1
Edrophonium Chloride (Tensilon) Test
positive in more than 90% of patients with
MG
Tensilon Test is not unique to MG
A dose of 2 mg is injected intravenously,
and the response is monitored for 60
seconds. Then 3 and 5 mg.
Diagnostic Procedures-2
Electromyography
10% decrement in amplitude when the first
stimulus is compared to the fourth or fifth
SFEMG is the most sensitive clinical test
of neuromuscular transmission and shows
increased jitter .
Diagnostic Procedures-2
Treatment
Cholinesterase Inhibitors- Mestinon 3060 mg/4-8/day
Corticosteroids 75% of patients markdly
improved ! Prednisone 1.5-2.0 mg/kg per day
Immunosuppressant DrugsPlasma Exchange ,IVIG
Thymectomy
Treatment-2
Azathioprine
Onset action: 4-8
side effects: allergic reaction,hepatic toxicity,
leukopenia
Cyclosporin Onset action: 2-3 renal toxicity,
hypertension, multiple potential drug interactions
Cyclophosphamide Onset action: variabl
side effects: leukopenia, hair loss, cystitis
Efficacy of PE in myasthenia
gravis: Hadassah experience
86 myasthenic patients were treated
with repeated courses of PE (ranging
from 6-126 exchanges during a period
of 3 years)
The follow up period was 3 years
During this period the efficacy of PE
was evaluated: the response rate was
over 85 % of patients (improved).
Myasthenia gravis:
Myasthenic crisis
Before Plasmapheresis
After Plasmapheresis
Current therapy of myasthenia gravis
What do we treat patients with MG when the conventional
therapy fails?
mAb therapy for neuro-inflammatory
diseases
Monoclonal antibodies (mAbs) represent an
emerging and rapidly growing field of therapy in
neuro-inflammatory diseases .
Most of them have been developed in systemic
autoimmune diseases and Oncology.
There are currently more the 240 mAbs in clinical
development
mAb therapy for neuro-inflammatory
diseases
Monoclonal antibodies mode of action:
Depletion of specific cells
Blocking specific molecules expressed on the cell
membrane
Neutralizing soluble serum factors
Monoclonal Abs directed at specific
immunologic aspects of MG
Abnormal B cells activation
Complement activation
BAFF disregulation
Helper and Regulatory T-cell defect
Monoclonal Abs directed at specific
immunologic aspects of MG.
Dalakas , Ann N Y Acad Sci, 2012
Examples of Therapeutic Monoclonal Antibodies
Name
Antigenic target
Clinical use
Muromomab
CD3
Transplant rejection
Daclizumab
CD25
Transplant rejection,adult
T-
cell leukemia
Rituximab
CD20
Infliximab
TNF
Crohn’s disease, RA
CD52
CLL,MS
TNF
RA
CD11a
Psoriasis
Natalizumab
ABT-874
-4 integrin
Anti IL-12
MS, Crohn’s disease
Not yet identified
Toralizuma
CD40L, CD154
ineffective in SLE
No candidate
Non Fc-binding
Not yet identified
Eculizumab
Anti-C5
paroxysmal nocturnal hemoglobinuria
and atypical hemolytic-uremic
syndrome
Abatacept
36
Anti-CTLA4
ineffective in SLE
Alemtuzumab
Adalimumab
Efalizumab
B-cell lymphoma,
AUTOIMMUNITY
Targeting B-cells
AChR + MG is the prototypic antibody mediated
disease with clear evidence that AChR antibodies
induce the disease in animal models and in humans.
Both AChR and MuSK antibody positive patients
respond to plasma exchange.
Anti-MuSK patients do not appear to respond to
IVIg.
Anti-MuSK antibodies are IgG4 which do not activate
complement.
Anti-AChR are IgG1 and IgG3 that activate complement.
Targeting B-cells
B-cell targeting therapies:
Rituximab
Ocrelizumab
Ofatumumab
Rituximab: Anti-CD20
Target
CD-20 receptor
Other names
Mabthera Rituxan, and Zytux
Rationale
B cells involvement in autoimmune diseases –
antibody mediated , B cells role as APCs and
cytokines production
Mode of action The antibody binds to CD20 expressed on B cells, from early
pre-B cells to later in differentiation, but absent on terminally
differentiated plasma cells. eliminates nearly all CD20expressing B cells by CDC and ADCC as well as induction of
apoptosis
Safety and
tolerability
Severe infusion reaction, cardiac arrest,
Infections – PML.
Resistance development, most likely due to less efficient antibody-
39
dependent cytotoxicity or to generation of human antichimeric antibodies
(HACA).
The role of B-cell activating factor
(BAFF) in myasthenia gravis
B-cell activating factor (BAFF) is important in the
differentiation and maturation of B cells and plasma cells.
Although the mechanism(s) by which BAFF and its receptors
help regulate B-cell function and tolerance is not known, it
may play a significant role in the immune process involved in
myasthenia gravis.
Serum BAFF levels were found to be significantly higher in
MG patients compared to controls including those with MS
There was no correlation to disease severity but a trend for
levels to be higher in AChR + patients.
There is also evidence that BAFF is upregulated in germinal
follicle like structures in myasthenic thymuses.
Belimumab : Anti-BAFF
Target
BAFF
Other names
Anti-BAFF
Rationale
BAFF- is important in the differentiation and
maturation of B cells and plasma cells
Mode of action
inhibits BAFF action via binding circulating BAFF and
reducing the number of circulating B-cells but not to
the extent as rituximab
Safety and
tolerability
approved in the US, Canada and Europe for the treatment
of systemic lupus erythematosis
41
A phase II trial in rheumatoid arthritis was
encouraging but no phase III trial is underway. A
phase II trial in MG has been announced
Therapy that targets complement
Complement mediated damage to the postsynaptic junction has been demonstrated to
bind to the AChR-antibody complex inducing
membrane-attack-complex damage to the
membrane reducing post-synaptic folds,
widening the synaptic cleft and reducing the
numbers of receptors.
Eculizumab : Anti-C5
Target
complement protein C5
Other names
Soliris
Rationale
Complement mediated damage to the post-synaptic junction has
been demonstrated to bind to the AChR-antibody complex inducing
membrane-attack-complex damage to the membrane reducing
post-synaptic folds, widening the synaptic cleft and reducing the
numbers of receptors.
Mode of action
a recombinant humanized monoclonal IgG 2/4 antibody that binds
to complement protein C5 which prevents the generation of the
terminal complement C5b-9 complex
Safety and
tolerability
nausea, back pain, nasopharyngitis, and headache
vulnerable to infection with encapsulated
organisms. meningococcal vaccination is recommended at
least 2 weeks prior to receiving eculizumab
43
Agents targeting T cell intracellular
signaling pathways, and costimulation
IL-2 mediate cell proliferation and differentiation.
Daclizumab binds to CD25 (IL-2 receptor antagonist) and
inhibits T cell proliferation.
Daclizumab is very well tolerated, has been approved for
one form of leukemia, and has been very promising in
patients with multiple sclerosis in at least two clinical trials.
Daclizumab An excellent agent to consider for MG
Daclizumab: Anti-CD25
Target
IL-2 receptor chain (CD25)
Other names
Anti-CD25, Zenapax®
Rationale
IL-2 mediate cell proliferation and differentiation.
Mode of action
Prevents IL-2 binding without triggering of complement- or
cell-mediated cell depletion, modulation of the IL-2 receptor
complex or induction of intracellular signaling events
a marked expansion of regulatory CD56bright NK cells
Safety and
tolerability
Gastrointestinal (e.g. nausea, diarrhoea),
metabolic and nutritional disorders
45
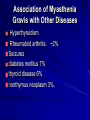
Association of Myasthenia
Gravis with Other Diseases
Hyperthyroidism
Rheumatoid arthritis. ~2%
Seizures
diabetes mellitus 7%
thyroid disease 6%
nonthymus neoplasm 3%,
Transitory Neonatal Myasthenia.
10-20% of newborns of MG mothers
frequency and severity correlate with
antibody level
Hypotonia and poorly fed during the first 3
days. symptoms may be delayed for 1-2
days. Usually last less than 2 weeks but
may continue for as long as 12 weeks.
Genetic Myasthenic Syndromes
not immune mediated
2:1 male predominance.
ophthalmoparesis and ptosis during
infancy. Limb weakness is usually mild
compared with ophthalmoplegia.
Respiratory distress is unusual.
ChE inhibitors improve limb muscle
weakness in many forms of congenital
genetic myasthenia
Lambert-Eaton Myasthenic
Syndrome
A pre-synaptic abnormality of ACh release
In association with malignancy, usually small cell lung
cancer (SCLC).
Abs against the voltage-gated calcium channels
(VGCCs) on nerve terminals
reduced tendon reflexes and enhanced by repeated
muscle contraction or repeated tapping of the tendon.
autonomic dysfunction :dry mouth, impotence and
postural hypotension.
Treatment with Guanidine hydrochloride increases the
release of ACh
Drug alert for patients with
myasthenia gravis
Interferon-α, botulinum toxin, and d-penicillamine should never be
used in myasthenic patients.
The following drugs produce worsening of myasthenic weakness
in most patients who receive them. Use with caution and monitor
patient for exacerbation of myasthenic symptoms.
–
Succinylcholine, d-tubocurarine, or other neuromuscularblocking agents
–
Quinine, quinidine, and procainamide
–
Aminoglycoside antibiotics, particularly gentamicin,
kanamycin, neomycin, and streptomycin
–
Beta blockers (systemic and ocular preparations): propranolol,
timolol maleate eyedrops
–
Calcium-channel blockers
–
Magnesium salts (including laxatives and antacids with high
Mg2+ concentrations)
–
Iodinated contrast agents
Many other drugs are reported to exacerbate the weakness in
some patients with MG. All patients with MG should be observed
for increased weakness whenever a new medication is started.
BOTULISM
A toxin produced by the anaerobic bacterium,
Clostridium botulinum,
Blocks the release of ACh from the motor nerve terminal
Intoxication usually follows ingestion of contaminated
foods that were inadequately sterilized
First Nausea and vomiting and then neuromuscular
symptoms 12-36 hours after ingestion
Clinical symptoms:
blurred vision, dysphagia, and dysarthria.
Pupillary responses to light are impaired.
tendon reflexes are variably reduced.
Fatal respiratory paralysis may occur rapidly.
Autonomic dysfunction, such as dry mouth, constipation,
or urinary retention in most.