* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Review
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Review
Inferior and Superior Vena Cave RA Tricuspid Valve Pulmonic Valve
Pulmonary Artery Lungs {oxygenation} Pulmonary Vein Left Atrium
Mitral Valve Left Ventricle Aortic Valve Circulation
Sodium Enters; Potassium leaves Depolarization
RELATIONSHIP OF THE ECG TO ELECTRICAL
EVENTS IN THE HEART
P wave- PR interval- QRS complex - ST segment- Twave
Normal
0.12 – 0.20
Upright
Only before
each QRS
morphology normal
<0.12 seconds
isoelectric
= NSR
present
RELATIONSHIP OF THE ECG TO ELECTRICAL
EVENTS IN THE HEART
Any deviation from the normal electrical
rhythm of the heart
= Dysrhythmia
RELATIONSHIP OF THE ECG TO ELECTRICAL
EVENTS IN THE HEART
Causes of dysrhythmias:
• MI, ischemia, necrosis
• Autonomic nervous system imbalance
• Distension of the chambers
notably in the arteries secondary to CHF
• Blood gas abnormalities i.e. hypoxia and abnormal pH
• Electrolyte imbalances
• Trauma {cardiac contusion}
• Drug effects and drug toxicity
• Electrocution
• Hypothermia
• CNS damage
• Idiopathic events: arising spontaneously or from an obscure or unknown cause
•
Normal occurances
RELATIONSHIP OF THE ECG TO ELECTRICAL
EVENTS IN THE HEART
The absence of cardiac electrical activity
= arrhythmia
RELATIONSHIP OF THE ECG TO ELECTRICAL
EVENTS IN THE HEART
ANALYZING RATE
• ECG strip method or 60 second method
• “300” method or triplicate method
• R-R method
CARDIAC EMERGENCIES
What’s next:
• Bringing It Home
• Cardiac arrest lecture
• Mega code practice and scenarios
• Exams
written
Mega code
BRINGING IT HOME
Cardiac Anatomy and Physiology
• Flow of blood through the heart and
cardiac conductive system
• Composition of Blood
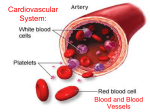
Composition of the Blood
•
•
•
•
Plasma
Red blood cells
White blood cells
Platelets
Flow of blood
Arteries – arterioles - veinules - veins
Major Blood Vessels
• Superior Vena Cava
• Carotid Arteries
• Jugular Veins
• Aorta
• Femoral Artery
• Inferior Vena Cava
• Brachial Arteries
Circulation of Blood between:
• Heart and lungs
• Heart and rest of the body
• Mechanical and Electrical functions of the
heart in relation to pulse and blood pressure
• Shock
Cardiac Compromise
Acute Coronary Syndrome
Syndrome: In medicine and psychology, the term
syndrome refers to the association of several
clinically recognizable features, signs (observed by a
physician), symptoms (reported by the patient),
phenomena or characteristics that often occur
together, so that the presence of one feature alerts
the physician to the presence of the others.
Cardiac Compromise:
• Any kind of problem with the heart
• May lead to a high index of suspicion for
possible:
MI
Angina
CHF
Signs and Symptoms of Cardiac
Compromise:
• Dyspnea
• Pain, pressure or discomfort
• Palpations
• Sweating
• N&V
• Anxiety
• Abnormal Pulse
• Blood Pressure:
Hypotensive: <90/systolic
Hypertensive: >150/systolic or
>90/diasolic
• Chest Pain
Causes of Cardiac Compromise:
• CAD
Atherosclerosis
Arteriosclerosis
Hardening of the arteries from
Ca++ deposits
• Restriction of blood through the artery
Thrombus; clot and debris from plaque
Occlusion: Thrombus cuts off
blood flow
Embolism: Thrombus that moves
to occlude the flow of
blood beyond the
blockage
Risk Factors:
• Heredity
• Age
• HTN
• Obesity
• Lack of exercise
• Elevated cholesterol and triglycerides
• Smoking
• Common Symptom
Chest Pain
• Aneurysm
Electrical Malfunctions of the Heart
• Dysrhythmia
Mechanical Malfunctions of the Heart
• Pump Failure
Angina Pectoris
Chest Pain
• Difference between Angina & MI
• NTG
• AMI
Sudden death is considered a cardiac arrest
within 2 hrs. of symptoms
Risk Factors
• CAD
• Chronic respiratory problems
• Unusual exertion
• Severe emotional stress
Treatment
• Fibrinolytics
• Angioplasty or Catheterization
• ASA regimen
CHF
Left sided heart failure/ Right sided failure
soon follows
Causes:
• Diseased heart valves
• HTN
• COPD
• As a complication of an MI
Pulmonary Edema
• Rales
• Blood tinged sputum
• Pedal Edema
• Abdominal Distension
Signs and symptoms of CHF
CARDIOGENIC SHOCK
• Tachycardia
• Dyspnea
• Normal to elevated B/P
• Cyanosis
• Diaphoresis
• Cool Clammy skin
•
•
•
•
•
Pulmonary Edema
Anxiety or confusion due to hypoxia
Pedal edema
JVD (late sign)
ABD distension
Enlarged liver and spleen
• Medication History
Lasix
PATIENT CARE
• POC
• O2
• Identify Priority Patient
No history of cardiac problems
Hx but no NTG
Hypotensive
• Transport: Thoughtful, calm, caring fashion
ASSIST with NTG
• Clinical signs and symptoms must be present
• Right med, route, dose, form, patient
• Pulse rate >50 and <100
Protocol
• Systolic B/P >110
• Has not taken Viagra or such within 48 to 72 hrs.
• Medical Control
• Remember usual protocol is 1 does q 5
minutes to 3 doses.
• CHECK BLOOD PRESSURE BEFORE
ADMINISTERING
CARDIAC EMERGENCIES
LET’S
PLAY