* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Nursing and heart failure
Echocardiography wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac arrest wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
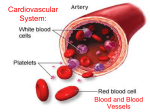
Nursing and heart failure Congestive Heart Failure (CHF) or cardiac failure, is one of the most common causes of in-hospital mortality for patients with cardiac diseases. It is the second most common complication after myocardial infarction (MI). Men are affected more than women. The 5 year mortality rate for men is 60% and about 45% for women. The aim for nurses - to improve patient outcomes and quality of patient’s life - to decrease hospital admissions and, therefore, cost Definition Congestive Heart Failure indicates the inability of the heart to pump enough blood to meet the body’s metabolic requirements for oxygen and nutrients leading to discrepancies between myocardial oxygen supply and demand. PATHOPHYSIOLOGY Changes in: - heart rate stroke volume contractility preload afterload Compensatory Mechanisms - ADRENERGIC MECHANISM - RENAL MECHANISM (RENIN-ANGIOTENSINALDOSTERON SYSTEM) - VENTRICULAR HYPERTROPHY ETIOLOGY - coronary heart disease long-standing hypertension cardiomyopathy valvular dysfunction, valvular diseases inflammatory or degenerative cardiac muscle diseases Precipitating factors - cessation of cardiac drug intake dysrythmias fever hypoxia hypoxemia anemia respiratory and/or metabolic acidosis electrolyte imbalance CLASSIFICATION - - - Right-Sided Cardiac Failure Left-Sided Cardiac Failure Forward Cardiac Failure (inability of the right and left ventricles to pump blood into the pulmonary and systemic circulation, respectively. It occurs due to increased pressure in the arterial system (afterload) causing decreased cardiac output and hypoperfusion of vital organs. This frequently occurs with aortic stenosis and/or systemic hypertension) Backward Cardiac Failure (inadequacy of the ventricles to empty the blood into the arterial circulation. This causes accumulation of fluid and elevation of pressure (e.g. increasing in all chambers of the heart and in the venous system behind the affected ventricles). Myocardial infarct and cardiomyopathy causes decreased systolic ejection which can lead to backward CHF) Acute and Chronic Cardiac Failure Low ventricular output (infarction, hypotension, cardiomyopathy or hemorrhage) and high ventricular output (fever, thyrotoxicosis, anemia, pregnancy) CHF Assessment Parameters - Respiratory Assessment - Cardiovascular Assessment (including capillary wedge pressure) - Renal Function Assessment - Peripheral Assessment - CNS Assessment Laboratory Result Analysis - arterial blood gases - liver function tests - kidneys function tests Pharmacological Management - Increasing Oxygen Supply - Decreasing Oxygen Demand (Positive Inotropic Agents) – cardiac glycosides - Negative chronotropic agents (betablockers, calcium channel blockers) - Reducing afterload and preload (nitrates, hydralazine, angiotensinconverting enzyme (ACE) inhibitors) - Diuretics (Thiazides, Loop Diuretics) Nursing Interventions - Promoting Rest - Promotion of Tissue Perfusion (moderate daily exercise, adequate oxygen administration as ordered, and diuresis) - Fluid and Dietary Considerations Patient Education Patient teaching is one of the most important factors in nursing management of congestive heart failure. Recurrent episodes of cardiac failure are often due in part to noncompliance, such as failing to follow medication therapy, straying from dietary guidelines, missing medical appointments, engagement in excessive and unregulated exercise, and failing to recognize recurring symptoms. Topics which should be covered in teaching include: gradual increase in activity as tolerated, which should be discontinued when symptomatic; medication actions, side effects, dosage, scheduling, administration, and signs of toxicity; encouragement of medical follow ups; report of any untoward symptoms that could indicate worsening of the condition (shortness of breath, nocturnal dyspnea, productive cough, ankle edema, anginal pain, palpitations, and extreme fatigue); maintaining weight; sodium and fluid restriction; prevention of infection, and avoidance of coffee and tobacco, which increase the workload on the heart by increasing sympathetic stimulation and causing vasoconstriction.