* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiac muscle tissue
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Rheumatic fever wikipedia , lookup
Coronary artery disease wikipedia , lookup
Jatene procedure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
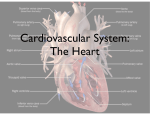
Heart walls – 3 distinct layers: 1 - endocardium - innermost layer; epithelial tissue that lines the entire circulatory system 2 - myocardium - thickest layer; consists of cardiac muscle 3 - epicardium - thin, external membrane around the heart. Cardiac muscle tissue: striated ( consists of sarcomeres just like skeletal muscle) cells contain numerous mitochondria (up to 40% of cell volume) adjacent cells join end-to-end at structures called intercalated discs which is cell membrane separate indivisual cardiac muscle from one another. Intercalated discs contain two types of specialized junctions: desmosomes (hold the cells tightly together) and gap junctions (which permit action potentials to easily spread from one cardiac muscle cell to adjacent cells). Cardiac muscle tissue forms 2 functional syncytia or units: the atria being one & the ventricles the other. Because of the presence of gap junctions, if any cell is stimulated within a syncytium, then the impulse will spread to all cells. In other words, the 2 atria always function as a unit & the 2 ventricles always function as a unit. However, there are no gap junctions between atrial & ventricular contractile cells. In addition, the atria & ventricles are separated by the electrically nonconductive tissue that surrounds the valves. So, as will be discussed later, a special conducting system is needed to permit transmission of impulses from the atria to the ventricles In cardiac muscle, there are two types of cells: contractile cells & autorhythmic (or automatic) cells. Contractile cells, of course, contract when stimulated. Autorhythmic cells, on the other hand, are self-stimulating & contract without any external stimulation. The action potentials that occur in these two types of cells are a bit different: 0n the left is the action potential of an autorhythmic cell; on the right, the action potential of a contractile cell. Autorhythmic cells exhibit PACEMAKER POTENTIALS. Depolarization is due to the inward diffusion of calcium . &it begins when: the slow calcium channels open, Repolarization is due to the outward diffusion of potassium • In contructile cell • depolarization is very rapid & is due to the inward diffusion of sodium . • repolarization begins with a slow outward diffusion of potassium, but that is largely offset by the slow inward diffusion of calcium . So, repolarization begins with a plateau phase. Then, potassium diffuses out much more rapidly as the calcium channels close , and the membrane potential quickly reaches the 'resting' potential . Most of the muscle cells in the heart are contractile cells. The autorhythmic cells are located in these areas: Sinoatrial (SA), or sinus, node Atrioventricular (AV) node Atrioventricular (AV) bundle (also sometimes called the bundle of His) Right & left bundle branches Purkinje fibers Various automatic cells have different 'rhythms': SA node - 60 - 100 per minute (usually 70 - 80 per minute) AV node & AV bundle - 40 - 60 per minute Bundle branches & Purkinje fibers - 20 - 40 per minute SA node = has the highest or fastest rhythm &, therefore, sets the pace or rate of contraction for the entire heart. As a result, the SA node is commonly referred to as the PACEMAKER. Spread of cardiac excitation ( Conducting System of the Heart): Begins at the SA node & quickly spreads through both atria Also travels through the heart's 'conducting system' (AV node > AV bundle > bundle branches > Purkinje fibers) through the ventricles For efficient pumping: The atria should contract (& finish contracting) before the ventricles contract. This occurs because of AV nodal delay (that is, the impulse travels rather slowly through the AV node & this permits the atria to complete contraction before the ventricles begin contraction). The atria should contract as a unit, & the ventricles should contract as a unit. This occurs because the impulse spreads so rapidly that all myocardial cells in the atria and ventricles, respectively, contract at about the same time. The impulse spreads rapidly through the ventricles because of the conducting system. Refractory period of contractile cell Lasts about 250 msec (almost as long as contraction period) The long refractory period means that cardiac muscle cannot be restimulated until contraction is almost over & this makes summation (& tetanus) of cardiac muscle impossible. This is a valuable protective mechanism because pumping requires alternate periods of contraction & relaxation; prolonged tetanus would prove fatal Coronary artery disease (CAD) is a condition in which plaque builds up inside the coronary arteries that supply heart muscle with oxygenrich blood. Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. When plaque builds up in the arteries, the condition is called atherosclerosis. Plaque narrows the arteries and reduces blood flow to your heart muscle. It also makes it more likely that blood clots will form and partially or completely block blood flow. When coronary arteries are narrowed or blocked, oxygen-rich blood can't reach the heart muscle. This can cause angina or a heart attack. Angina is chest pain or discomfort that occurs when not enough blood flows to an area of heart muscle. A heart attack occurs when blood flow to an area of heart muscle is completely blocked. This prevents oxygen-rich blood from reaching that area of heart muscle and causes it to die. Without quick treatment, a heart attack can lead to serious problems and even death. Over time, CAD can weaken heart muscle and lead to heart failure and arrhythmias. Heart failure is a condition in which your heart can't pump enough blood throughout your body. Arrhythmias are problems with the speed or rhythm of your heartbeat. CAD is the most common type of heart disease • Heart Valves: • Atrioventricular (AV) valves - prevent backflow of blood from ventricles to atria during ventricular systole (contraction) – Tricuspid valve - located between right atrium & right ventricle – Mitral valve - located between left atrium & left ventricle • Semilunar valves - prevent backflow of blood from arteries (pulmonary artery & the aorta) to ventricles during ventricular diastole (relaxation) – Aortic valve - located between left ventricle & the aorta – Pulmonary valve - located between right ventricle & the pulmonary artery (trunk) • All valves consist of connective tissue (not cardiac muscle tissue) and, therefore, open & close passively. Valves open & close in response to changes in pressure: • AV valves - open when pressure in the atria is greater than pressure in the ventricles (i.e., during ventricular diastole) & closed when pressure in the ventricles is greater than pressure in the atria (i.e., during ventricular systole) • Semilunar valves - open when pressure in the ventricles is greater than pressure in the arteries (i.e., during ventricular systole) and closed when pressure in the pulmonary trunk & aorta is greater than pressure in the ventricles (i.e., during ventricular diastole • What happens in the heart during each 'mechanical' event: – Atrial systole : • no heart sounds (because no heart valves are opening or closing) • a slight increase in ventricular volume because blood from the atria is pumped into the ventricles – Ventricular systole: • the first heart sound (lub) (labeled S1 below) - this sound is generated by the closing of the AV valves (& this occurs because increasing pressure in the ventricles causes the AV valves to close) • initially there is no change in ventricular volume (called the period of isometric contraction) because ventricular pressure must build to a certain level before the semilunar valves can be forced open & blood ejected. Once that pressure is achieved, & the semilunar valves do open, ventricular volume drops rapidly as blood is ejected Heart valve disease is a condition in which one or more heart valves don't work properly, making the heart work harder and affecting its ability to pump blood. Malfunctioning heart valves can create two basic problems: (1) Regurgitation, or backflow, occurs when a valve doesn’t close tightly. Blood leaks back into the chamber rather than flowing forward through the heart or into an artery. Backflow is most often due to prolapse (the flaps of the valve flop or bulge back into an upper heart chamber during a heartbeat). 2) Stenosis occurs when the flaps of a valve thicken, stiffen, or fuse together. This prevents the heart valve from fully opening, and not enough blood flows through the valve. heart valve disease coulde be congenital or acquired later in life. Although a valve may be normal at first, disease can cause problems to develop over time. Many people have heart valve defects or disease, but don't have symptoms, and not cause any problems. For other people, the condition can worsen slowly over time until symptoms develop. If not treated, advanced heart valve disease can cause heart failure, stroke, blood clots, or sudden death due to cardiac arrest. Lifestyle changes and medicines can relieve many of the symptoms and problems linked to heart valve disease, and can also lower the risk of developing a lifethreatening condition, such as stroke or sudden cardiac arrest. Eventually, however, faulty heart valves may have to be repaired or replaced