* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ECG Interpretation
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Heart arrhythmia wikipedia , lookup
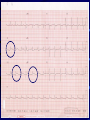
ECG Interpretation What is an ECG • Electrocardiogram • Traces the electrical activity of the heart • 12 lead, 15 lead Uses of ECG Tracing • • • • • • Ischemia/infarct Arrhythmias Ventricular and atrial enlargements Conduction defects Pericarditis Effects of some drugs and electrolytes ECG How to Conduct an ECG 1. 2. 3. 4. 5. Patient lies flat on back Electrodes are placed on the body Sites may need to be shaved or cleaned to ensure the leads will stick properly. Patient will lie as still as possible, hold breath, or put hands under bottom to keep from moving. The results are then printed out on paper for MD to review. ECG Strip Lead Placements • • • • • • • V1 - Junction of the 4th ICS, Right sternal border V2 - Junction of the 4th ICS, Left sternal border V3 - Midway between V2 and V4 V4 - Junction of 5th ICS, Mid clavicle V5 - Anterior aspect of axilla, same line as V4 V6 - Mid axilla, same line a V4 4 limb leads (for grounding etc) Lead Placements Cont’ Normal Conduction Pattern Understanding the Waves Each wave • • • • • P Q R S T ECG Strip r/t heart Understanding the Waves • One small box = 0.04 seconds • One large box = 0.2 seconds • 5 large boxes = 1 second http://en.wikipedia.org/wiki/File:ECG_principle_slow.gif Understanding the Waves • Baseline (what is it?) • P wave – Length of time it takes the impulse to pass from the SA node to the AV node – Should precede every QRS wave • PR interval – Should be no longer than 0.12 – 0.2 Understanding the Waves • QRS – Should be no longer than 0.12 – If energy is going towards a positive electrode (camera), the picture will show a positive QRS complex – If energy is going away from positive electrode, the picture will show a negative QRS complex – If energy is toward the positive electrode and then passes by it, the QRS will be biphasic – Ventricle contracting Understanding the Waves • T wave – Should always start from baseline – Will indicate ischemia Understanding an ECG • Is as easy as… 1. 2. 3. 1. = rate 2. = intervals 3. = rhythm Step 1 = Rate • Different ways to calculate a rate: – a) ECG usually tells you – b) Locate a QRS that is close to a big line and count to next big line: 300, 150, 100, 75, 60, 50 – c) take a 6 second strip, count QRS and multiply by 10 (hint: the middle of V3 on the lead II strip is 6 seconds) Step 1 = Rate (cont’) • Checking the regularity: – map out QRS’s Step 2 = Intervals • We assess intervals to see where the impulse is coming from (pacemaker beat) • Remember: – PR interval: normal is 0.12 - 0.2 – QRS interval: normal is less than or equal to 0.12 Step 3 = Rhythm The biggest question in relation to rhythm is… Is this rhythm affecting my patient? (Normal) Sinus Rhythm • 60-80 bpm • P preceding each QRS • Normal intervals Normal ECG Other Sinus Rhythms • Sinus bradycardia – a sinus rhythm with a rate <60 bpm Other Sinus Rhythms • Sinus tachycardia – a sinus rhythm with a rate >80 bpm Atrial Arrhythmias • Atrial fibrillation (A-fib) – irregular rate – no discernable P waves – increased risk of strokes due to clots that might form due to fibrillation (patients are usually on anticoagulation therapy) Atrial fibrillation Atrial Arrhythmias Cont’ • Atrial flutter – saw tooth in appearance – irregular rate Atrial flutter Blocks • 1st degree AV block – a PR interval that exceeds 0.20 sec Blocks Cont’ • 2nd degree AV block (Mobitz) – a) type I (Wenckebach) • longer and longer PR intervals until a QRS is dropped Blocks Cont’ – b) type II • P waves and then suddenly a QRS is dropped • P’s are regular Blocks Cont’ • 3rd degree AV block – HR <40 bpm – a complete block of electrical activity from atria to ventricle – P’s are regular Ventricular Rhythms • Ventricular fibrillation – complete breakdown of all rhythm – a) course – b) fine V-fib • What’s the first thing to do when coming up on a patient with this rhythm? Ventricular Rhythms Cont’ • Ventricular tachycardia (V-tach) – impulse originates in the ventricle – always has a wide QRS complex V-tach What’s the first thing to do when coming up on a patient with this rhythm? Asystole • Pulseless Coronary Arteries MI’s MI’s MI’s • How can you tell on an ECG that your patient is having a heart attack? • T waves • Different views of heart will show different injured areas of heart MI’s • T wave shouldering is classic MI’s • How else can you tell that your patient has had an MI? • Cardiac Markers – CK will show in 4-6 hours (starts to come back down after 1 day) – Troponin will show in 4-6 hours (may stay elevated for weeks) – Others are: LDH, CK-MB, myoglobin, AST Locating an MI Area Leads Artery Complications Inferior II, III, aVF Right coronary Bradycardia Anterior V1, V2, V3, Left anterior Pulm edema, V4 descending hypotensive Lateral I, aVL, V5, V6 Circumflex I Lateral (circumflex) aVR V1 Anterior (Lt ant desc) V4 Anterior II Inferior (Rt coronary) aVL Lateral V2 Anterior V5 Lateral III Inferior aVF Inferior V3 Anterior V6 Lateral ECG Tissue Damage Locations Where is this MI?