* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter V Thorax
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Rheumatic fever wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Artificial heart valve wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Aortic stenosis wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
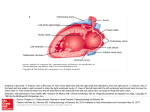
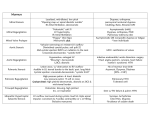
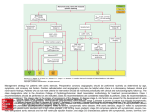
Chapter V Thorax D. Heart and blood vessels Heart Part II by Dr. Zhuo-ren Lu IV. Auscultation A. A routine procedure of auscultation includes heart rate, rhythm, cardiac sound, extra heart sound, cardiac murmur and pericardial friction sound. 1. Auscultatory valve area (1) The mitral valve area is in the 5th left intercostal space, 1 or 2 cm medial to the midclavicular line or the apical impulse area particularly in pathological cases. (2) The pulmonary valve area is in the second left intercostal space just lateral to the sternum. (3) The aortic area is located in the second right intercostal space just lateral to the sternum. (4) The second aortic area is in the 3rd or 4th left intercostal space lateral to the sternum. (5) The tricuspid valve area is located at the left or right side of the junction of the xiphoid process and the sternum. The routine procedure of auscultation is recommended as counterclockwise direction: apex pulmonary valve area aortic valve area second aortic valve area tricuspid valve area. 2. Heart rate (HR) and rhythm The heart rate normally varies with age, sex and physical activity. In adults, it usually varies from 60 to 100 beats per minutes. The rate is increased (tachycardia) in severe anemia, high fever, hyperthyroidism, heart failure and various types of arrhythmia. The HR above 160 beats/min indicates that the supraventricular tachycardia. The heart rate may be decreased (bradycardia) in increased intracranial pressure, obstructive jaundice, syncopy, complete heart block, and most cases of sick sinus syndrome. l There may be a pulse deficit (HR pulse rate) in atrial fibrillation(Af), which constitutes a grossly irregular rhythm and extremely variable in heart sound. Normally, the rhythm of the heart beat is regular or slight irregular during respiration with no clinical importance, and any deviation from this regularity is termed arrhythmia. The most common cause of the arrhythmia is premature contraction (extrasystole). It may occur as the result of excessive smoking or alcoholic intake, and also in some organic heart diseases. In bigeminal beats it is coupled or occurs in pair, with the second beat usually being weaker. In trigeminal beats, there is a pause after every third beat. 3. Heart sounds (1) The first heart sound (S1 ) l It is mainly produced by closure of both the mitral and tricuspid valves. The mitral valve closure precedes slightly that of the tricuspid valve. l S1 is synchronous with the apical impulse and corresponds with the onset of ventricular systole. (2) The second heart sound (S2 ) l It is produced by closure of both the aortic and pulmonary valves. Normally, aortic valve closure precedes pulmonary valve does. l Normally, P2 A2 in children and young persons, P2 A2 in old persons, and P2 A2 in mid-age persons. The differentiation between S1 and S2: There is a longer pause between S2 and the subsequent S1 (diastole) than between S1 and S2 (systole). S2 is usually clearly audible in the pulmonary valve area. S2 is higher in frequency and shorter in duration than S1. It may identify S1 by synchronous palpation at the apex or over the carotid artery. (3) The third heart sound (S3) (S3) Being low in both frequency and intensity, it is best heard with the bell of the stethoscope. It occurs during the phase of early diastolic filling after S2. This sound is heard in most children and some adults. (4) The fourth heart sound (S4) Like the third sound, S4 is also low in frequency and intensity, and is best heard at the apex. The sound occurs late in diastole and is related to atrial contraction. It is rarely heard under normal condition. A. Changes of intensity (1) All heart sounds In some patients with pulmonary emphysema or a very muscular chest wall, all heart sounds may be distant. (2) S1 The principal factor responsible for the intensity of is the position of the atrioventricular valve at the onset of ventricular contraction. l A loud S1 may be heard in mitral stenosis because less filling from left atrium to left ventricle and then the mitral valve in a lower position at the moment of ventricular contraction. l Tachycardia, anemia, fever, exercise, and hyperthyroidism may be associated with an intensity of S1. l A lower S1 may be caused by the illness of myocardium. (3) S2 l S2 becomes louder with hypertension or pulmonary artery hypertension. l A decrease in intensity of S2 over the aortic and/or pulmonary valve area may be caused by the damaged integrity and activity of the related semilunar valve. B. Splitting of heart sounds (1) A widely splitting of S1 at the apex suggests commonly the possibility of right boundle branch block because the second component of S1 delays. (2) Splitting of S2 is of great practical importance. It is the results of the marked asynchrony between the aortic valve and pulmonary valve closure. Because of the normal increase in venous return to the right side of the heart on inspiration, the right ventricle requires a slight longer period to empty itself. Normal splitting: in pulmonary valve stenosis and pulmonary artery hypertension and CRBBB, the splitting of S2 is clearly audible with inspiration. Fixed splitting: in ASD, there is a wide fixed split of S2 over the pulmonary valve area with little or no change in the degree of splitting during either phase of respiration. Paradoxical splitting: in CLBBB, the order of valve closure may be reversed. On expiration, pulmonary closure occurs first and is followed by aortic valve closure. During inspiration the pulmonary valve closure is normal delayed, with increased filling on the right side of the heart, and the two components then move closer together on inspiration. C. Extra heart sounds Diastolic extra heart sounds: gallop rhythm (ventricular gallop, atrial gallop, summation gallop), opening snap, pericardial knock Systolic extra heart sounds: systolic ejection sounds and ejection clicks (1) Gallop rhythm The term refers to that condition in which three and occasionally four heart sounds are spaced to audibly resemble the canter of a horse. The protodiastolic (ventricular gallop) is a brief lowpitched sound, usually heard near the end of the first third of diastole. It is the pathologic counterpart of the third heart sound and occurs at the time of rapid diastolic ventricular filling. The ventricular gallop sound is produced by an overdistension of the ventricle in the rapid filling phase of diastole, associated with an increase in ventricular diastolic volume and pressure. Ventricular gallop is usually heard at the apex in ventricular failure from any cause. Presystolic (atrial gallop) l It is associated with systolic overloading of ventricles where the ventricular diastolic pressure is elevated, namely, in systemic or pulmonary hypertension and in aortic or pulmonary stenosis. l The atrial gallop may also occur wherever the distensibility of the ventricle is impaired, such as MI, hypertension, and myocardiopathy. l It may even precede the signs of left ventricular hypertrophy. The atrial gallop sound is low-pitched, of short duration, and is best heard when the bell of the stethoscope is applied lightly to the chest wall. Quadruple rhythm When both the ventricular and atrial gallop sounds are present, this results in a quadruple rhythm. Summation gallop If both the ventricular and atrial gallop sounds are present and the heart rate increases, the diastolic interval shortens and the extra sounds come closer together. They may actually fuse, resulting in a summation gallop. (2) Opening snap The opening snap occurs soon after S2 and is produced by opening of the atrioventricular valves. l In mitral stenosis, the valve forms a restrictive diaphragm, which bulges into the left atrium during systole and then springs into the left ventricle when atrial pressure suddenly exceeds ventricular diastolic pressure. l This sound is brief in duration and higher in pitch than other gallop sounds. l It is heard best in the left 3rd and 4th parasternal areas with the patient in left lateral position. (3) Pericardial knock In the presence of constrictive pericarditis, at times an extra sound is heard in diastole occurring shortly after S2. It occurs earlier in diastole than the ventricular gallop does. Pericardial knock is higher in frequency and transmitted widely than opening snap. It is heard best in the apex or the left lower parasternal area. (4) Systolic ejection sounds and ejection clicks Pulmonary ejection clicks may occur in stenosis of the pulmonary valve, in pulmonary hypertension, and in that situation where the pulmonary artery is dilated. They are best heard over the pulmonary auscultatory valve area. Aortic ejection clicks occur in stenosis of the aortic valve, aortic regurgitation, aneurysm of the ascending aorta, and hypertension with dilatation of the aorta. They are heard over the base of the heart as well as at the apex. Some middle and late systolic clicks occur just prior to or during a late systolic murmur. The systolic click is probably related to the prolapsed mitral valve with longer chordae or exuberant leaflets. Following the termination of the prolapse, the late murmur is a reflection of late systolic mitral regurgitation. It is referred to as mitral valve prolapse syndrome (middle and late systolic clicks - late systolic mitral regurgitation). 4. Cardiac murmurs Cardiac murmurs are abnormal sounds produced by vibrations within the heart itself or in the walls of the large arteries. Murmurs are definitely longer in duration than heart sound, and are clearly audible with different qualities. A. Mechanism of production 1. Increasing the rate or velocity of blood flow 2. Decrease in the diameter of a heart valve or a constriction in one of the major arteries 3. Valve insufficiency 4. The abnormal communication between the right and left sides of chambers 5. By inserting a taut membrane (vegetation, ruptured chordae) 6. By a sudden increase in the diameter of a major vessel (aneurysm). B. Characterization of murmurs (1) Location The described location of a murmur is the site of precordium where it is audible most significantly. Murmurs of valvular origin are usually best heard auscultatory valve areas. over their respective (2) Timing Systole and diastole may be divided into three parts: early, middle, and late. Murmur may occur one part of systole or diastole, but at times may persist throughout systole. Certain systolic murmurs are produced by insufficiency of the mitral and tricuspid valves or by stenosis of the aortic and pulmonary valves. Most diastolic murmurs are the results of stenosis of the mitral and tricuspid valves or insufficiency of aortic and pulmonary valves. The most common lesions encountered are mitral stenosis, mitral and aortic insufficiency. (3) Quality On occasion the quality of cardiac murmurs may be of assistance in arriving at a more accurate diagnosis. l A blowing systolic murmur is often produced in mitral or tricuspid insufficiency and atrial or ventricular septal defect. l The mid- and late diastolic murmurs caused by mitral stenosis increase in intensity and assume a rumbling quality. l High-pitched blowing murmurs may resemble the sound of a whistle and at times are musical in character (vegetation or ruptured chordae). (4) Intensity l A grade I murmur is barely audible. l A grade II murmur is usually readily heard and slight louder than grade I. l Grade III and IV murmurs are quite loud. l Grade IV is often accompanied by a thrill. l Grade V is even more pronounced, and also accompanied by a thrill. l A grade VI murmur is so loud that even it may be heard with the stethoscope just removed from the chest wall. l Grade I and II are frequently encountered in persons without organic heart disease, whereas those of grade III intensity or louder seldom occur in a normal heart. l In clinic, diastolic murmurs are not graded because most of them occur in organic heart diseases. (5) Transmission Some murmurs are transmitted with or in the direction of the bloodstream by which they are produced. l The murmur of aortic regurgitation may be heard distinctly down along the left border of the sternum and over the apex. l The murmur caused by aortic stenosis may be audible over the carotid arteries. L The murmur of mitral regurgitation may transmit with the direction to left axilla. C. Classification of murmurs (1) Systolic murmurs Ejection murmurs is short in duration. They begin after S1, attain a peak in early or middle systole, and terminate before S2. Examples of systolic ejection murmurs are those in aortic stenosis and pulmonary stenosis, including the vast majority of so-called functional murmurs. Pansystolic murmurs It is of longer duration than the ejection murmur and usually obscures S1 and S2. l Mitral pansystolic murmurs are high-pitched, blowing in character, and frequently radiate toward the left axilla. Pansystolic murmurs are usually associated with mitral regurgitation, tricuspid regurgitation and VSD. l Murmurs that originate on the right side of the heart frequently increase in intensity during the course of inspiration. This fact may assist in differentiating tricuspid from mitral regurgitation and also in distinquishing between pulmonary and aortic ejection murmurs. Functional systolic murmur is commonly heard in children and young adults without any structural abnormality or recognizable heart disease. It is characteristically soft, blowing or ejection in quality, early, short, limited area, slight in intense (grade I or II), and variable. It is usually heard best at the pulmonary valve area and apex. Functional murmur varies with position and respiration. (2) Diastolic murmurs Regurgitant diastolic murmur is early in onset, beginning immediately after S2, is longer in duration, and is pandiastolic in nature. l The murmur of aortic regurgitation is highpitched, sighing or splashing in character, and transmitted along the left lower sternal border or the direction to the apex. l Regurgitant diastolic murmur also may occur in pulmonary regurgitation. Ventricular filling murmurs are low-pitched diastolic murmurs. In true mitral stenosis there is a definite delay in emptying of the left atrium. Austin Flint murmur Relative stenosis of the mitral or tricuspid valve may occur in mitral regurgitation, aortic regurgitation, and in some cases of congenital heart disease with left-to-right shunt. This murmur is less intense and shorter in duration than its organic counterpart. The nonobstructed mitral valve with higher position becomes relatively stenotic with respect to accommodating this large volume of blood. Graham Steell murmur A soft diastolic murmur may be heard over the pulmonary auscultatory valve area. It is caused by the relative regurgitation of the pulmonary valve owing to the dilatation of pulmonary artery when mitral stenosis exists. (3) Continuous murmurs The prototype of a continuous murmur is the Gibson murmur of patent ductus arteriousus. It is heard maximally under the left clavicle. 5. Pericardial friction rub l This to-and-fro rubbing be heard over the entire precordial region or a very small area. l It may be heard in both phases of the cardiac cycle. Pericardial friction rub is unaffected by respiration and is thus differentiated from a pleural friction rub. l It is also increased as pressing the stethoscope firmly against the patient’s chest wall. l A rub may be readily heard at one moment and be absent several minutes later. l The intensity of the rub is usually increased when the subject is sitting upright and leaning forward.