* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download A. Penicillins
Survey
Document related concepts
Transcript
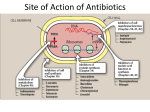
Dr. Bilal Aljaidi Antibacterial agents: Antibiotic: any substance produced by a microorganism that is antagonistic to the growth of other microorganisms (mainly bacteria) in high dilution (Waksman 1942). Antimicrobial agent: is a substance that kills or inhibits the growth of microorganisms such as bacteria, fungi, or protozoans. Either kills the microbe (microbiocidal) or prevent its growth (microbiostatic). covers both antibiotics and synthetic agents Antibacterial agents: Infection is the colonization of the host organism with a microorganism like bacteria, parasite, virus, or even a macro organism like fungi and macro parasites such as worms and nematodes. The microorganism then will use the host resources to reproduce and grow that results in a disease. Host system normally use the immune system to fight against the invading organism, first by the innate immune system, then by the adaptive immune system. History of Antibacterial agents: The presence of bacteria was first identified in 167o by Van leeuwenhoek. Pasteur was the first who link the bacteria to disease in 1800. Lister introduced carbolic acid as antiseptic and sterilizing agent for the operating wards. Koch identified that some bacteria is responsible for specific infections such as tuberculosis, cholera and typhoid History of Antibacterial agents: Paul Ehrlich “ the father of chemotherapy” developed the principle of chemotherapy: a chemical could directly interfere with the proliferation of microorganism at a concentration tolerated by the host .. This was named the magic pullet.. Which is nowadays called the selective toxicity. In 1910, Ehrlich had developed the first synthetic antibacterial agent; Salvarsan, which is active against protozoa especially trypanosoma. History of Antibacterial agents: In 1934, Proflavine was used in the wound infections, due to its systemic toxicity, it did not used systemically. In 1935, Prontosil was discovered as effective antibacterial agent in vivo. later found to be a prodrug that release sulfanilamide as the active metabolite: History of Antibacterial agents: Sulfonamides were the only effective antibacterial agents until the discovery of Penicillins in 1940. Streptomycin was discovered in 1945 and used against tuberculosis and other gram –ve bacteria, then lead to the discovery of other aminoglycosides. Streptomycin History of Antibacterial agents: Chloramphenicol and tetracycline antibiotics were discovered in 1947. In 1955, Cephalosporins were discovered. Many synthetic antibacterial agents were prepared later such as quinolones (1962), Flourinated quinolones (1980),Linezolid (2000) and other sulfonamide derivatives with a broad spectrum activity. The extensive studies on the bacterial cell components, genome and metabolic pathways considerably helped in better understanding the essential metabolic stages that are important for the growth and proliferation of the bacterial cells, which means that targeting these pathways might result in killing or attenuating the bacterial growth. Also the absence of certain essential bacterial metabolic pathways means that targeting such reaction could result in selective bacterial killing without harming human cells and result in safe antibacterial agents Bacterial cell Is a prokaryotic cell. Differ significantly from eukaryotic cells: 1-10 µm length whereas eukaryotic length is 10-100 µm Has no nucleus. Circular DNA, no chromosomal structure. Most of the organelles are simpler that eukaryotics. Characteristic cell wall which differ from bacteria to another, but generally, it is thick and fatty envelope which protect the bacterial cell from lysis and invading by external environment. Potential targets for antibacterial agents Protein synthesis Nucleic acid synthesis Cell metabolism (e.g. folate synthesis) Cytoplasmic membrane Bacterial cell wall synthesis Potential targets for antibacterial agents Sulfonamides (on metabolic enzymes) Penicillins Cephalosporins Aminoglycosides Tetracycline Chloramphenicol Quinolones Rifampicin Penicillins Cephalosporins Cell wall Monobactams synthesis Carbapenems Cycloserine Vancomycin Teicoplanin Bacitracin RNA elongation Dactinomycin Ansamycins Protein synthesis (tRNA) Cytoplasmic membrane structure Polymixins Mupirocin Protein synthesis (30S inhibitors) Tetracyclines Aminoglycosides Antibacterial agents acting on the cell wall biosynthesis Penicillins and Cephalosporins b-lactam antibiotics A 5-membered thiazolidine ring 6-membered dihydrothiazine B Penicillin nucleus Carbon atom C Cephalosporin nucleus D monocyclic Carbapenem nucleus Monobactam nucleus Penicillins Penicillins Highly strained structure due to the presence of bicyclic fused system composed from four membered lactam ring fused to the five membered thiazolidine ring. Bacteria synthesizes penicillin using cysteine, valine and some of the fermentation products: Penicillins Difficult to synthesize in the lab due to: The unstable highly strained ring system. The three chiral centre it has which should be with certain stereochemistry. Beechams was successfully isolated the biosynthetic precursor; 6-APA that was used as an intermediate for the synthesis of most of the semisynthetic penicllins. The bacterial cell wall Peptidoglycan = a vital component of bacterial cell walls, responsible for its shape and integrity Peptidoglycan = macromolecule made of sugar (glycan) chains cross-linked by short peptide bridges The nature of the peptidic cross links varies among bacteria but the essential mechanism is similar The bacterial cell wall Peptidoglycan N-acetylglucosamine (NAG) Gram – Only two layers of peptidoglycan Gram + Consists of 50-200 peptidoglycan layers Transpeptidase Involved in crosslinking N-acetylmuramic acid (NAM) D-alanine + D-ala D-ala (natural substrate) Penicillins Bacterial cell lysis Excellent selective toxicity Penicillin-enzyme complex cross-linking inhibited The wall become fragile and can no longer prevent the cell from swelling and bursting Penicillin mimic the structure of D-ala-D-ala, because of that the transpeptidase mistakenly bind to it instead of D-ala-D-ala. Also this explains the lack of penicillin toxicity, since D-amido acids are not present in human, only the Lamino acids present. Also targeting the cross linking in the peptidoglycan biosynthesis which is only present in bacteria explains the selective toxicity. Structure-activity relationships of penicillins (SAR) The strained β-lactam ring is essential. The free carboxylic acid is essential (the carboxylate ion binds to the charged nitrogen of the lysine at the active site. The bicyclic system is essential. The acylamino side chain is essential. Sulfur is not essential. The stereochemistry of the bicyclic ring with respect to the acylamino side chain is important. Structure-activity relationships of penicillins Acid sensitivity of penicillins Acid sensitivity of penicillins Three reasons for the acid sensitivity of penicillin G: Ring strain: due to the large angle and torsional strain exist, acid catalyzed ring opening will relief these strains. A highly reactive β-lactam carbonyl group: This amide bond is exceptionally unstable compared to the normal amide (why?).. The stabilization of the amide bond by the resonance is impaired here due to the increase in the ring strain that will be formed after the delocalization of the nitrogen lone pair to form a double bond within the four memeberd lactam ring Acid sensitivity of penicillins The effect of the acyl side chain: It has a self-destructive mechanism in which the oxygen of the carbonyl group will attack the carbonyl carbon of the lactam ring causing the ring opining just like the attack of water previously mentioned. This gives Penillic acid and penicillenic acid as final products (explain the mechanism of formation?) Acid resistant Penicillins To reduce the acid instability of penicillins: We can not change the β-lactam. We can not change the bicyclic system and its ring strain. The only thing that can be modified is the acyl group in order to reduce the self destructive mechanism (How?). This can be done by decreasing the nucleophilicity of the carbonyl oxygen which can be done by adding electron withdrawing group. Acid resistant Penicillins β-lactamase (Penicillinase): The wide spread use of penicillin G led to the increase in the number of resistant strains, especially in S. aureus. The main mechanism of resistance is the production and secretion of β-lactamase enzyme. β-lactamase is a mutated version of transpeptidase which is closely related in structure, especially in the active site. This means that β-lactamase will interact with penicillin structure in the same manner as transpeptidase. β-lactamase can hydrolyze 1000 penicillin molecule per second because the cleaved penicillin will leave the active site to react with other molecule. β-lactamase (Penicillinase): Gram +ve bacteria normally release β-lactamase to outside of the cell that will cleave penicillin before reaching the bacteria. Gram –ve bacteria release β-lactamase into the periplasmic space, which again will cleave penicillin before reaching the plasma membrane. Penicillin has to reach the plasma membrane where the transpeptidase present to do its antibacterial action. 95% of S.aureus became resistant to penicillins Most of gram –ve bacteria are β-lactamase producing bacteria β-lactamase (Penicillinase): There are various types of β-lactamase enzymes: Some are selective against penicillins (penicillinase). Some are selective against cephalosporins (cephalosporinase). Some are non-selective, acting on penicillins and cephalosporins at the same time. β-lactamase resistant Penicillins Structural modification has to be made to penicillin structure to prevent the binding to β-lactamase active site. This was a difficult task since β-lactamase and transpeptidase have a very similar active site. The only successful modification was by adding bulky group at the acyl side chain (Steric Shield), but not too bulky because this proved to reduce penicillin activity. β-lactamase resistant Penicillins 95% of S.aureus in hospitals became resistant to methicllin (MRSA) which in turns are resistant to most of the older generation penicillins Isoxazoyl Penicillins Effective against β-lactamase producing strains. Acid stable due to the electron withdrawing effect of the isoxazole ring. Used against S.aureus resistant bacteria. Broad Spectrum Penicillins Factors affecting the extent of penicillin activity: Chemical structure. The ability to cross the cell wall. Their susceptibility to β-lactamase . Their affinity to transpeptidase enzymes. Broad Spectrum Penicillins Chemical modification to get broad spectrum penicillins: 1. 2. Addition of hydrophobic group at the acyl side chain found to improve activity against gram +ve but reduce it against gram –ve bacteria. The addition of hydrophilic group at the acyl side chain causes a reduction in activity. Broad Spectrum Penicillins 3. Activity on gram –ve enhanced when a hydrophilic group was added at the -carbon in the acyl side chain, such in ampicillin and amoxicillin. This polar groups help the penicillin to pass through the porines that exist in the cell envelope of the gram – ve bacteria Ampicillin and amoxicillin Broad spectrum penicillins. Acid resistant penicillins (why?). Sensitive to β-lactamase (why?). Poorly absorbed through the mucus memebrane, this is due to the fact that they formed a zwitter ionic molecule at physiological pH (they contain a carboxylic acid and an amino group in their structure. The oral bioavailability can be improved by masking one of them, mainly the carboxylic acid…. By preparing a prodrug esters. Ampicillin prodrugs The methyl ester did not give the same improvement in absorption and activity (why?). Ureidopenicillins They all have a urea group at the -carbon in the acyl side chain. They have better activity compared to amoxicillin and they are more resistant to β-lactamase. Used parenterally for gram –ve infections especially P.aeruginosa. the ureido group though to mimic Some of the peptidoglycan structure, which means that it can bind to penicillin-binding protein Carboxypenicillins They have a carboxylic acid at the -carbon of the acyl side chain. They have broad spectrum activity.











































![ch 14 remember thing[1]](http://s1.studyres.com/store/data/008375860_1-2c45a3b285ef35d04828b346253789f0-150x150.png)