* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PPT
Psychedelic therapy wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug design wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Psychopharmacology wikipedia , lookup
Drug discovery wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Neuropharmacology wikipedia , lookup
Dydrogesterone wikipedia , lookup
Pharmacokinetics wikipedia , lookup
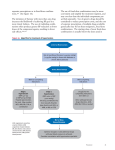
PHARMACOLOGY OF HYPERTENSION VICKI GROO, PHARM.D. CLINICAL ASSOCIATE PROFESSOR CLINICAL PHARMACIST, HEART CENTER [email protected] 413-0928 OBJECTIVES Classify hypertension and define treatment goals Be able to describe the pharmacology of oral antihypertensives with considerations in drug choice and compelling indications Be able to describe the pharmacology of intravenous antihypertensives used in the treatment of hypertensive emergency CLASSIFICATION Normal Prehypertension Hypertension Stage 1 Stage 2 SBP < 120 120-139 and or DBP < 80 80-89 140-159 ≥ 160 or or 90-99 ≥ 100 **Adults (18 yo) **Avg of 2 readings, 2 mins apart, on 2 occasions Secondary HTN only accounts for 5-10% of population JAMA 2003;289:2560-2572 EPIDEMIOLOGY 31% of US population with HTN 30% of US population with pre-HTN Present in: • 69% of patients who present with 1st MI • 77% of patients who present with 1st stroke • 74% of patients with heart failure Only 47% have BP under control http://www.cdc.gov/bloodpressure/facts.htm NATIONAL HEALTH & NUTRITION EXAMINATION SURVEY 2007-2008 81% 73% 50% TREATMENT GOALS JNC-7 REDUCE MORBIDITY AND MORTALITY Measurable goal: • Prehypertension: <120/80 • HTN w/ diabetes or renal disease: <130/80 • Others: <140/90 Minimize/ control other CV risk factors Reduce/ minimize adverse drug effects JAMA 2003;289:2560-2572 AHA BP TARGETS 2007: For prevention and management of ischemic heart disease: *Don’t worry about learning these for now. They may change Circulation 2007:115:2761-88 ALGORITHM FOR TREATMENT OF HYPERTENSION Lifestyle Modifications Not at Goal Blood Pressure (<140/90 mmHg) (<130/80 mmHg for those with diabetes or chronic kidney disease) Initial Drug Choices Without Compelling Indications With Compelling Indications Stage 1 Hypertension Stage 2 Hypertension (SBP 140–159 or DBP 90–99 mmHg) Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination. (SBP >160 or DBP >100 mmHg) 2-drug combination for most (usually thiazide-type diuretic and ACEI, or ARB, or BB, or CCB) Not at Goal Blood Pressure Optimize dosages or add additional drugs until goal blood pressure is achieved. Consider consultation with hypertension specialist. JNC VII JAMA 2003;289:2560-2572 Drug(s) for the compelling indications Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed. DRUG THERAPY CONSIDERATIONS Clinical trial data Over 2/3 of patients will require ≥2 drugs Cost/ adverse effects JAMA 2003;289:2560-2572 Limit salt intake Physical activity Lifestyle Modifications DASH eating Plan Lose weight Limit alcohol intake PHARMACOLOGY OF ANTIHYPERTENSIVES Diuretics: • Deplete sodium thereby decreasing blood volume Agents that block production or action of angiotensin • Reduce peripheral vascular resistance • Potentially ↓ blood volume Sympathoplegic agents: • ↓ peripheral vascular resistance • Inhibit cardiac function • ↑ venous pooling in capacitance vessels Direct vasodilators: • Relax vascular smooth muscle, thus dilating resistance vessels DIURETIC MOA DIURETIC COMPARISON HCTZ CTD Indapamide benzothiadiazine thiazide-like Non-thiazide sulfonamide VD 2.5 L 3-13 L 25 L T½ 8-15 hours 45-60 hours 14 hours duration 16-24 hours 48-72 hours 24 hr SBP (-) 7.4 ± 1.7 (-) 12.4 ± 1.8 PM BP (-)6.4 ± 1.8 (-) 13.5 ± 1.9 P = 0.054 and 0.009 for 24 hr and pm BP respectively Hypertension 2004;43:4-9, Indapamide DIURETIC CONSIDERATIONS K Dose Other 1st line choice Thiazides: Hydrochlorothiazide ↓ 12.5-50 mg/d Chlorthalidone ↓↓ 12.5-25 mg/d Metolazone ↓↓↓ 2.5-10 mg/d Reserve for resistant edema --- 1.25-2.5 mg/d 1st line choice elderly Indapamide Aldosterone Antag Reserve for resistant HTN or HF Spironolactone ↑ 12.5-50 mg/d avoid K > 5.0 or CrCl < 30 Eplerenone ↑ 25-100 mg/d avoid K > 5.0 or CrCl < 30 K sparing Caution, ACE/ARB, renal failure Amiloride ↑ 5- 20 mg/d Use in combo to counteract K loss Triamterene ↑ 37.5-50 mg/d Combo product with HCTZ available Loop Reserve for HF or resistant edema Furosemide ↓↓ 20-80 mg/d Bioavailability 60% or less Bumetanide ↓↓ 0.5-4 mg/d Bioavailability 80% Torsemide ↓↓ 5-10 mg/d Bioavailability 80% Goodman and Gilmans: The Pharmacologic Basis of Therapeutic 12th edition: http://www.accesspharmacy.com DIURETICS Compelling Indications: • Heart Failure • High CAD risk • Diabetes • Recurrent Stroke Prevention Monitoring • Electrolytes after initiation or dose increases • Every 6-12 months • K sparing, every 3 months if also on RAAS inhibitor Side Effects • • • • Increase glucose Increase uric acid — precipitate gout dehydration — orthostatic hypotension Spironolactone — gynecomastia MECHANISM OF ACTION ACE INHIBITORS ARBS Drug Dose Drug Captopril 12.5-50 mg tid Candesartan (Atacand)* 4-32 mg/d Enalapril 2.5-40 mg/day Eprosartan (Tevetan)* 400-800 mg/d Lisinopril 5-40 mg/day Irbesartan (Avapro)* 75-300 mg/d Benazepril 5-80 mg/day Losartan (Cozaar)* 25-100 mg/d Fosinopril* 10-80 mg/day Omelsartan (Benicar) 20-40 mg/d Moexipril 7.5-30 mg/day Telmisartan (Micardis) 40-80 mg/d Quinapril 5-80 mg/day Valsartan (Diovan) 80-320 mg/d Ramipril 1.25-20 mg/day * generic Perindopril 2-16 mg/day Trandolapril 1-8 mg/day Combining with thiazide usually more effective than dose increase * Dual elimination: liver & kidney Dose Direct Renin Inhibitors • Aliskiren (Tekturna) • 150-300 mg/day • As effective as ACE or ARB in HTN Goodman and Gilmans: The Pharmacologic Basis of Therapeutic 12th edition: http://www.accesspharmacy.com ACE INHIBITORS AND ARB Compelling Indications • Systolic Heart Failure • DM • CKD with Proteinuria • CAD Monitoring • 1-2 weeks after initiation or dose change for K & Cr • Every 6 months on stable doses Side Effects • Dry Cough Switch to ARB • Angioedema: ARB likely okay, consider severity • Hyperkalemia: supplements, diet, worsening renal fxn Combining RAAS inhibitors is generally not recommended • No added benefit CV or renal outcomes / Increased toxicity • ACE or ARB + aldosterone antagonist is the exception Avoid in Pregnancy BETA BLOCKERS MOA: Sympatholytic ↓ HR and CO / ↓ release of renin Receptor Affinity Lipid Solubility Renal Elimination Dose Atenolol β1 Low Yes 25-100 mg/d Bisoprolol β1 Low No 2.5-10 mg/d Carvedilol β1, β2, α Mod No 3.125-25 mg bid Labetalol β1, β2, α Low No 100-400 mg bid Metoprolol tartrate Metoprolol succinate β1 Mod No 50-200 mg bid 25-200 mg/d Nebivolol β1 Low No 5-40 mg/d β1, β2 High No 40-120 mg bid Propranolol Avoid sudden discontinuation Rebound HTN d/t up regulation of ᵦ receptors Goodman and Gilmans: The Pharmacologic Basis of Therapeutic 12th edition: http://www.accesspharmacy.com BETA BLOCKERS Compelling Indications • CAD • Systolic Heart Failure Monitoring • ECG if bradycardic- AV block • Avoid combining with other AV nodal blocking agents Side Effects • Bronchoconstriction—Reactive Airway Disease • Choose B1 selective agent and keep at lower doses • Metabolic—↓HDL, ↑ LDL and triglycerides • Diabetes—↓ insulin sensitivity • Mask symptoms of hypoglycemia, delay recovery • Carvedilol may have advantage as it ↑’s insulin sensitivity • Peripheral Vascular Disease—↑ symptoms, use B1 selective • Depression—Choose agent with low lipid solubility • Fatigue CALCIUM CHANNEL BLOCKERS http://www.accesspharmacy.com/content.aspx?aID=6543820 http://www.drugdevelopment-technology.com/projects/istaroxime/istaroxime4.html CCB CONSIDERATIONS AV Node SA Node Contractility Vasodilation Nifedipine^ 0 1 1 5 Amlodipine 0 1 1 5 Felodipine 0 1 1 5 Nicardipine 0 1 0 5 Diltiazem^ 4 2 2 3 Verapamil^ 5 4 4 3 DHP Non-DHP# ^ Do not use short acting agents in treatment of HTN # Do not combine with beta-blockers: increased risk of bradycardia Doses provided in Dr DiDomenico’s lecture on angina Goodman and Gilmans: The Pharmacologic Basis of Therapeutic 12th edition: http://www.accesspharmacy.com CALCIUM CHANNEL BLOCKERS Compelling Indications • High CAD risk • Diabetes Monitoring / Side Effects • Dihydropyridine (DHP) • peripheral edema • reflex tachycardia • dizziness • Non DHP • Bradycardia • Contra-indicated in heart failure • Constipation (especially verapamil) VASODILATORS: ALPHA-1 BLOCKERS Doxazosin: start 1 mg daily: max 8 mg daily Prazosin: start 1 mg bid-tid: max 15 mg/day Terazosin: start 1 mg qhs: max 20 mg/day http://cvpharmacology.com/vasodilator/alpha.htm VASODILATORS: ALPHA-1 BLOCKERS Compelling Indications: None Second line therapy • Also used to treat BPH (benign prostatic hypertrophy) Monitoring: • Na and H20 retention with high doses Side Effects: • • • • Dizziness — Orthostatic hypotension, first dose syncope Headaches Reflex tachycardia Fatigue VASODILATORS: DIRECT MOA: vascular smooth muscle relaxation Compelling Indications: None Second line therapy: Resistant HTN Hydralazine • 10 – 50 mg qid; max 300 mg /day • Often dosed bid or tid to improve adherence • Rare but serious SE: Lupus erythematosus, blood dyscrasias, peripheral neuritis • Headaches, tachycardia, angina, nausea, diarrhea, rash Minoxidil • • • • Start 5 mg daily; usual 10-40 mg daily; max 100 mg daily Rare but serious SE: Stevens-Johnson syndrome Hypertrichosis — used topically to promote hair growth Headache, edema, tachycardia, paresthesia VASODILATORS: DIRECT Caution: Increased myocardial work Use in combination with B-blocker / diuretic to combat these effects CENTRAL ALPHA 2 AGONISTS Bind to and activate α2 receptors in the brain ↓ sympathetic outflow to the heart → CO and HR ↓ sympathetic outflow to vasculature → ↓ vascular tone http://www.cvpharmacology.com/vasodilator/Central-acting.htm CENTRAL ALPHA 2 AGONISTS Compelling Indications: None Second line therapy: Resistant HTN Clonidine • Start 0.1 mg bid, titrate up weekly: max 2.4 mg/day • Available as a transdermal patch changed weekly • Severe rebound HTN if stopped abruptly • Side Effects: sedation, depression, bradycardia + many more Methyldopa • Start 250-500 mg bid-tid, adjust every 2-3 days, max 3gm/day • Can be used in pregnancy • Serious but uncommon SE: blood dyscrasias, myocarditis, pancreatitis • Side effects: sedation, orthostatic hypotension + many more ANTIHYPERTENSIVES: Centrally Acting: • Methlydopa • Clonidine Sedation, dry mouth B-blockers: • Atenolol • Carvedilol • Metoprolol • Propranolol Bradycardia Angiotensinogen Renin Aliskiren α 1 blocker: • Prazosin, Doxazosin, Terazosin Dizziness, edema Vascular Smooth Muscle: • Hydralazine, Minoxidil • CCBs Headache, Dizziness, edema, Diuretics: • Thiazide • Loop • Other hypokalemia ACE Angiotensin ACE I Inhibitors Hyperkalemia, dry cough Angiotensin II ARBs ALGORITHM FOR TREATMENT OF HYPERTENSION Lifestyle Modifications Not at Goal Blood Pressure (<140/90 mmHg) (<130/80 mmHg for those with diabetes or chronic kidney disease) Initial Drug Choices Without Compelling Indications With Compelling Indications Stage 1 Hypertension Stage 2 Hypertension (SBP 140–159 or DBP 90–99 mmHg) Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination. (SBP >160 or DBP >100 mmHg) 2-drug combination for most (usually thiazide-type diuretic and ACEI, or ARB, or BB, or CCB) Not at Goal Blood Pressure Optimize dosages or add additional drugs until goal blood pressure is achieved. Consider consultation with hypertension specialist. JNC VII JAMA 2003;289:2560-2572 Drug(s) for the compelling indications Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed. INADEQUATE BP RESPONSE WITH INITIAL AGENT Increase dose Substitute new drug from different class • Little to no response to initial drug • No compelling indication for the drug • Troublesome SE Add a new drug from a different class • Initial drug produces some response and is well tolerated • Compelling indication for the initial drug • Add thiazide if not used initially HTN: SPECIAL POPULATIONS Elderly • Isolated systolic HTN common • SBP rises and DPB declines with aging • • • • Generally salt sensitive Use lower initial drug doses and slower dose titration Avoid 1-blockers, labetalol, central 2 agonists JNC-8 – higher BP goal? AHA Consensus Statement on the Elderly 2011 • Goal SBP < 140 mm Hg • Age > 80, goal SBP < 150 mmHg • No evidence for lower BP goals for elderly patients at high risk, eg DM, CAD, CKD. • Maintain DBP > 65 mmHg --- coronary perfusion Circulation 2011;123:2434-2506 HTN ELDERLY GUIDELINES Canada 2013 • In the very elderly (age ≥ 80), the target for SBP should be < 150 (grade C) • No changes for those age 65-79; ie goal remains at < 140/90 Europe 2013 • In elderly < 80 years old with SBP ≥160 mmHg there is solid evidence to reducing SBP to 150 and 140 mmHg (IA) • In fit elderly patients < 80 years old SBP values <140 mmHg may be considered, whereas in the fragile elderly population SBP goals should be adapted to individual tolerability (IIb C) • If > 80 years and with initial SBP ≥160 mmHg, it is recommended to reduce SBP to between 150 and 140 mmHg provided they are in good physical and mental conditions (IB) Benefit in treating elderly, ↓ stroke, CV events, heart failure Canadian Journal of Cardiology 2013;29:528-542 HTN: SPECIAL POPULATIONS African Americans • Prevalence, severity and impact increased compared to other populations • Onset at younger age • More Na+ sensitive, lower plasma renin activity • Good response to Na restriction and diuretic therapy • response to ACE inhibitors, ARBs, and -blockers as monotherapy • HOWEVER, can be overcome by adding a diuretic • Still indicated if compelling indication exists! • ACE inhibitor angioedema 2-4 x more frequent HYPERTENSIVE CRISIS HYPERTENSION CRISES EMERGENCY URGENCY BP >180/120 BP >180/120 Acute Target Organ Damage No Target Organ Damage Life threatening Not life-threatening GOAL: BP now GOAL: BP over days IV therapy Oral therapy HYPERTENSIVE EMERGENCIES Heart • Acute coronary syndrome • Acute heart failure with pulmonary edema • Dissecting aortic aneurysm CNS • Intra-cerebral hemorrhage / CVA • Encephalopathy Eclampsia Acute Renal Failure Eyes: • Papilledema, hemorrhage TREATMENT FOR HYPERTENSIVE EMERGENCIES Goal: • Lower MAP no greater than 20-25% in a few hours • Maintain DBP 100-110 mmHg • Too rapid or too much cerebral hypoperfusion Continuous BP monitoring IV Vasodilators IV Adrenergic Inhibitors Sodium Nitroprusside Labetalol Nicardipine Esmolol Nitroglycerin Phentolamine Enalaprilat Fenoldopam Hydralazine IV VASODILATORS MOA Indication Nitroprusside Vasodilator* Most HTN emergencies • Caution high ICP or azotemia Nicardipine CCB Most HTN emergencies • Except acute heart failure • Caution coronary ischemia Nitroglycerin Vasodilator* Coronary Ischemia Enalaprilat ACE inhibitor Acute heart failure • Avoid in acute MI Fenoldopam Dopamine 1 agonist* Most HTN emergencies • Caution glaucoma Hydralazine Direct vasodilator Eclampsia * See next slide IV VASODILATORS: MOA Fenoldopam Release Pro drug D1 receptor agonist moderate affinity α2 vasodilation Nitroprusside: • • • arteriole and venous No tolerance Less effect on HR Nitroglycerin • • • 1° venodilator Arteriole dilator at high doses + tolerance http://cvpharmacology.com/vasodilator/nitrodilator%20mech.gif http://www.drugabuse.gov/sites/default/files/imagecache/content_image_landscape/images/colorbox/dopamine.gif IV VASODILATORS Dose Onset Adverse Effects Nitroprusside 0.25-10 ug/min immediate Thiocyanate Cyanide toxicity Nicardipine 5-15 mg/hr 5-10 min ↑ HR, HA, flushing Nitroglycerin 5-100 ug/min 2-5 min HA, vomiting Tolerance with prolonged use Enalaprilat 1.25-5 mg q6h 15-30 min High renin states: ↓↓↓ BP Variable response Fenoldopam 0.1-0.3 ug/kg/min < 5 min ↑ HR, HA, flushing, nausea Hydralazine 10-20 mg IV 10-50 mg IM 10-20 min 20-30 min ↑ HR, HA, flushing, vomiting, angina Duration of action varies from 1-2 min to 6 hours NITROPRUSSIDE TOXICITY Metabolism releases Cyanide Increased Risk if: • • • • Rate at ≥ 5 ug/kg/min 2 ug/kg/min for prolonged use (24-48 hours) Renal insufficiency Can administer Na Thiosulfate to enhance metabolism of cyanide Cyanide Toxicity • • • • • Weakness Headaches Vertigo Confusion / giddiness Perceived difficulty breathing Thiocyanate Toxicity • • • http://www.biomedcentral.com/content/figures/1471-2253-13-9-1-l.jpg Anorexia / nausea Fatigue Toxic psychosis IV ADRENERGIC BLOCKERS MOA Indication Labetalol B1, B2, α blocker Most HTN emergencies Except acute heart failure Esmolol B1 blocker Aortic dissection Perioperative Phentolamine α antagonist Catecholamine excess Dose Onset Adverse (min) Effects Labetalol 20-80 mg q 10 min 0.5-2.0 mg/min 5-10 Esmolol 250-500 ug/kg/min x 1 min 1-2 50-100 ug/kg/min x 4 min Hypotension, nausea Phentolamine 5-15 mg ↑ HR, HA, flushing 1-2 Duration of action varies from 3-10 min to 6 hours Heart block