* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download HTN Soap note with graphs
Survey
Document related concepts
Transcript
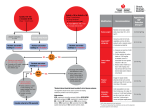
FINAL DRAFT-HTN 4/1/08 SUBJECTIVE Patient presents for evaluation of confirmed hypertension CLASSIFICATION OF BLOOD PRESSURE (BP)* CATEGORY SBP mmHg Normal < 120 DBP mmHg and < 80 Prehypertension 120 – 139 or 80 - 89 Hypertension, Stage1 140 – 159 or 90 – 99 Hypertension, Stage 2 > 160 or > 100 * See Blood Pressure Measurement Techniques (reverse side) Key: SBP = systolic blood pressure DBP = diastolic blood pressure *** For those with high pressures (systolic greater than 180 mm Hg or diastolic greater than 110 mm Hg) evaluate and treat immediately or within one week, depending on clinical situation and complications. Confirm Elevated Blood Pressure: Confirmation is based on the initial visit, plus two follow up visits with at least two blood pressure readings at each visit. At least once a BP must be checked in both arms. At least once the BP must be taken in the upper arm above the antecubital space. Medications and Compliance Reviewed Medications that contribute to elevated BP -NSAIDS -decongestants -diet aids -herbals Past history reviewed/Problem list Pertinent conditions (CAD, angina, previous MI, DM, CHF, PVD, prior hx HTN, previous HTN rx, lipid disorders (including metabolic syndrome), LVH, Retinopathy, Renal disease (GFR<60 and microalbuminuria) Lifestyle factors Smoking, high sodium intake, high fat diet, physical inactivity, excessive alcohol, overweight (BMI>30) Family history Cardiovascular Dyslipidemia Diabetes Family history of premature cardiovascular disease (men younger than 55 or women younger than 65). Page 1 of 9 ROS Constitutional (wt gain or loss), fatigue Visual (blurred vision, other) Neurological (headache, dizziness, weakness, loss of feeling, other) Respiratory (dyspnea at rest or activity, snoring, apneic spells) Cardiac (Chest pain with or without exertion, palpitations, irregular pulse, orthopnea, claudication, edema) Neuropsych (depression, insomnia, psychosocial stress, anxiety) PHYSICAL EXAM Vitals Waist circumference General (grooming, orientation, distress, obesity, other) Head Fundoscopic (hemorrhages, exudates, AV crossing changes, disc normal or edematous, arteriolar narrowing general or focal, cataracts, eye doctor visit) Neck (JVD, thyromegaly, carotid bruits, other) Lungs (auscultation, percussion, respiratory effort, rales, wheezing, rhonchi, other) Heart (rhythm, murmurs, PMI, gallop, click, other) Abdomen (soft, tenderness, organomegaly, abnormal pulsation, bruits, enlarged kidneys, mass, other) Neurological (localized weakness, facial droop, gait) Extremities ( edema, pulses, symmetry, radial-femoral delay) Psych (orientation, mood, affect) LAB FBS HCT Na K Creatinine (GFR) Ca Lipids 12 lead EKG Additional tests may be ordered at the discretion of the provider based on clinical findings. These may include, but are not limited to, CBC, CXR, uric acid, and urine microalbumin. Page 2 of 9 ASSESSMENT Primary hypertension without target organ disease or with target organ disease (LVH, CAD, CABG, CHF, PVD, angina, renal disease, retinopathy, stroke, TIA, dementia) ASSESS FOR IDENTIFIABLE CAUSES OF HYPERTENSION Sleep apnea Cushing’s syndrome or steroid therapy Drug induced/related Pheochromocytoma Chronic kidney disease Coarctation of aorta Primary aldosteronism Thyroid/parathyroid disease Renovascular disease Risk Factors for Major Cardiovascular Disease: Hypertension Age (older than 55 for men, 65 for women) Diabetes mellitus Elevated LDL cholesterol Low HDL cholesterol (men <40 mg/dL, women <50mg/dL) Estimated GFR less than 60 mL/min Microalbuminuria Family history of premature cardiovascular disease (men younger than 55 or women younger than 65) Obesity (body mass index greater than or equal to 30 kg/m2, waist circumference greater than 40 inches for men and greater than 35 inches for women) Physical inactivity Tobacco usage, particularly cigarettes Consider a Diagnosis of Secondary HTN: Patients with an abrupt onset of symptomatic HTN Stage 2 hypertension Hypertensive crisis Sudden loss of BP control after many years of stability on drug therapy Drug resistant HTN Individuals with no family history of HTN Acute increase in plasma creatinine that is unexplained or after an initial treatment with an ACE or an ARB Lateralizing abdominal bruit Recurrent flash pulmonary edema Page 3 of 9 Secondary Etiology Clinical Scenario Tests Renal artery stenosis FMD – young females Older patients with vascular disease Duplex Doppler US or MRA or CT angiogram Primary renal disease Abnormal GFR GFR UA Pheochromocytoma Headache (90%), palpitations, sweating/pallor, paroxysm of HTN or persistent HTN (50/50) Hypokalemia, adrenal incidentaloma 24 urine fractionated metanepharines or Plasma fractionated metanepharines Primary aldosteronism Cushing’s Disease “moon”facies, central obesity, stria, ecchymosis Obstructive Sleep Apnea Snoring +/- apneic spells, daytime somnelence Absent or lagging LE pulses Both hypo and hyper Hypercalcemia – stones, groans, and psychic overtones Coarctation of the Aorta Thyroid disorder Hyperparathyroidism Plasma aldosterone concentration (PAC) to plasma renin activity (PRA) = PAC/PRA 1mg Overnight Dexamethasone Suppression Test 24 hour urine cortisol Overnight Sleep Study Comments All are options and debated. MRA most often used at Theda for screening. If pt has RI Nephrogenic Systemic Fibrosis, although rare, now a real issue as it is life threatening. Contrast induced nephropathy also issue with CT angio. Renal US can show asymmetry and Polycystic Kidney Disease. Options are debated. Different sources will sight different cutoffs to change sensitivity and specificity. In general, <20 normal Options are debated. CT angiogram TSH TSH sufficient for screening test. PTH Page 4 of 9 Calculated 10 year CHD risk Goal BP < 140/90 Goal BP for those pts with diabetes, CKD, and heart failure: <130/80 Goal blood pressures measured out of the office setting should be: <135/85 (no comorbidities) <125/75 ( those with comorbidities) Review this with the patient. Goal blood pressures for those patients with chronic kidney disease: <130/80 <120/75 if urinary protein excretion > 1-2g/day Consider 24 hour ambulatory blood pressure monitoring (ABPM) in the assessment of white coat or office effect patients who lack evidence of target organ damage, and who have normal out-ofoffice BP readings. Other clinical situations in which ABPM may be helpful include the assessment of drug resistance, hypotensive symptoms, episodic hypertension and suspected autonomic dysfunction. Page 5 of 9 PLAN Lifestyle modifications should be: The cornerstone of the initial therapy for hypertension Reviewed and re-emphasized at least annually Lifestyle Modifications to Prevent and Manage Hypertension Modification Recommendation Approximate SBP reduction (range) Weight reduction Adopt DASH** eating plan Dietary sodium reduction Physical activity Moderation of alcohol consumption Maintain normal body weight (body mass index 18.5-24.9 kg/m2). Consume a diet rich in fruits, vegetables and low-fat dairy products, with a reduced content of saturated and total fat. Reduce dietary sodium intake to no more than 100 mmol per day (2.4 g sodium or 6 g sodium chloride). Engage in regular aerobic physical activity such as brisk walking (at least 30-45 minutes per day, most days of the week). Limit consumption to no more than two drinks (e.g., 24 oz. beer, 10 oz. wine, or 3 oz. 80 proof whiskey) per day in most men and to no more than one drink per day in women and lighter-weight persons. 5-20 mm Hg/10 kg 8-14 mm Hg 2-8 mm Hg 4-9 mm Hg 2-4 mm Hg **DASH indicates Dietary Approaches to Stop Hypertension. Page 6 of 9 Medications COMPELLING INDICATIONS FOR INDIVIDUAL DRUG CLASSES COMPELLING INDICATION Heart failure INITIAL THERAPY OPTIONS THIAZ, BB, ACEI, ARB, ALDO ANT Post myocardial infarction BB, ACEI, ALDO ANT High CVD risk THIAZ, BB, ACEI, CCB Diabetes THIAZ, BB, ACEI, ARB, CCB Chronic kidney disease ACEI, ARB Recurrent stroke prevention THIAZ, ACEI Key: THIAZ = thiazide diuretic, ACEI = angiotensin converting enzyme inhibitor, ARB = angiotensin receptor blocker, BB = beta blocker, CCB = calcium channel blocker, ALDO ANT = aldosterone antagonist Primary HTN Medications: A Thiazide type diuretic should be considered as initial therapy with uncomplicated HTN. In patients for whom diuretics are contraindicated or poorly tolerated, use of a betablocker, ACE inhibitor, ARB or calcium antagonist is appropriate. Outcome data does not support B blockers for first line therapy for patients >60 years of age. In order to decrease cost, consider three strategies: split tablet dosing, 3 month supply by mail order and generic medications. HTN with Diabetes: Regimen should include either an ACE inhibitor or an ARB. If one class is not tolerated the other should be substituted. If needed to achieve BP targets: GFR 50ml/min- a thiazide diuretic should be added GFR < 50ml/min- a loop diuretic should be added Multiple drug therapy (two or more agents at maximal doses) is generally required to achieve blood pressure targets. FOLLOW UP Once a hypertensive drug therapy is initiated, most patients should return for follow up and medication adjustments at least monthly until BP goal is reached. Option if not at goal: -Increase dose of initial drug. -Substitute agent from another class -Add a second drug from another class BP at goal: -Follow up office visit in 3-6 months -Follow up visits to assess for target organ disease, new risk factors, comorbidities and need for lab tests. -Serum potassium and creatinine should be monitored at least annually. Additional labs as indicated with change in condition or medication regimen. Page 7 of 9 PATIENT EDUCATION Website Title/Description Organization http://www.americanheart.org Web site with excellent resources for patient education and general heart health resources. Understanding and Controlling Your High Blood Pressure and Exercise and Your Heart. Web site with excellent resources for patient education. Includes an online catalogue of materials. -Facts about Heart Disease and Women: Preventing and Controlling High Blood Pressure (brochure #97-3655) -Facts about Lowering Blood Pressure (brochure #5232) -Facts about the DASH Diet (booklet #03-4082) -Your Guide to Lowering Blood Pressure (booklet #03-5232) Web site with excellent resources for patient education resources, particularly using search terms “hypertension,” “blood pressure” and “home monitoring.” American Heart Association (AHA) http://www.nhlbi.nih.gov http://www.mayoclinic.com http://www.webmd.com National Heart, Lung & Blood Institute (NHLBI) Mayo Health Oasis Comprehensive health resources for consumers, physicians, nurses, and educators. Includes news, chat forums, health quizzes and consumer product updates. Page 8 of 9 REFERENCES Institute for Clinical Systems Improvement Health Care Guideline, Hypertension Diagnosis and Treatment, Eleventh Edition /October 2006. www.icsi.org JNC 7, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, U.S. Department Of Health And Human Services, May 2003. www.nhlbi.nih.gov Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, Adult Treatment Panel III, September 2002. www.nhlbi.nih.gov Institute for Clinical Systems Improvement Health Care Management of Type 2 Diabetes Mellitus, Eleventh Edition/ November 2006. www.icsi.org Page 9 of 9









![[ Insert Title Here ]](http://s1.studyres.com/store/data/008479268_1-03ff748536c27aeae665c17a72e89ec4-150x150.png)