* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Read More - Division of Rheumatology
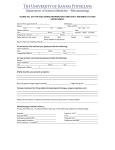
Survey
Document related concepts
Major histocompatibility complex wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Adaptive immune system wikipedia , lookup
Rheumatic fever wikipedia , lookup
Innate immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Molecular mimicry wikipedia , lookup
Autoimmunity wikipedia , lookup
Transcript
The rheumatologists at Columbia University Medical Center/ New York-Presbyterian Hospital, are acknowledged as leaders in the spheres of patient care, medical education, and basic and clinical research focused on finding the causes and cures of arthritis. Given the extraordinary medical advances that have occurred throughout the history of the Division of Rheumatology at Columbia, our physicians are now poised to prevent many joint disorders and universally improve the lives of patients who have arthritis. Dr. Joan Bathon is the current director of the Division of Rheumatology at New YorkPresbyterian Hospital/Columbia University Medical Center. Prior to coming to Columbia, Dr. Bathon served as deputy director of the Division of Rheumatology and director of the Arthritis Center at Johns Hopkins. Dr. Bathon is the Editor-in-Chief of the American College of Rheumatology journal, Arthritis and Rheumatism. Dr. Bathon is a renowned clinical researcher whose research focuses on rheumatoid arthritis and osteoarthritis; she is also a recognized authority on the arthritis-related cardiovascular risk. Dr. Bathon is presently the principal investigator of several federal and foundation grants to study risk factors and predictors of the enhanced risk of RA patients for accelerated cardiovascular disease. She is the co-principal investigator of a National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) sponsored Rheumatic Disease Research Center Core (RDRCC), and is a co-investigator of one of the Field Centers for the “Osteoarthritis Initiative (OAI)”, a NIAMS-sponsored large-scale longitudinal observational study of risk factors for knee osteoarthritis. Dr. Bathon is a former Associate Editor of Arthritis Research and Therapy and past Advisory Editor of Arthritis and Rheumatism. She previously served as a member of the FDA Arthritis Advisory Committee as well as a member of the Board of Directors of the American College of Rheumatology, and of the Board of Directors of the Arthritis Foundation, Maryland Chapter. Dr. Bathon is former Director of the Dean’s Office of Women in Science and Medicine, former CoChair of the Women’s Leadership Council, and former Chair of the Department of Medicine’s Task Force on Academic Careers of Women in Medicine, all at Hopkins. The Division of Rheumatology at Columbia has a long and distinguished history in the study and treatment of rheumatic diseases and in the mentoring and training of leaders in the field of rheumatology. For nearly a century it has been of our mission to be first and foremost in clinical care, the training of clinician scientists, and research. In the 1920’s, the Edward Daniels Faulkner Clinic for Arthritis was established at the ColumbiaPresbyterian Hospital. This clinic was the first clinical and research unit dedicated to rheumatic diseases in the country. The Faulkner clinic also established the first rheumatology fellowship program in New York. Dr. Ralph H. Boots, a practicing rheumatologist who had done significant research on rheumatic fever at the Rockefeller Institute for Medical Research, was the Faulkner clinic’s first director. Together with Dr. Martin Dawson, a colleague from the Rockefeller Institute, he affected the clinical and research arms of the clinic and ultimately brought about the rheumatology fellowship program. Borne from the Columbia fellowship program was the groundbreaking discovery of rheumatoid factors and their link to rheumatoid arthritis. Dr. Charles Ragan, a rheumatology fellow, together with Dr. Harry Rose, Chairman of the Division of Microbiology is credited with charting new ground with this breakthrough. Dr. Ragan was an astute and gifted scientist as well as a brilliant physician. In 1962 he was appointed the first Rheumatology Division Chief at Columbia by Dr. Robert Loeb. Dr. Ragan recruited and was succeeded by Dr. Charles Christian who made important contributions to the immune complex disease in experimental rabbit models and equally important contributions to human Systemic Lupus Erythematosus. Dr. Christian was followed by Dr. E. Carwile LeRoy- a pioneer in scleroderma research. In 1977 Dr. Leonard Chess was recruited to lead the Division; he served as director of the Division of Rheumatology at Columbia for 25 years. He is presently the director of Columbia University’s NIH designated Autoimmunity Center of Excellence (ACE). The National Institute of Health Autoimmunity Centers of Excellence were first established in 1999; Columbia was selected as one of four original centers. This important aspect of the Division’s lineage supports mechanistic studies of immune therapies for rheumatic diseases and clinical trials. An esteemed research scientist, Dr. Chess, has pioneered the identification and study of biologically and clinically important molecules on the surface of human T lymphocytes. An important characteristic of the Chess lab has been its ability to bring basic discoveries made at the bench to the development of drugs employed in the treatment of human immune disease. In this regard, Dr. Chess’ lab identified the structure and functions of key human T cell surface molecules (including CD4, CD8, γδTCR, CD40L, α1/β1 integrin). Some of these molecules have been employed to develop therapeutics in clinical trials of human immunologic disease: including recombinant CD4 molecules for HIV and monoclonal anti–CD40L and anti-VLA-1 for autoimmune disease and transplant rejection. In the early 1980’s, in collaboration with Dr. Richard Axel, Dr. Chess defined the functions of CD4 and CD8 molecules. The work on CD4 genes enabled experiments that definitively showed that CD4, in addition to functioning as a receptor for MHC class II, is also a HIV receptor and to clinical trials employing recombinant soluble CD4 which blocks HIV entry into cells. In 1986 Dr. Chess defined and isolated the first human T cells expressing the γδ T cell receptor and demonstrated that these T cells could function to secrete lymphokines and kill tumor cells. In the early 1990's, Dr. Chess' laboratory isolated and structurally defined a novel structure on activated CD4 T cells termed CD40 ligand (CD40L). This molecule has been shown to mediate the helper activity of T cells because patients with mutations in the CD40L gene have markedly reduced and defective antibody responses and succumb to pyogenic infections. Antibodies to CD40L were produced in Dr. Chess' lab were shown to inhibit antibody and cell mediated immune responses and were effective in the treatment of autoimmune responses and graft rejection in animal models and in human trials. In more recent studies, Dr. Chess together with Dr. Hong Jiang are defining immunoregulatory functions of MHC class I restricted CD8 T cells, which control autoimmune phenomenon in mice and man. Moreover these regulatory cells control immune responses by perceiving the avidity of antigen activated T cells. This has led to formulation of an avidity model of T cell regulation which has been shown to be intimately associated with the mechanisms of self-nonself discrimination as central function of the immune system. In 2005 Dr. Betty Diamond was recruited to be Director of Rheumatology; after a brief tenure at Columbia she accepted a position at the Feinstein Medical Research Facility. Dr. Robert Winchester, a member of the Columbia University Medical Center faculty since 1991, was appointed Director of the Division in 2007. Dr. Winchester was a pioneer in applying immunofluorescent techniques to characterizing lymphocyte subpopulations and the reactivity of autoantibodies with lymphocyte antigens. His introduction of (Fab’)2 fragments as fluorescent reagents allowed exclusion of IgG as a molecule intrinsically expressed on B cells as was the prevailing view at the time. These reagents facilitated the characterization of the presence and complex specificity of anti-lymphocyte antibodies in lupus. This work on fluorescent microscopy also led to his independent identification of MHC class II molecules, with the recognition of what is now termed HLA-DR. He was the first to show HLA-DR is expressed on B cells and monocytes and early myeloid forms, but not resting T cells. His studies on the expression of HLA-Dr during early hematopoetic differentiation are classic examples of the acquisition and loss of differentiation antigens with developmental stage. Several aspects of the expression of HLA-DR were found relevant to rheumatic diseases, including the first demonstration that fibroblastoid lineage lining cells in the rheumatoid synovium expressed HLA-DR molecules. Activated T cells in the circulation of those with SLE, or in the joint fluid of those with rheumatoid arthritis were shown to express HLA-DR. This was the first demonstration that upon activation a T cell expresses novel activation molecules. This was also one of the earliest observations that the T cells were activated in these autoimmune diseases and pointed the way towards the importance the T cell in autoimmune disease. His use of monoclonal antibodies led to the recognition of the monocyte antigen that is now termed CD14, and these reagents were used to show that the synovial lining was composed of cells derived from two distinct cell sublineages: the fibroblastoid and the myeloid. Dr. Winchester identified various allelic forms of HLA-DR, and was the first to show that the genetic susceptibility to systemic lupus differed from that associated with rheumatoid arthritis. He showed susceptibility to rheumatoid arthritis was associated with HLA-DR4 and with HLADR2 and HLA-DR3 in the case of lupus. Then using early molecular biologic techniques he contributed greatly to characterizing the structure of the MHC genes and their allelic variants. For this work on the identification of MHC class II genes and molecules he was elected a Fellow of the American Association for the Advancement of Science. The genetic characterization of population differences in the association of various HLA-DR alleles with rheumatoid arthritis resulted in the formulation of the shared epitope hypothesis. This theory unified the seemingly capricious associations of rheumatoid arthritis susceptibility with seemingly completely different HLA-DR alleles, by showing that they each encoded a similar peptide binding pocket. The shared epitope has become an important tool in numerous clinical and basic studies on rheumatoid arthritis. For this work Dr. Winchester was awarded the Howley prize of the Arthritis Foundation. With the appearance of the HIV epidemic Dr. Winchester described two new rheumatic diseases. One was the syndrome of diffuse infiltrative lymphocytosis, or DILS due to exuberant CD8 T cell response to HIV that simulated Sjogren’s syndrome. He also recognized that an inflammatory arthritis with features of Reiter’s syndrome and psoriatic arthritis developed in those who had the profound CD4 T cell depletion of AIDS, and used this “experiment of nature” to suggest that the pathogenesis of these spondyloarthritis diseases did not require direct participation of CD4 T cells and was likely mediated by CD8 T cells. Dr. Winchester continued his focus on translational studies that seek to understand the genetic basis of susceptibility to autoimmune disease and the mechanisms responsible for triggering and mediating autoimmune injury. One major area of research is concerned with the genetics of psoriatic arthritis and psoriasis that is revealing unexpected heterogeneity in the syndrome. Other work involved studies of the T-cell repertoire and provided insight into the mechanism of drugs used in the therapy of psoriatic arthritis, showing that methotrexate had essentially an immunomodulatory rather than a tolerizing effect on the T cells of the joint. This also led to a new hypothesis on the basic biology of psoriatic arthritis involved triggering by innate immune receptors that recognized tissue injury and stress. Dr. Winchester’s research has been performed in concert with a number of different gifted fellows and trainees who went on to have successful independent careers in research. In recognition of his commitment to fostering the next generation of clinical researchers, Dr. Winchester was awarded the American College of Rheumatology Excellence in Investigative Mentoring Award in fall 2008. Dr. Winchester currently serves as Professor of Medicine, Division of Rheumatology at Columbia.