* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Therapy of systemic hypertension
Survey
Document related concepts
Discovery and development of proton pump inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Norepinephrine wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Neuropharmacology wikipedia , lookup
Transcript
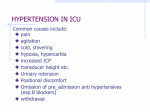
Therapy of systemic hypertension By Dr.Mohamed Abd Almoneim Drug therapy (antihypertensive drugs): • ►First choice groups (commonly used drugs): ABCD Angiotensin-converting enzyme inhibitors (ACEIs). Beta-blockers. Calcium channel blockers. Diuretics. ►Second choice groups: α1-adrenergic blockers: e.g. prazosin and doxasosin. Combined α and β-blockers: e.g. labetalol. Adrenergic neuron blockers: e.g. α-methyldopa and reserpine. Direct vasodilators: e.g. hydralazine and diazoxide. Central α2 stimulants: e.g. clonidine and guanfacine. Serotonin receptor blockers: e.g. ketanserine. Dopamine (D1) receptor agonists: e.g. fenoldopam. Beta blockers (LoL) * Pharmacokinetics Most of beta-blockers are absorbed orally: 1-Lipophilic (fat-soluble) beta-blockers: They are well absorbed, but undergo extensive hepatic metabolism (first pass effect). They are preferred in patients with renal failure. They can also cross the BBB and produce CNS effects. e.g. propranolol, ……. 2-Hydrophilic (water-soluble) beta-blockers: They are less well absorbed and slowly eliminated by the kidney. They are not preferred in patients with renal failure and cannot cross to CNS. e.g. atenolol, ………………etc. Mechanism of Action 1-Beta blocking action: 2-Intrinsic sympathomimetic action (ISA):= stimulate action. 3-Local anaesthetic, or quinidine-like action or membrane stabilizing activity. 3-CNS depressant action. 4-Direct vasodilator action.(recent drugs only) Not all beta-blockers have the above-mentioned actions but they differ in their mechanism of action. Classification 1- NON SELECTIVE BETA-BLOCKERS (1st GENERATION)=block 1, 2, 3 Liable to cause side effects.(propranolol) 2- BETA-1 SELECTIVE BLOCKERS "CARDIOSELECTIVE" (2nd GENERATION)= block 1 only (atenolol, bisoprolol) 3- BETA-BLOCKERS WITH V.D. ACTION (3rd GENERATION)e.g carvidelol Pharmacological Effects Cardiovascular system *Decreases heart rate and myocardial contractility.(B1) *Slow A-V conduction because the vagal action on the A.V. node predominates(B1). * Decreases total coronary blood flow(B2) and oxygen consumption(B1). *Quindine like action suppresses ectopic foci in the heart. *Decrease blood flow to most tissues by the unopposed alpha effect in response to reduced COP. *Decrease platelet aggregation. Lowers blood pressure by:******** 1-Negative inotropic and chronotropic effects lead to decreased COP 2-Decrease renin release 3-Blocks presynaptic 2 receptors lead to decreased NE release. 4-Decrease central sympathetic outflow. 5-Resetting of baroreceptors downwards. 6-May act through vascular prostaglandins. 7-Some blockers have vasodilator properties. Respiratory system Bronchospasm and increased airway resistance in susceptible patients Eye Decreases aqueous humor formation and reduce intra-ocular pressure. Metabolic effects: In normal individual : no effect on blood glucose. But in patient with diabetes: Augment hypoglycemic effects of insulin by blocking glycogenolsis and gluconeogenesis. Mask the hypoglycemic symptoms except sweating. Increase triglycerides and decrease H.D.L. CNS Antianxiety effect Insomnia, lethargy, night mares, vivid dreams and depression Others Salt and water retention secondary to the decrease in COP. Therapeutic Uses A- Cardiovascular 1-Treatment of hypertension with a diuretic. 2-Ischaemic heart diseases :(angina and infarction) 3-Cardiac arrhythmias: *Supraventricular arrhythmias especially those produced by exercise, thyrotoxicosis and pheochromocytoma. *Digitalis induced arrhythmias. *Arrhythmias induced during surgery (I.V. esmolol). 4-Hypertrophic obstructive cardiomyopathy: by their negative inotropic action. GIT Cases of gastrointestinal bleeding by decreasing COP and enhancing splanchenic vasoconstriction. Endocrine Hyperthyroidism. Pheochromocytoma. (Must be combined with alpha-blockers). C- Eye Open angle glaucoma. (Timolol) D- CNS Prophylaxis of migraine Anxiety and essential tremors. Carvedilol is nonselective beta blocker with antioxidant and alpha mediated vasodilator properties used in CHF, postinfarct LV Dysfunction and hypertension not for angin (combined beta and alpha blocker) Combined alpha and beta-blockers: labetalol It is selective 1 blocker and non-selective betablocker. It has rapid onset of action. It is used to control severe hypertension associated with pheochromocytoma and hypertension in pregnant patient. Adverse Effects 1-Heart failure, bradycardia, hypotension. 2-Bronchospasm in susceptible patients. 3-Potentiation of the hypoglycaemic effect of insulin and oral hypoglycemic drugs and masking of the hypoglycaemic symptoms. 4-Peripheral ischaemia, intermittent claudication and cold extremities. 5-Reduced blood flow to the liver and kidney reducing metabolism of drugs. 6-Hyperkalaemia.. 7-Nightmares, vivid dreams and depression. 8-Nausea, vomiting, diarrhea or constipation. 9-Increased plasma triglycerides and decrease HDL. 10-Allergic reactions (rash fever) 11-Sudden withdrawal leads to aggravation of the disease under treatment due to up regulation of beta-receptors. 12-Decrease sexual function. Contraindications 1-Congestive heart failure. 2-Heart block. 3-Variant angina. 4-Hypotension. 5-Peripheral vascular diseases. 6-Bronchial asthma. 7-With verapamil (Negative chronotropic and inotropic). 8-Alone in pheochromocytoma (Severe hypertension). 9-Never stopped suddenly (Especially in case of angina) 10-Diabetes mellitus. ►Indications of beta-blockers in hypertension: 1-Hypertension associated with: IHD, cardiac arrhythmia, or thyrotoxicosis. 2-Hypertension associated with high plasma renin (hyperreninemic hypertension). 3-In patients with increased sympathetic overactivity e.g. young age, hyperkinetic circulation, etc. 4-As a part of combined therapy. What are the criteria of ideal beta-blocker in hypertension? It should be: (1) β1-cardioselective, (2) Has long duration of action; and (3) Has improved pharmacokinetic profile e.g. atenolol, bisoprolol…... Alpha blockers :PRAZOSIN Mechanism of Action (Selective 1 blocker and Direct V.D. at high doses). Pharmacological Effects V.D. of arteries and veins lowering the blood pressure. It does not produce any change in C.O.P., renal blood flow and GFR thus; it could be used in renal failure. Salt and water retention. Therapeutic Uses Treatment of mild to moderate hypertension. Treatment of acute congestive heart failure (decreases pre- and after-load). Impaired bladder emptying due to prostate obstruction (decreased the tone of trigone) leads to decreased resistance to flow of urine. Adverse Effects First dose effect: 1-The initial dose especially if large can produce postural hypotension and syncope. It occurs most commonly in salt and water depleted patients (start with a small dose and at bedtime). 2-Dizziness, headache, drowsiness, and palpitation (disappears with continued treatment). 3-False positive tests for antinuclear factor. 4-Salt and water retention. TERAZOSIN and TRIMAZOCIN Similar to prazosin but it does not produce first-dose syncope. Centrally acting antihypertensive drugs 1-Adrenergic neuron blockers: reserpine . Reserpine : *Adrenergic neurone blocking action by preventing the granular uptake of catecholamines where it stays outside the granules (in the cytoplasm) to be inactivated by MAO enzyme. Now, the nerve has to synthesize more and more NE to keep the stores constant. As this process is limited, with frequent sympathetic stimulation the granules are depleted and the released NE becomes less, leading to decreased sympathetic tone. This process of depletion needs about seven days to be completed. Depletion of tissues e.g. brain, heart, and adrenal medulla from their catecholamine and 5HT content. *Parasympathomimetic action. The hypotension effect is due to: *Adrenergic neurone blocking action. *Central action (inhibition of VMC and tranquilization) *Depletion of suprarenal medulla. Adverse Effects: 1-Bradycardia, flushing and nasal stuffiness. 2-Hyperacidity, peptic ulceration, salivation and diarrhea. 3-Loss of libido and impotence in males. 4-Salt and water retention. 5-Psychic depression, suicidal attempts, parkinsonian-like rigidity and nightmares, cancer breast. Uses : Less common nowadays due its side effects. Not alone but as part of combination therapy for treatment of hypertension. 2-Alpha methyl dopa: Pharmacological actions 1-In the CNS it is transformed to alpha methyl NE. which activates inhibitory 2 receptor in the medullary region leading to inhibition of the sympathetic outflow. 2-Inhibits plasma renin activity. 3-Adrenergic neurone blocking action by: *Inhibition of dopa decarboxylase enzyme. *Competes with dopa for dopa decarboxylase enzyme leading to formation of alpha methyl norepinephrine (false chemical transmitter) ineffective on the adrenergic receptors. Pharmacological effects Antihypertensive. Therapeutic Uses Treatment of hypertension. (in pregnant female and in chronic renal failure) because it does not affect the heart rate, COP, renal, cerebral or myocardial blood flow. Adverse effects Drowsiness (common and disappears with continued treatment). Depression (Less than reserpine). Nasal stuffiness. Drug fever. Salt and water retention. Liver damage. Bone marrow depression. Positive Commb's test. 3-Beta-Blockers: propranolol . 4-Central α2 stimulants: Clonidine and guanfacine. Mechanism: It stimulates presynaptic α2 receptors → inhibition of NA release. It inhibits dopamine hydroxylase enzyme → inhibition of NA synthesis. Inhibition of central sympathetic outflow. It inhibits renin release and plasma renin activity. Therapeutic uses: 1-Moderate to severe hypertension. 2-Prophylaxis of migraine. 3-In opiate withdrawal to decrease symptoms of sympathetic overactivity. 4-As a sedative to reduce anxiety in preanesthetic medication. Side effects: Sedation and dry mouth (xerostomia). Severe hypertension can occur with overdoses due to stimulation of α1 receptors as a result of loss of selectivity. Sudden withdrawal can lead to hypertensive crisis (treated by combined α & β blockers), so it must be stopped gradually. Salt and water retention. Guanfacin: it has a mechanism of action and side effects similar to clonidine. Serotonin receptor blockers: Ketanserine Mechanism: It blocks vascular α1 receptors and platelet 5-HT2 receptors → VD and ↓ platelet aggregation. Uses: Treatment of hypertension. Treatment of peripheral vascular disease. Thrombophlebitis and pulmonary embolism. Side effects: dizziness and fatigue. Dopamine (D1) receptors agonists: Fenoldopam Mechanism: It stimulates D1 receptors in peripheral arteries leading to VD and diuresis. Uses: it is given by continuous i.v. infusion 1-Treatment of hypertensive emergencies. 2-Treatment of post-operative hypertension. Side effects: Hypotension and reflex tachycardia Increase IOP so it should be avoided in patients with glaucoma. LOOP DIURETICS (High-Ceiling Diuretics) Loop diuretics include: furosemide, bumetanide, ,,,,, Pharmacokinetics They are rapidly absorbed from GIT and can be given i.v. General characteristics 1-Efficacy: are the most potent diuretics. They are effective at low GFR even below 10 ml/minute. 2-Onset: They have rapid onset of action, ½ - 1 hour after oral administration and 5-10 min. following i.v. injection. 3-Duration: They have short duration of action up to 4 hours. Mechanism of action A.Renal mechanism: 1-Diuretic : see renal pharmacology……………….. 2-The loop diuretic furosemide produces stimulation of cyclooxygenase activity resulting in increased synthesis of vasodilator prosta-glandins PGE2 and PGI2. These prostaglandins may contribute to furosemide increased glomerular filtration and promoting water and sodium excretion. B. Extra-renal mechanism: Furosemide has actions on the vascular system (venodilator action) that occur before its diuretic and is mediated by PGs. These effects produces changes in renal blood flow and a reduction in LV filling pressure. Uses 1-Acute pulmonary edema. 2-All types of Na+ salt and water retention including edema, ascites and pleural effusion especially severe cases. 3-Hypertensive emergencies (by i.v. route) and in some cases of renal hypertension. 4-Oliguria due to acute renal failure. 5-Hyperkalemia; they can significantly enhance urinary K+excretion. 6-Drug poisoning to produce forced diuresis and enhance renal excretion of the offending drug. Side Effects Hypokalaemia metabolic alkalosis: Hypomagnesaemia: Hyovolaemia and hyponatraemia: Hyperuricaemic: Ototoxicity (more with ethacrynic acid): It is common with impaired renal functions and in patients receiving other ototoxic drugs such as aminoglycoside antibiotics. Glucose intolerance (hyperglycemia): this is due to inhibition of insulin release from B cells of pancreas (by opening K+ channels) and/or diminishes peripheral glucose utilization. This is less common than with thiazides. Hypersensitivity and idiosyncrasy: allergic reactions in the form of skin rash, oesinophilia or allergic interstitial nephritis occur with furosemide and are usually reversible. Hyperlipidemia: increase LDL & TG and decrease HDL. Interactions 1-The diuretic induced K+ deficiency increases the sensitivity of myocardium to digitalis. 2-Glucocorticoid treatment produces additive decrease in serum potassium level. 4-Ethacrynic potentiates ototoxicity of aminoglycosides. 5-Furosemide potentates nephrotoxicity of cephalosporins. 6-Non-steroidal anti-inflammatory drugs which are potent inhibitors of prostaglandin synthesis, reduce the diuretic effects of furosemide because these effects may be mediated through furosemide induced increase in synthesis of PGE2 and PGI2. 7-Organic acid such as probenicid and indomethacin which are secreted by the active organic acid secretory system in the PCT could inhibit tubular secretion of loop diuretic competitively and thus prevent them to reach their site of action and reduce their diuretic activity. THIAZIDES e.g. chlorothiazide and hydrochlorothiazide Widely used diuretics because they are effective orally and have moderate diuretic efficacy (prevents reabsorption of about 10% of Na+ in the filtrate). Pharmacokinetics Thiazides are well absorbed one hour after oral administration. They are widely distributed in the body and can cross the placenta Thiazides are excreted by the renal organic acid secretory system at the PCT. General Characteristics Site: They act principally at proximal part of DCT. Efficacy: They have moderate diuretic efficacy (prevents reabsorption of about 10% of Na+ in the filtrate. They should be avoided in renal impairment. Onset: They act within one hour after oral administration. Mechanism of Action: • See renal pharmacology(urine block) Pharmacological Effects 1-They increase renal excretion of Na+ and Cl- accompanied with water. 2-They increase K+ excretion. 3-They may decrease uric acid excretion leading to hyperuricaemia. 4-They decrease renal blood flow through a direct action on renal vasculature. 7-Antihypertensive effect (zhe mechanism of antihypertensive action is): *Decrease peripheral vascular resistance due to vasodilator action possibly through: A- Direct V.D B- Decreased vascular receptor sensitivity to vasopressor agents (adrenaline, angiotensin...) by decreasing Na+ content in the cells of vascular wall. C- Increase synthesis of the vasodilator PGs. *Decreased cardiac output due to decrease blood volume by the diuretic action Uses Essential hypertension: they may be used alone as initial monotherapy or as a part of combined antihypertensive regimen. They are used in treatment of edema and ascites (i.e. all types of Na+ and H2O retention) due to mild or moderate congestive heart failure, hepatic disease and renal disease. Side Effects Hypokalaemia metabolic alkalosis. Hypovolaemia and hyponatraemia. Hypotension Hyperuricaemia. Hyperglycaemia: produced by the same mechanisms mentioned with loop diuretics. Hyperlipidaemia: thiazides increase serum cholesterol, triglycerides and LDL. This is possibly due to decreased insulin activity or release. Hypersensitivity: hypersensitivity reactions are related to sulfonamide moiety and there is cross sensitivity with other sulfonamides. Deterioration of patients with hepatic or renal failure. Other side effects: parethesia, drowsiness, fatigability and impotence are dose-related side effects. POTASSIUM - SPARING DIURETICS Aldosterone antagonists: Spironolactore and eplerenone. Direct Na+- channel inhibitors: Triamterene and amiloride. General Characteristics Site: Distal part of DCT or cortical part of collecting ducts. Efficacy: weak since the fraction of filtered Na load reabsorbed at thus site is only 2-5% of the filtered Na+ load. Mechanism of action 1-Block of aldosterone receptors (spironolactone &eplerenone): 2-Direct inhibition of Na+ transport though specific Na+ channels in late part of the DCT and the collecting tubules. e.g. triamterene and amiloride. Uses of K+ Sparing Diuretics 1-Commonly given with loop acting or thiazide diuretics to balance the excessive K+ loss and to limit the incidence of metabolic alkalosis that occurs at the same setting during use of loop acting or thiazide diuretic. 2-Cases of hyperaldosteronism either primary (Conn's syndrome) or secondary (CHF, hepatic cirrhosis, nephrotic syndrome) especially spironolactone. 3-Refractory edema (with potent diuretics to potentate their diuretic action). Side Effects of K+ Sparing Diuretics 1-It may cause hyperkalemia due to decrease k+ secretion. This occurs especially in patients on high K+ intake or in patients with severe renal insufficiency or in-patient treated with other drugs that cause potassiumsparing effect e.g. beta-blockers, non-steroidal anti-inflammatory drugs, angiotensin converting enzyme inhibitors or angiotensin receptor blockers. 2-Hyperchloraemic metabolic acidosis. 3-Nausea, abdominal pain, drowsiness and mental confusion. 4-Spironolactone, lead to gynecomastia and impotence in males and menstrual disordersin females. Contraindications of K+ Sparing Diuretics In presence of hyperkalemia In combination with other K+ sparing drugs or with K+ supplements. In-patient with chronic renal insufficiency. Drug interactions Administration with ACE inhibitors and other agents causing hyperkalemia or potassium supplements may cause hyperkalemia. ►Indications of diuretics in hypertension: 1-Thiazides are given as initial therapy in most cases of essential hypertension. 2-Loop diuretics are given in hypertensive emergencies. 3-Hypertension associated with salt and water retention: e.g. Congestive heart failure (CHF). Chronic renal failure (give loop diuretics). Liver cirrhosis (give spironolactone). Primary hyperaldosteronism (give spironolactone).