* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 3.1_Cardiac_Physiology_
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
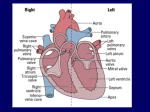
ANATOMY & PHYSIOLOGY II Lecture #3: Cardiac Physiology Name I. Characteristics of Cardiac Muscle A. Microscopic Anatomy 1. Similarities to skeletal muscle a. Striated – cells have actin and myosin arranged in A and I bands with Z discs, etc. b. Cellular components – most are the same, including a sarcoplasmic reticulum and T tubules. 2. Differences from skeletal muscle a. Branching cells form a connected network throughout the heart wall. b. Intercalated discs connect neighboring cells. These contain gap junctions that allow the flow of ions between neighboring cells so that cardiac muscle fibers are electrically linked. This allows them to behave as a single functional unit. c. Have one central nucleus in each cell (skeletal muscle fibers have many along the sides.) d. Have many mitochondria so they rely almost solely on aerobic metabolism for ATP production. B. Two Types of Cardiac Muscle Cells 1. Contractile cells (99%) do the work of muscle contraction. 2. Autorhythmic cells (1%) release electrical impulses to maintain the rhythm of heart contractions. These are scattered throughout the myocardium and function more like nerve cells than muscle. Automatic intrinsic rate of depolarization - these cells automatically depolarize at regular intervals, sending an electrical impulse to the contractile cells around them. These cells form the intrinsic conduction system of the heart. C. Contraction of Cardiac Muscle 1. The basic mechanism is the same as for skeletal muscle. 2. But contraction of cardiac muscle has some important differences: a. Cardiac muscle is stimulated to contract by cells of the intrinsic conduction system, not by nerve impulses. b. The whole organ contracts as a single unit. It is not divided into smaller motor units. c. Cardiac muscle has a long absolute refractory period. This means it cannot be stimulated to contract again while it is in the process of the first contraction. This prevents tetany (continuous contraction without a relaxation period in between contractions). d. Cardiac muscle produces long, sustained contractions as a result of slow Ca+2 channels. These allow entry of calcium from outside of the cell, which lengthens the period of depolarization. 2 D. Effect of Calcium 1. Background - calcium is a stimulatory ion for cardiac muscle contraction. 2. Contractile cells respond to increased calcium levels by contracting more forcefully. 3. Autorhythmic cells are depolarized mainly by calcium (not sodium). An increased calcium level causes them to depolarize more rapidly, so it increases their firing rate. To Do: Answer the following questions: 1. Which cells form the intrinsic conduction system? a) contractile cells b) autorhythmic cells 2. What stimulates a cardiac muscle cell to contract? a) nerve impulses b) cells within the heart 3. What prevents the heart from going into tetany? a) a long absolute refractory period b) slow calcium channels 4. Slow calcium channels cause: a) the heart to work as a single unit b) long, sustained contractions 5. Calcium causes contractile cells to: a) contract more forcefully b) depolarize more rapidly. II. Intrinsic Conduction System - For the heart to maintain its functional rhythm it needs specialized cells that form an electrical conduction system. A. The Conduction System Has Five Components: 1. Sinoatrial node (SA node) Located in the right atrium near the entrance of the SVC (sinus venarum region). Intrinsic rate of depolarization – about 75 times per minute under normal conditions (most rapid) When the SA node fires it sends impulses throughout both atria. These impulses then reach the second component (via the atrial myocardium and the internodal pathway): 2. Atrioventricular node (AV node) Located in the interatrial septum just above the tricuspid valve. Intrinsic rate – slower than the SA node (about 50 /min). Impulses next go to the: 3. Atrioventricular bundle (AV bundle or bundle of His) Location – begins at the bottom of the interatrial septum. This is the only electrical connection between the atria and the ventricles. It is short, and branches into the: 4. Right and left bundle branches Location – these travel along the right and left side of the interventricular septum towards the apex. 5. Purkinje fibers Location – these begin in the lower end of the interventricular septum, then do a U-turn at the bottom where they branch profusely. They carry impulses throughout the myocardia of the ventricles. 3 Contraction begins at the apex and sweeps upwards pushing blood towards the exit vessels. Intrinsic rate – slowest of any part of the conduction system (about 30 /min). To Do: Label the following structures on this diagram. a. b. Sinoatrial node Atrioventricular node c. d. Atrioventricular bundle Right & left bundle branches e. Purkinji fibers B. Establishing the Basic Heart Rhythm 1. SA node – because the SA node has the fastest intrinsic rate of depolarization, its impulses override the others and determine the rate at which the cardiac muscle contracts. Thus the SA node is called the pacemaker. Pacemaker - the portion of the conduction system that sets the pace at which the heart beats. 2. AV node – if the SA node stops functioning the AV node takes over. 3. Ectopic pacemaker – a pacemaker other than the SA node. 4. Sympathetic and parasympathetic nerve fibers modify the basic heart rate. III. Cardiac Cycle A. Terminology 1. Cardiac cycle - the events of one complete heart beat. 2. Systole (sis' toley) - the contraction phase 3. Diastole (dye ass' toley) - the relaxation phase B. Timing - One cycle lasts 0.8 sec (when the heart rate is 75 beats/min) 1. Overview a. Atria - the two atria contract at the same time, slightly before the ventricles. 4 b. Ventricles - the two ventricles contract at the same time, just after the atria. C. Events of One Cardiac Cycle 1. The SA node depolarizes, causing the atria to contract and send blood into the ventricles. - The AV valves are open, and the semilunar valves are closed. 2. The impulse pauses for 0.1 sec at the AV node to allow the atria to finish pushing blood into the ventricles. The atria then relax until the next cycle. 3. The impulse travels down the AV bundle, through the right and left bundle branches to the Purkinji fibers, which cause the walls of the ventricles to contract. This starts at the bottom and moves upwards to push blood up towards the pulmonary trunk and aorta. - The pressure of the blood against the valves CLOSES the AV valves and OPENS the semilunar valves. - Closing of the AV valves causes the first heart sound (“lub”). 4. Blood rushes up into the pulmonary trunk and aorta for about 0.3 secs. This is called the ejection period. 5. As the ventricles begin to relax, blood starts to flow backwards into the ventricles, but this causes the pouches of the semilunar valves to fill. - Closing of the semilunar valves causes the second heart sound (“dub”). - Soon after this the AV valves open again, because the pressure in the ventricles becomes less than that in the atria. 6. All four chambers relax for about 0.4 sec (this is diastole) until the next cardiac cycle begins. During this time the atria fill with blood and much of this blood flows directly into the ventricles, so that 80% of ventricular filling actually occurs during diastole. D. On the ECG (electrocardiogram): 1. P wave - caused by atrial depolarization (during contraction of the atria). 2. QRS complex - caused by ventricular depolarization (during contraction of the ventricles). 3. T wave - caused by ventricular repolarization (during diastole while ventricles are relaxed). - Atrial repolarization occurs during the QRS complex but is obscured by ventricular activity. To Do: 1. Number the events below from 1-6 to indicate the order in which they occur. Venticles contract Ventricles relax Atria contract Blood flows into pulmonary trunk and aorta Semilunar valves close 2. Label the P, QRS, and T waves below. 5 AV valves close IV. Cardiac Output A. Background 1. Cardiac output (cardiac minute output) - the amount of blood ejected from the heart every minute (specifically from the left ventricle). The quantity ejected from the left ventricle equals that ejected from the right ventricle. 2. Cardiac (minute) output = heart rate (beats/min) x stroke volume (ml/beat) = 5,250 ml = 75 beats/min x 70 ml/beat Thus, about 5 liters (all the body's blood) goes through the heart each minute. To Do: What would be the cardiac output if the heart was beating 100 times each minute and the left ventricle was pushing out 75 ml with each beat? B. Factors Affecting Cardiac Output - Cardiac output can be altered by changing stroke volume or heart rate. 1. Stroke volume – is mainly affected by preload, contractility, and afterload. a. Preload – the amount of blood entering the heart. This determines how much the heart muscle is stretched. 1) Frank-Starling Law of the Heart – the more the heart muscle is stretched, the more force it exerts when it contracts (Rubber Band Principle). 2) End-diastolic volume (EDV) – the amount of blood that collects in the ventricle during diastole. * EDV is the main thing affecting how much the heart muscle is stretched. EDV is affected by: a) Heart rate – a slower rate allows more time for filling and increases EDV. b) Venous return – rate at which blood is delivered to the heart by the veins. This increases during exercise due to squeezing of muscles and rapid breathing, which forces more blood back towards the heart. To Do: Answer the following questions: 1. Preload is determined by the amount of blood a) leaving the heart or b) entering the heart. 2. Preload affects a) stroke volume, b) contraction strength, c) cardiac output, or d) all three (a-c) 3. More stretching of the heart wall causes contraction strength to a) increase or b) decrease. 4. A faster heart rate would cause EDV to a) increase or b) decrease. 6 5. An increase in the preload will cause the cardiac output to a) increase or b) decrease. b. Contractility - strength of heart contractions independent of stretch and EDV. Stronger contractions result in more complete ejection of blood from the heart. 1) Contractility is increased by: a) Stimulation by the sympathetic nervous system b) Certain chemicals - epinephrine, Ca2+ ions, certain drugs like digitalis 2) Contractility is decreased by: a) Acidosis b) High extracellular potassium levels c) Calcium channel blockers c. Afterload – back pressure exerted by arterial blood. This is the pressure that must be overcome in order to force blood out of the ventricles. - Afterload is mainly a problem in people with high blood pressure. In this case, less blood is pumped out with each stroke, requiring the heart to contract more often (work harder) to pump the necessary amount of blood to the tissues. To Do: Answer the following questions: 1. An increase in contractility causes stroke volume to a) increase or b) decrease. 2. Circle the things that would cause contractility to increase: too many hydrogen ions an infusion of calcium excitement an infusion of potassium taking a calcium channel blocker taking digitalis 3. Hypertension (high blood pressure) causes afterload to a) increase or b) decrease. 4. An increase in afterload causes stroke volume to a) increase or b) decrease. 2. Heart rate - is affected by the autonomic nervous system, chemical regulation and some other factors. a. Autonomic nervous system regulation 1) Sympathetic nervous system - sympathetic nerve fibers release norepinephrine, which attaches to 1 adrenergic receptors. This increases the rate at which the pacemaker fires (as well as increasing contractility; see above). Norepinephrine 1 adrenergic receptors increases rate 2) Parasympathetic nervous system - vagus nerve fibers release acetylcholine, which slows the rate of the pacemaker. (Ventricles are sparsely innervated, so little effect on contractility.) Vagus nerve acetylcholine slows rate 7 * Under resting conditions the parasympathetic system is dominant and inhibits the SA node. (This is called vagal tone). If the vagus nerve is cut, the SA node fires about 100 times/min (vs. 75 when innervated). b. Chemical regulation 1) Hormones - release of epinephrine by the adrenal medulla stimulates the SA node 2) Ions - improper levels (either too high or too low) of calcium, sodium and potassium all can lead to potentially life-threatening problems. c. Other factors can affect the heart rate as well. These include: 1) age 4) activity level 2) gender 5) conditioning due to exercise 3) body temperature 3. Summary Cardiac output = Stroke volume x Heart rate Afterload Preload Contractility Sympathetic Parasympathetic EDV Starling’s law Hormones (epinephrine) Venous return Factor has a direct effect (an increase causes more cardiac output) Factor has an inverse effect (an increase causes less cardiac output) To Do: Answer the following questions: 1. Circle the factors that increase cardiac output: Increased venous return Increased afterload Epinephrine Decreased contractility Decreased parasympathetic activity Increased EDV 2. What has the least effect on stroke volume? a) contractility b) sympathetic activity c) parasympathetic activity d) afterload 3. What is the direct effect of increased parasympathetic activity? a) increases heart rate b) decreases heart rate c) increases stroke volume d) decreases stroke volume 4. Starling’s law describes how preload affects: a) afterload b) heart rate c) contractility 8 Learning Objectives for Lecture #3: Cardiac Physiology After studying this material you should be able to: 1. Describe the similarities and differences between the microscopic anatomy of skeletal and cardiac muscle fibers. 2. Identify the two different types of cardiac muscle cells and know the function of each. 3. Describe the ways in which cardiac muscle contraction differs from skeletal muscle contraction. 4. Describe the effect of calcium on the heart. 5. Explain the function of the conduction system of the heart and the special feature of the cells that compose it. 6. List in order the components of the conduction system and know the location of each. 7. Identify the structures involved in establishing the basic heart rhythm. 8. Define the terms cardiac cycle, systole and diastole. 9. List the events of a single cardiac cycle, explain what causes the opening and closing of the AV and semilunar valves during the cardiac cycle, and identify the source of the first and second heart sounds. 10. Identify the events of the cardiac cycle that produce the various waveforms seen on an ECG. 11. Define the following terms: cardiac output, preload, end-diastolic volume (EDV), contractility, and afterload and explain how they are interrelated. 12. Decribe the Frank-Starling law of the heart and explain how it effects stroke volume and contractility. 13. Calculate cardiac (minute) output if given the heart rate and stroke volume. 14. Identify the various factors that influence cardiac output and the mechanism by which each works to either increase or decrease output. The following CD-ROM, while not required, may help you to visualize the material covered in this lecture. This is available on reserve in the LRC. It is also part of the Interactive Physiology CD that was packaged with new editions of the textbook, and is available online at www.interactivephysiology.com. Use the same user name (login) and password as for the MyA&P website that goes along with the textbook (the course ID is quale29285): Interactive Physiology, “Cardiovascular System” Lecture #3: Cardiac Physiology – Answer Key Page 2 - Answer the following questions: B 1. Which cells form the intrinsic conduction system? a) contractile cells b) autorhythmic cells B 2. What stimulates a cardiac muscle cell to contract? a) nerve impulses b) cells within the heart A 3. What prevents the heart from going into tetany? a) a long absolute refractory period b) slow calcium channels B 4. Slow calcium channels cause: a) the heart to work as a single unit b) long, sustained contractions A 5. Calcium causes contractile cells to: a) contract more forcefully b) depolarize more rapidly. Page 3 - Label the following structures on this diagram. a. b. Sinoatrial node Atrioventricular node c. d. Atrioventricular bundle Right & left bundle branches e. Purkinji fibers a. Sinoatrial node b. Atrioventricular node c. Atrioventricular bundle d. Right and left bundle branches e. Purkinji fibers Page 4 - 1. Number the events below from 1-6 to indicate the order in which they occur. 2 Venticles contract 5 Ventricles relax 1 Atria contract 4 Blood flows into pulmonary trunk and aorta 6 Semilunar valves close 3 AV valves close 2. Label the P, QRS, and T waves below. P QRS T 2 Page 5 - What would be the cardiac output if the heart was beating 100 times each minute and the left ventricle was pushing out 75 ml with each beat? 100 x 75 = 7,500 ml Page 5 - Answer the following questions: B 1. Preload is determined by the amount of blood a) leaving the heart or b) entering the heart. D 2. Preload affects a) stroke volume, b) contraction strength, c) cardiac output, or d) all three (a-c) A 3. More stretching of the heart wall causes contraction strength to a) increase or b) decrease. B 4. A faster heart rate would cause EDV to a) increase or b) decrease. A 5. An increase in the preload will cause the cardiac output to a) increase or b) decrease. Page 6 - Answer the following questions: A 1. An increase in contractility causes stroke volume to a) increase or b) decrease. 2. Circle the things that would cause contractility to increase: too many hydrogen ions an infusion of calcium excitement an infusion of potassium taking a calcium channel blocker taking digitalis A 3. Hypertension (high blood pressure) causes afterload to a) increase or b) decrease. B 4. An increase in afterload causes stroke volume to a) increase or b) decrease. Page 7 - Answer the following questions: 1. Circle the factors that increase cardiac output: C Increased venous return Increased afterload Epinephrine Decreased contractility Decreased parasympathetic activity Increased EDV 2. What has the least effect on stroke volume? a) contractility b) sympathetic activity c) parasympathetic activity d) afterload B 3. What is the direct effect of increased parasympathetic activity? a) increases heart rate b) decreases heart rate c) increases stroke volume d) decreases stroke volume C 4. Starling’s law describes how preload affects: a) afterload b) heart rate c) contractility