* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cholinergic and Anti
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Psychopharmacology wikipedia , lookup
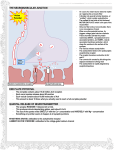
FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 1 of 9 I. II. III. IV. V. VI. NEOSTIGMINE [S19]: a. Yesterday, we were talking about cholinergic and anti-cholinergic drugs b. Remember acetylcholine- what it does and how it works i. Yesterday we focused on production and action of acetylcholine ii. Today we’re talking about cholinergic antagonists c. Before we turn to discussion of antagonists used to block action of acetylcholine, we will finish the discussion on inhibitors of acetylcholinesterase i. Drugs that inhibid acetylcholinesterase have the same effect as dugs that are direct agonists of acetylcholine ii. Indirect choilnomimetic drugs because they don’t bind to the acetylcholine receptors iii. Good test question- If you’re given a drug that is an acetylcholinesterase inhibitor 1. It’s site of action is at the acetylcholinesterase, not at the nicotinic or muscarinic receptor 2. Those drugs will stimulate the amount of acetylcholine in the synaptic cleft, so you will get both a nicotinic and muscarinic response 3. These drugs work at the level of the enzyme, not the level of the receptor 4. They are referred to as the indirect-acting cholinomimetic drugs TABLE 7-3 [S14] a. You’ll be responsible for effects of acetylcholine on different organs ACETYLCHOLINESTERASE [S15] a. The interaction of Acetylcholinesterase itself ACETYLCHOLINE [S16] a. The next few slides use the same cartoon setup b. The rectangular slide represents the surface of the enzyme i. So if you were to think about what the enzyme would look like, it might be a basketball ii. This is one little patch on the surface of the basketball but the site where acetylcholine binds c. Above is the structure of acetylcholine i. Has an acetyl region (right) and a choline (left) d. Drugs we’re talking about are analogs of acetylcholine- have structural resemblance to it i. When you think about effects, it helps to think about the fact that insecticides have their effect because of their structural similarity to acetylcholine ii. Because of that, they are able to interact with the acetylcholinesterase enzyme and block its action e. We will be looking at another slide like this but with other chemicals instead of acetylcholine- some drugs and some poisons INDIRECT CHOLINERGIC MIMETICS[S18] a. Neostigmine is charged and the others are not b. Edrophonium has a charge but is used for a specific niche i. Very ultra-short acting ii. Used for diagnosis of myasthenia and for the evaluation of a patient who is on anti-cholinergic therapy for myasthenia but the dosage is failing after a while because they have too much or too little of a drug- they use edrophonium to investigate that iii. The effects of these reagents: miosis, lower intra-ocular pressure, lower heart rate- all things that you would expect to happen when the acetylcholine level is higher NEOSTIGMINE [S19] a. Here we see Neostigmine, and over to the right are different chemicals that are members of the same familyedrophonium, neostigmine, physostigmine i. All of these have a group on the left that looks analogous to the acetate group and something on the other end that looks analogous to choline that you find in acetylcholine ii. Not exactly the same as acetylcholine because if it were it wouldn’t inhibit actions b. Neostigmine binds to the same enzyme site as acetylcholine i. Cleavage of this (top left) compound forms 2nd picture on left ii. With acetylcholine, you’ve got an acetate group, but with neostigmine you’ve got a carbamylated intermediate, so it stays on the enzyme longer before the bond can be clipped iii. Eventually, after a longer period of time, that bond gets clipped iv. The enzyme is temporarily inhibited, and as a result, less acetylcholine is broken down and the level of acetylcholine goes up c. You can give this drug every few hours to maintain acetylcholine levels that are higher than normal d. This is the mechanism of action of acetylcholinesterase inhibitors which are cholinomimetic because their effect is to increase the amount of endogenous acetylcholine present in the synaptic cleft FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 2 of 9 i. The person is still making acetylcholine, you’re not giving them a drug that looks like acetylcholine to bind to a receptor ii. Rather, you’re putting in a drug that looks like acetylcholine to inhibit the breakdown of acetylcholine iii. This is an indirect mimetic agent as opposed to a direct one VII. INSECTICIDE POISONING [S20] a. Insecticides penetrate the skin i. Very lipid-soluble so they can go across the skin ii. This is unusual- most drugs can get on your skin without much of an impact iii. With insecticides, a single drop can get on your skin and kill you 1. Nerve gas is the same way- a single inhalation of a very small dose will kill you b. What would be the effect of a drug that is an irreversible inhibitor of acetylcholinesterase? i. It would drop heart rate precipitously and cause you to die ii. This makes sense because it inhibits acetylcholinesterase VIII. ISOFLUOROPHATE [S21] a. Prototypical insecticide drug b. Has a phosphate group that is analogous to an acetate group i. You look at it and think it has nothing to do with acetylcholine, but it resembles the acetate group and can bind to same site on acetylcholinesterase c. Has isopropyl groups attached, so it reacts with the enzyme to form a complex that is somewhat stable i. If it were to fall off and be reversible: 1. You would go back to the initial form of the enzyme (with the OH) 2. The enzyme would be able to work again 3. But this doesn’t happen very much- this is a very limited reaction ii. Instead you have process called aging 1. The isopropyl group is clipped off instead of the phosphate 2. The enzyme is left with phosphate group on it permanently 3. When this happens, the enzyme is dead and you can’t regenerate it 4. So if you get this insecticide or a similar nerve toxin in your body, you can’t reverse the process d. What do you do for somebody who gets exposed to insecticide? What is the treatment approach? i. Give them something to bind to the insecticide- would be a good approach, but usually the insecticide has already done its thing 1. By the time the person gets to the emergency room, they are in a nonbreathing crisis ii. Give them something to upregulate acetylcholinesterase- would be good but it’s not possible 1. Once acetylcholinesterase is inhibited, you have to wait for your body to synthesize new acetylcholinesterase, which takes weeks iii. You basically have to breathe for the person and give them fluids for weeks until they recover 1. We aren’t that good at this supportive therapy, so usually people die when they are exposed to high doses e. The aging process takes 24-36 hours to be completed i. There is a drug called pralidoxime (PAM) competes for binding with the phosphate part of the molecule ii. If you put in PAM within 24 hours, it will react with the phosphate to form a new complex, and the enzyme will go back to its active native state iii. This is called rescuing the enzyme iv. So in the first 24 hours of insecticide poisoning, you can give this drug PAM, and you can partially rescue some of the enzyme f. So treat with supportive care + PAM + one other approach we haven’t mentioned yet g. What is the major cause of this person dying after being exposed to insecticide? i. Low heart rate and ischemia, which are caused by acetylcholine ii. Could you put in a drug to block the action of Ach? 1. One suggestion is norepinephrine a. Has opposite effects from acetylcholine, so it could be beneficial b. How would your body respond to this crisis? i. With insecticide poisoning and massive amounts of acetylcholine, your heart rate would slow and you would get bronchoconstriction ii. Your body tries to do the opposite 1. Goes into massive fight or flight response with your adrenal gland pumping out tons of epinephrine 2. Tries to stimulate all the ß1 and ß2 receptors it can to keep body from shutting down FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 3 of 9 iii. But you’ve got so much acetylcholine you can’t overcome it c. So you’re body will already be releasing the norepinephrine d. Theoretically, you could give more- for example an Epi-pen would give a beneficial shot of epinephrine e. But in a way, you can’t overcome the effects of acetylcholine by stimulating the opposite reaction h. Nicholas Cage movie about Alcatraz where nerve gas on the island- he takes a big syringe and jabs it into himself to inject something that saves his life i. Injected atropine ii. Atropine blocks acetylcholine receptors- topic of the next part of our talk is drugs that block acetylcholine receptors iii. Think about this scenario- this guy has massive amounts of acetylcholine 1. If you give a drug that blocks its binding to the acetylcholine receptor, you will diminish effects of acetylcholine iv. This is not a common scenario- only take atropine in an emergency situation where you’re trying to block an excessive amount of acetylcholine i. Some derivatives of atropine are used by optometrists everyday in their office IX. INSECTICIDE POISONING [S22] a. Here is your treatment for insecticide poisoning b. Treat with Pralidoxime if you get it within 24 hours c. Then treat with atropine to relieve the symptoms of excess ACh X. EFFECTS OF ANTICHOLINESTERASE AGENTS [S23] a. Effects of acetylcholinesterase agents on humans should be recognizable to you b. Test question: What does an insecticide do to heart rate? To eyes? To lungs? To intestines? c. It all represents a situation where acetylcholine is present at very high levels XI. SAMPLE QUESTION (INDIRECT-ACTING CHOLINOMIMETIC) [S24] a. Which of the following is an indirect-acting carbamate cholinomimetic drug with poor lipid solubility and a duration of action of about 2-4 hours? b. Acetylcholine wouldn’t be indirect- it acts directly on the receptor i. Could think about acetylcholine if the question asked for a direct-acting c. Bethanechol is an acetylcholine mimetic agent that binds to a receptor- direct acting d. Physostigmine i. Inhibits acetylcholinesterase, so it is an indirect mimetic ii. Not charged, so it is fairly lipid-soluble and can enter the CNS iii. Close but not right e. Pilocarpine- a natural analog that has cholinomimetic actions by binding to receptors f. Neostigmine i. Indirect-acting cholinomimetic ii. Binds to acetylcholinesterase and inhibits its activity iii. Carries a positive charge iv. So it is an indirect-acting carbamate cholinomimetic drug with poor lipid solubility, so it’s the right answer g. These are the kinds of test questions he likes to give, so think about this one XII. OTHER DRUGS THAT AFFECT ACETYL CHOLINE SYNTHESIS AND RELEASE [S25] a. Hemicholinium looks like choline, so it competes with and blocks choline reuptake b. Vesamicol inhibits the uptake of acetylcholine inside the cell and into the vesicles c. Botox inhibits release of acetylcholine from the vesicles by preventing them from binding to the cell surface and being released d. Be familiar with the mechanism of action of these 3 drugs XIII. ANTICHOLINERGIC DRUGS [26] a. Atropine- grandfather of the group i. Blocks binding specifically to muscarinic receptors 1. Today we’re talking about anti-muscarine drugs, used for a variety of purposes 2. There are anti-nicotinic receptor drugs a. Neuromuscular blocking agents like curare b. We will talk about them later when we talk about anesthesia c. Used in surgical procedures to cause paralysis of the diaphragm ii. Atropine has long duration of action- over a week, so not used for must clinical situations 1. Chemists have made analogs of atropine that have shorter half-lives XIV. ATROPINE ANALOGS [S27] FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 4 of 9 a. You need to know these four drugs because there will be questions about them b. 3 of these 4 have “atropine” (trop) in the word and are atropine derivatives c. Tropicamide i. Used by optometrists ii. Causes mydriasis and cycloplegia 1. Mydriasis and miosis refer to how wide pupil is open a. Miosis i. Pinpoint pupils/ dilated very small (helps to remember that miosis is the smaller of the two words) ii. Cholinergic system b. Mydriasis i. Eye wide open ii. Fight or flight response, eyes open so you can see escape- adrenergic system iii. Another way to get the eye wide open (other than stimulating fight or flight) is to block the cholinergic stimulus (acetylcholine) so the adrenergic response predominates 2. Cycloplegia a. Paralyze eyes so they can’t focus b. Muscles that control the size and shape of the lens are innervated by acetylcholine and norepinephrine c. Blocking the action of acetylcholine prevents muscles from contracting and causing the lens to change shape, so you can’t focus eyes for reading iii. Blocks the action of acetylcholine from binding to its receptor d. Ipratropium i. Given in the form of an inhaler- tells you that its site of action is in the lungs ii. Blocks action of acetylcholine in the lungs 1. Acetylcholine in lungs causes bronchoconstriction 2. So if you block the bronchoconstriction, bronchodilation effect from the adrenergic system predominates iii. If you’re having difficulty breathing from asthma, what two drugs could you give to stimulate drugs to bronchodilate? 1. Could you give a cholinergic agonist and ß agonist and get what you want? a. ß2 agonist i. ß2 receptors are the ones found in the smooth muscles of the lungs ii. Would dilate bronchioles (fight or flight response) b. Cholinergic agonist would cause constriction c. So cholinergic and adrenergic agonists put together would cancel each other out- the ß adrenergic agonist would bronchodilate and the cholinergic agonist would bronchoconstrict d. Not a good plan 2. What if you put in a ß antagonist and a cholinergic agonist? a. Would cause constriction and constriction – wouldn’t be able to breathe b. Not a good plan 3. What if you put in a cholinergic antagonist and ß agonist? a. Dilation and dilation b. The two drugs would work in tandem c. What we give kids with asthma to open up the airways iv. So Ipratropium is part of asthma therapy because it blocks acetylcholine action and causes bronchodilation e. Benztropine i. Used in Parkinson’s disease- an important and devastating disease ii. Since it’s used in Parkinson’s disease, you can predict that it must be lipid soluble to get into the CNS iii. We don’t know the exact cause of Parkinson’s disease, but the major defect underlying Parkinson’s is that dopamine levels (a neurotransmitter) are diminished 1. Plaques in the brain tissue are associated with Alzheimer’s not sure about Parkinsons iv. So why would we treat Parkinson’s with a cholinergic blocker? Why not a dopamine agonist or replenisher? 1. We don’t understand the CNS enough, but dopamine and acetylcholine probably interact with each other 2. Many neurons in the CNS have multiple receptors and modulate each other’s effects so that dopaminergic neurons can increase or decrease their activity as a result of cholinergic neurons impacting them and releasing acetylcholine and vice versa so you have feedback loops FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 5 of 9 3. If you have a deficit of dopamine, you act as if you have too much acetylcholine 4. If you give someone a moderate dose of an acetylcholine blocking agent, the symptoms of Parkinson’s disease improve a little a. You don’t want to put a lot in, but you want to tweak the system a little to dampen down the acetylcholine level f. Scopolamine i. Used for motion sickness, another CNS problem ii. So it has to be lipid-soluble to get to the CNS iii. Neurons that stimulate the motion sickness pathway use cholinergic innervation iv. Block acetylcholine to dampen the amount of seasickness v. Problem with this is dry mouth afterwards 1. This is an anti-cholinergic symptom because blocking acetylcholine blocks secretions all over the body, including the mouth 2. Dentists can anticipate dry mouth in patients taking anti-cholinergic drugs and can use this history to help them get symptomatic relief XV. ATROPINE [S28] a. Blocks the acetylcholine binding to muscarinic receptors- ALWAYS A TEST QUESTION on national boards and his tests b. Long duration of effects c. Analogs with shorter half-lives have been developed XVI. EFFECTS OF MUSCARINIC BLOCKING DRUGS [S29] a. On the skin, they inhibit sweating, so you get dry b. On the eyes, you get cycloplegia i. Get an increase in aqueous outflow resistance, so be careful with how it would interact with a patient who has glaucoma c. Digestive, urinary, cardiovascular effects i. Bradycardia at low dose ii. At high dose, you get an increase in cardiac output XVII. TABLE 8-2 [S30] a. These are the atropine analogs we use- atropine, scopolamine, homatropine, tropicamide b. This is their duration of action c. Tropicamide used in the examination of getting an eye to dilate has the shortest half-life XVIII. ALZHEIMER’S DISEASE [S31] a. Final place where we use these drugs is in treatment of AD b. You may have heard of tacrine- a drug that has been around for a long time c. We don’t have good treatment for AD, a fatal disease d. When people die from AD, they regress in their ability to think, eat, swallow, and finally to breathe- like they return to the fetal state with all of the neural pathways being shut down e. Acetylcholine isn’t the single answer to this problem i. Symptomatically you get neurofibrillary tangles and a diminishing of the normal neural circuitry in brain, so you get some symptomatic relief from acetylcholinesterase inhibitors ii. Not satisfactory because it is a mono-component approach to a multi-component disease, but it is better than nothing iii. We don’t really have something that addresses AD in a very good way right now XIX. SAMPLE QUESTION- ATROPINE OVERDOSE [S32] a. Atropine overdose- Which one of the following would you expect with an overdose of atropine? b. What kind of drug is atropine? What does it do? i. You can go back to the fight or flight response to think about this ii. Binds to cholinergic receptors and prevents acetylcholine from binding iii. So if you have acetylcholine receptors that normally respond to acetylcholine, that effect would be blocked c. So GI smooth muscle cramping, an increase in cardiac rate, an increase in gastric secretion, an increase in constriction of the pupils, or an increase in urine production? d. Effect of acetylcholine on heart ratei. Fight or flight- heart rate goes up ii. Acetylcholine- heart rate goes down iii. So blocking acetylcholine action causes heart rate to increase e. You have to walk through the process for all of these questions FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 6 of 9 ANTIHISTAMINE LECTURE I. MAST CELLS CONTAIN MEDIATORS THAT CAUSE INFLAMMATION [S27] a. Typically focus on mast cells and basophils when we talk about antihistamines b. Mast cells i. Cells found in tissues that are sensitive to stimuli ii. Usually associated with histamine in an allergic response 1. Runny nose, hay fever, pain, itching, redness, swelling, hives 2. Response to some irritation 3. Histamine is a key player in that response 4. Usually a good thing- your body has it there to protect you and alert you when something bad is happening c. But some people have excessive amounts of IgE i. When they are exposed to a common pollen, they get an over-aggressive response to it ii. They get an increased amount of histamine release, which can feel pretty nasty iii. So drugs have been developed to block that effect- anti-histamines d. Histamine receptors are actually cousins to the cholinergic receptors i. Remember how acetylcholine works biochemically 1. Some of the receptors are involved in activation of phospholipase C and release of DAG and IP-3, which stimulates the release of calcium, which causes muscle contraction 2. The other receptors are involved in cyclic AMP inhibition ii. Histamine receptors have these two components as well as a third type of receptor which stimulates cyclic AMP production e. So histamine has four receptors i. You mainly hear about the H1 receptor (99% of what you read about in books) ii. H2 receptor involved in acid secretion by the stomach iii. H3 and H4 receptors have been new developments 1. We don’t have drugs to block their action yet 2. H3 and H4 antagonists will be available in the future f. Histamine is made in mast cells, and mast cells also have enzymes and lipid-derived mediators like prostaglandins, leukotrienes, and cytokines- so a whole mix of stuff i. When mast cells get activated, they dump out histamine to get an immediate response ii. The other stuff is also dumped out, and it goes to other cells and causes a later response iii. So if I scratch my skin, I will get redness iv. If I inject histamine into my skin, I will develop a flare – a redness and a white area of irritation 1. This is explained by the fact that mast cells contain both histamines and these other chemicals that all have effects locally and with other cells II. MAST CELL [S28] a. Here is what a mast cell looks like b. Granules are full of stuff waiting to be released i. This stuff causes edema, pain, redness, and itching ii. Doesn’t cause anything until it is released iii. This is the reason why we feel the symptoms iv. These little vesicles contain histamine, leukotrienes, and other reagents that are all involved in the process of itching and pain III. MAST CELLS WAIT TO BE ACTIVATED [S29} a. They are waiting to be activated b. IgE stimulates allergic response to a lot of things like pollen, foods, drugs, insect venoms, etc c. You also have anaphylatoxins if you have an anaphylactic response d. Drugs like opiates may cause immediate release of histamine- very uncomfortable e. Some people with asthma have an unfortunate hypersensitive reaction to a small amount of aspirin that causes an immediate release of histamine f. You can also get stimulation by heat, cold, or trauma g. You can sometimes get an autoimmune response IV. HISTAMINE [S30] a. Synthesized and stored in mast cells b. High concentrations found in tissues that are sensitive to exposure- in the skin, mucosa of the bronchial tree, and in the intestines c. Histamine has no clinical application FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 7 of 9 i. You would never give histamine for something and there are no histamine agonists ii. Histamine is a nasty chemical that causes side effects iii. But you do give anti-histamines/ histamine antagonists d. Released after an antigen binds to IgE e. Has four receptors: H1, H2, H3, and H4 V. HISTAMINE [S31] a. Produced almost exclusively in basophils of mast cells b. Cause itching and increase in vascular permeability, increase in vasodilation, and smooth muscle contraction, and gastric acid secretion i. Gastric acid secretion from H2 receptor in the stomach 1. H2 receptor works by increasing cAMP ii. H1 receptor works by releasing calcium inside the cell c. The histamine H1 receptor is confusing because they are on both endothelial cells and vascular smooth muscle cells i. Remember yesterday’s diagram of a blood vessel with endothelial cells on the inside and smooth muscle cells around it 1. Smooth muscle cells have nerve endings where norepinephrine can bind 2. Endothelial cells have receptors that can respond to epinephrine present in the bloodstream 3. Like a garden hose- endothelial cells on the inside and smooth muscle cells on the outside ii. In this case, there are histamine receptors on both kinds of cells 1. On endothelial cells, histamine causes edema from blood vessels getting leaky a. What usually prevents vessels from getting leaky? How are the endothelial cells usually aligned with each other? i. They are tightly linked from cell to cell so stuff doesn’t get out of the blood vessels b. Histamine binds to the receptors and causes cells to change their conformation i. The endothelial cells pull apart from each other ii. Stuff in blood vessels can then leak out into tissues c. So if I have a pollen in my nose that causes my mast cells to release histamine, the histamine released in the endothelial cells causes them to pull apart so the liquid in the bloodstream comes out of the blood vessels and causes a stuffy nose- histamine-stimulated congestion or edema 2. At the same time, your body tries to overcome this by causing vasoconstricton because you have histamine receptors on smooth muscle cells that cause constriction 3. Some areas of your vascular bed have more H1 receptors than others- so constriction in some areas and dilation in others- this is complex iii. The net effect of histamine release is that you get vasodilation 1. These receptors would ordinarily cause vasoconstriction, so there must be something else going on 2. Endothelial cells are releasing nitric oxide (endothelial-derived releasing factor) which is the most potent vasodilator we have iv. So histamine is doing 2 things that are opposing each other 1. Causes smooth muscle contraction, which would tend to close blood vessels 2. Stimulates endothelial cells to release NO, which causes massive vascular dilation 3. Contraction and dilation are going head-to-head, and vasodilation wins a. Doesn’t make sense when you just look at histamine causing receptors that causes the release of calcium and contraction of smooth muscle cells b. There may be a self-limiting amount of vasodilation because the endothelial cells are stimulating NO, which causes dilation, and histamine is trying to cause constriction at the same time v. Certain beds like the smooth muscle in the stomach have pronounced constriction- important effects on the GI tract, which don’t make sense unless you understand that histamine causes smooth muscle contraction vi. In vascular beds where you have mast cells nearby and you have release of histamine, the predominant effect is the endothelial cell effect to cause dilation and pulling apart of endothelial cells, which causes edema FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 8 of 9 1. This is the effect that predominates in your nasal cavity and eyes where you get tearing and a stuffy nose 2. This wins out because of the number of receptors that are there for histamine vii. Complicated because you have vasodilation and smooth muscle contraction occurring at the same time VI. SYSTEMIC EFFECTS [S32] a. What is the effect in the rest of the body? b. In the cardiovascular system, the vasodilation of small blood vessels leads to a fall in blood pressure, which leads to a decrease in peripheral resistance i. For example, a scorpion bite/ venomous bite can cause an anaphylactic response in which blood pressure falls precipitously and can be life-threatening- histamine plays part of the role in that 1. You get increased capillary edema as well c. In the bronchioles, you get constriction because of H1 receptors d. In the GI tract, you get contraction and cramping of the smooth muscle cells e. The H2 receptor in stomach is responsible for acid production i. So some drugs that diminish acid secretion are inhibitors of H2 receptors- ranitidine and cimetidine are two of the more famous ones, famotidine is out there as well now f. In the nervous system, it stimulates itching and pain with H1- very uncomfortable VII. ALLERGIC DISEASE [S33] a. What happens in allergic rhinitis- you get dermatitis, urticaria, asthma, anaphylaxis b. All of these immediate responses happen as a result of histamine release VIII. CARTOON [S34] a. Can be violent as to how much stuff comes out of you in response to histamine IX. ALLERGIC RHINITIS EPIDEMIOLOGY [S35] a. 10% Americans have allergic rhinitis b. Most commonly kids, improves in middle age c. Very strong family history and certain stimulants will stimulate it X. GIRL WIPING HER NOSE [S36] a. Pediatricians can pick up on allergic kids that don’t know they have it because of the little crinkle in their nose from doing this XI. ANTIHISTAMINES IN ALLERGIC RHINITIS [S37] a. Symptoms can be affected by antihistamines b. Sneezing, pruritis, rhinorrhea, congestion, and late-phase reactions c. Antihistamines are effective in these immediate responses but not in the late-phase responses XII. REDUCTION OF HISTAMINE EFFECTS [S38} a. How do you reverse the effect of histamine? b. Epinephrine- has the opposite actions of histamine i. If you have a severe anaphylactic response (such as spider bite), you can give an epi-pen to help overcome the effect of histamine ii. Increases heart rate and blood pressure c. Drugs called mast cell stabilizers i. We don’t know how they work ii. Prevent mast cells from releasing as much histamine when they’re stimulated iii. Ex- runners with allergic asthma have problems on cold mornings, take this to as a stabilizer to prevent amount of histamine released so they will have less of an allergic response to a cold, early morning run d. There are 2 generations i. First generations get into brain and cause side effects of sedation 1. These are sometimes good- make a child with a runny nose sleepy, good for parents 2. Reversible, competitive antagonists of H1 receptors ii. 2nd generations designed to not cause this side effect of sedation 1. So if you’re giving anti-histamine drugs to a truck driver or you on your way to class, and you don’t want to sleep through your lecture, take a 2 nd generation antihistamine 2. Can’t enter the brain and doesn’t cause sedation iii. Distinction makes sense chemically: make 2nd generation more polar or give it charge so it can’t enter brain and cause sedation XIII. HISTAMINE H1 RECEPTOR [S39] a. H1 receptors are involved in allergic rhinitis and are similar to M1, M3, and M5 cholinergic receptors FUNDAMENTALS II: 10:00-11:00 Scribe: LOUISA WARREN 12/3/2010 Proof: ASHLEY RUSSELL PILLION CHOLINERGIC AND ANTI-CHOLINERGIC DRUGS AND ANTIHISTAMINES Page 9 of 9 b. Work by increasing a phospholipase C cascade that produces IP-3 and DAG, which stimulate muscle contraction c. Found in smooth muscles of the intestine and blood vessels of trachea d. Also found in vascular endothelial cells- stimulate cells to pull apart and release NO, a potent vasodilator XIV. HISTAMINE H2 RECEPTOR [S40] a. The H2 receptor works differently b. It stimulates adenylate cyclase, which increases the level of cyclic AMP, so it is similar to a ß-adrenergic receptor c. Found in the stomach, heart, some smooth muscle, brain d. It’s kind of interesting that you have acetylcholine receptors that work by increasing the release of calcium and ß-adrenergic receptors that work by increasing the amount of cyclic AMP, and you’ve got muscarinic receptors that work by inhibiting the levels of cyclic AMP, and now histamine receptors i. Some histamine receptors work by increasing the level of calcium, some work by increasing cyclic AMP ii. What is cool is that there are H3 receptors that are presynaptic and have the opposite actionthey decrease the amount of cyclic AMP that is formed 1. So some neurons secrete histamine as a neurotransmitter, and they probably have an autoregulation by H3 receptors 2. We don’t have any drugs yet that work there, but if someone comes up with an H3 agonist, it will most likely turn off the release of histamine from the presynaptic membrane 3. It is very likely that in the future someone will develop an H3 antagonist that will dampen histamine release 4. An H3 antagonist would be a bad thing- we won’t see them because they would stimulate histamine release XV. H1 RECEPTOR ANTAGONISTS [S41] a. Sedation is the big side effect of H1 antagonists i. Also cause dryness of the mouth ii. Somewhat anti-cholinergic effect iii. Paradoxical effect in some kids 1. Most kids, when given Benadryl, Dramamine, or other drugs like that, they get sleepy 2. 10% have opposite effect- they get wired and can’t sleep a. We don’t know why that is b. Probably because of some pharmacogenetic difference b. Also used to prevent nausea, vomiting, motion-sickness i. Some overlap with cholinergic system there c. Sometimes used to suppress tremors, but that is not commonly done XVI. 1st GENERATION ANTIHISTAMINES (BLOCK H1 RECEPTORS) [S42] a. We don’t use brand names in the course, but I put them here so you would recognize that some of these drugs like Dimenhydrinate, Diphenhydramine, and Promethazine are widely used in medicine b. Many are available over the counter c. Took one by injection for food poisoning because couldn’t take pills- quieted vomiting d. Used a lot OTC for stuffy nose, sleep aids, and motion sickness e. Phenylephrine was previously added in combination with these drugs, but it was taken away from OTC availability because it was used to make drugs i. Now not usually in combination with these compounds f. For test purposes, you definitely need to know Dimenhydrinate, Diphenhydramine, Chlorpheniramine, and Promethazine i. These 4 are on almost every test/ national boards ii. Know that these are all antihistamines [End 52:30 mins]