* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Answers to WHAT DID YOU LEARN QUESTIONS
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
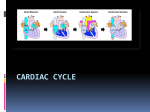
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
McKinley/O’Loughlin Human Anatomy, 2nd Edition CHAPTER 22 Answers to “What Did You Learn?” 1. Arteries carry blood away from the heart, and veins carry blood back to the heart. 2. The pulmonary circulation consists of the chambers on the right side of the heart (right atrium and ventricle) as well as the pulmonary arteries and veins. It carries blood to and from the lungs. The systemic circulation consists of the chambers on the left side of the heart (left atrium and ventricle), along with all the other named blood vessels. It carries blood to all the organs and tissues of the body. 3. The posterosuperior surface of the heart, formed primarily by the left atrium, is called the base of the heart. The inferior conical end is called the apex of the heart. It projects slightly anteroinferiorly toward the left side of the body. 4. The pericardium is composed of two layers: a fibrous pericardium attached to both the sternum and the diaphragm, and an inner serous pericardium. The serous pericardium has two layers: a parietal layer that lines the inner surface of the fibrous pericardium, and a visceral layer, which covers the outside of the heart. The space between the parietal and visceral layers is the pericardial cavity. It is a potential space with a very thin fluid lining, however, it may become a real space as it fills with fluid as a result of inflammation and infection. 5. A relatively deep coronary sulcus extends around the circumference of the heart and separates the atria from the ventricles externally. 6. Both the right and left ventricles are separated from the superior atria by AV valves, contain papillary muscles, and are lined by trabeculae carneae. The right McKinley/O’Loughlin Human Anatomy, 2nd Edition ventricle has thinner walls and pumps blood into the pulmonary trunk, while the left ventricle has thicker walls and pumps blood into the ascending aorta. 7. The chordae tendineae are thin strands of collagen fibers that attach to the cusp of the AV valve and prevent the valve from prolapsing (everting and flipping into the atrium) when the ventricle is contracting. 8. While the left and right coronary arteries share some tiny connections, called anastomoses, functionally they act like end arteries, which have no anastomoses and are the “end of the line” when it comes to arterial blood flow. 9. Differences between cardiac and skeletal muscle include: (1) the sarcoplasmic reticulum is less extensive and not as well organized in cardiac muscle; (2) cardiac muscle has no terminal cisternae; (3) a tight association of SER and Ttubules is lacking in cardiac muscle; (4) T-tubule distribution is reduced in cardiac muscle; and (5) T-tubules overlie Z lines in cardiac muscle instead of A–I junctions as in skeletal muscle. 10. The atrioventricular node is located in the floor of the right atrium, between the right AV valve and the coronary sinus opening. 11 Autorhythmic means that the heart itself (not external nerves) is responsible for initiating the heartbeat. 12. Sympathetic innervation increases the heart rate and the force of the heart contractions. 13. The contraction of a heart chamber is called systole. During this period, contraction of the myocardium forces blood either into another chamber (atrium to ventricle) or into a blood vessel (ventricle into the attached large artery). The McKinley/O’Loughlin Human Anatomy, 2nd Edition relaxation phase of a heart chamber is termed diastole. During this period, the myocardium of each chamber relaxes between contraction phases, and the chamber fills with blood. 14. Late ventricular diastole is a continuation of ventricular relaxation. The AV valve opens, and passive filling of the ventricle from the atria begins. 15. Flexibility and elasticity in connective tissue decrease with aging. As heart valves become slightly inflexible, both heart murmur and altered blood flow through the heart result. Answers to “Content Review” 1. The pulmonary circulation consists of the chambers on the right side of the heart (right atrium and ventricle) as well as the pulmonary arteries and veins. It conveys blood to the lungs via pulmonary arteries to exchange respiratory gases in the blood before returning to the heart in pulmonary veins. The systemic circulation consists of the chambers on the left side of the heart (left atrium and ventricle), along with all other named blood vessels. It carries blood to all the peripheral organs and tissues of the body for nutrient and gas exchange before returning the blood to the right atrium. 2. The heart is rotated such that its right side (right atrium and ventricle) are located more anteriorly, while its left side (left atrium and ventricle) are located more posteriorly. 3. The parietal layer of serous pericardium is a serous membrane that lines the inner surface of the fibrous pericardium, which supports the heart in the mediastinum. McKinley/O’Loughlin Human Anatomy, 2nd Edition The visceral layer of serous pericardium (also called the epicardium) is a serous membrane that covers the outside of the heart. Together, both layers produce serous fluid in the pericardial cavity to reduce friction as the heart moves during beating. 4. The fibrous heart skeleton is located between the atria and ventricles and is formed from dense irregular connective tissue. The function of the heart skeleton includes: (1) separation of the atria and ventricles, (2) anchor heart valves by forming supportive rings at the attachment point of the valves, (3) provides electrical insulation between atria and ventricles, and (4) provides a rigid framework for the attachment of cardiac muscle tissue. 5. Chordae tendineae are thin strands of collagen fibers that anchor into papillary muscles and attach to the cusp of the atrioventricular valves to prevent the valve from prolapsing (inverting and flipping into the atrium) when the ventricle is contracting. 6. The atria are thin walled because they do not need to generate high pressure to push blood into the ventricles. Most of the filling of the ventricles is passive, and the ventricles are inferior to the atria so moving blood into the ventricles from the atria is relatively easy. The right ventricle wall is relatively thin with respect to the left ventricle wall because the right ventricle only has to pump blood through the pulmonary circuit to the lungs immediately lateral to the heart, whereas the left ventricle must generate enough pressure to drive blood through the entire systemic circuit. McKinley/O’Loughlin 7. Human Anatomy, 2nd Edition The right coronary artery typically branches into a marginal artery (which supplies the right border of the heart) and the posterior interventricular artery (which supplies both left and right ventricles). The left coronary artery typically branches into the anterior interventricular artery (also called the left anterior descending artery, which supplies the anterior surface of both ventricles, most of the interventricular septum, and the circumflex artery (supplies left atrium and ventricle). 8. Cardiac muscle resembles skeletal muscle in that fibers in both muscles are striated and have extensive capillary networks that supply needed nutrients and oxygen. Cardiac and skeletal muscle differ in the following ways: (1) in cardiac muscle, the sarcoplasmic reticulum is less extensive than in skeletal muscle and not as well organized; (2) there are no terminal cisternae in cardiac muscle fibers; (3) T-tubule distribution is reduced in cardiac muscle and there is no close association between T-tubules and the sarcoplasmic reticulum; and (4) Ttubules overlie Z lines in cardiac muscle instead of A–I junctions as in skeletal muscle. 9. Sympathetic innervation increases heart rate and increases the force of the heart contractions. Parasympathetic innervation will decrease heart rate. Parasympathetic innervation tends to have no effect on the force of contractions, except in special circumstances. 10. The phases of the cardiac cycle are: atrial systole, ventricular systole (early and late), and ventricular diastole (early and late). (1) During atrial systole, the atria contract to pump blood into the ventricles to finish their filling. The AV valves McKinley/O’Loughlin Human Anatomy, 2nd Edition remain open and the ventricles are still in diastole from the previous cycle. The semilunar valves remain closed. (2) During early ventricular systole, the atria are now in diastole, the ventricles begin to contract and the AV valves close. The semilunar valves remain closed for a short period of time and then they are forced open. (3) During late ventricular systole, the atria remain in diastole, the ventricles continue contracting, the AV valves remain closed, and the semilunar valves remain open. (4) During early ventricular diastole, the atria remain in diastole, the ventricles enter diastole, the semilunar valves close, and the AV valves remain closed for a short period of time and then they open. (5) During late ventricular diastole, the atria remain in diastole, the AV valves remain open and the ventricles passively fill with blood, and the semilunar valves remain closed.