* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Urinary Incontinence Drugs
Nicotinic agonist wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Toxicodynamics wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
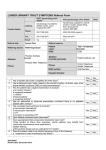
Urinary Incontinence Drugs Urge Incontinence- Detrusor Instability, Detrusor Hyperactivity w/ impaired bladder contractility or involuntary sphincter relaxation. Stress Incontinence (ST)- urethral sphincter failure – due to either anatomic changes or intrinsic sphincter deficiency (ISD). Overflow Incontinence- hypotonic or underactive detrusor due to drugs, fecal impaction, DM, lower spinal cord injury, disruption of motor innervation of detrusor, urethral obstruction or genital prolapse Mixed Incontinence- combination of urge and stress incontinence, especially common in older women. Tx: Pharmacological, Behavioral, Surgical. 1st choice should be the least invasive treatment w/ fewest potential adverse CI’s. Before tx- complete evaluation & appropriate urodynamic testing. Muscarinic Receptors – Role in treatment of Incontinence Muscle Receptor Location Effects of Antagonism MI Brain, salivary gland, SNS ganglia Impairment of memory & cognition, dry mouth, impaired secretion of gastric acid M2 Smooth muscle, hindbrain, cardiac Tachycardia, gastric sphincter tone M3 – Primary receptor for overactive Bladder Smooth muscle, salivary gland, eye Bladder and bowel contractility, dry eyes and mouth, abnormal vision M4 Brain, salivary gland Unknown CNS effects M5 Substantia Nigra, eye Unknown CNS effects, abnormal vision, in pilocarpine-induced salivation 1. Oxybutynin (Ditropan, Ditropan MOA – inhibits involuntary detrusor muscle contractions, delays desire to void, urgency & frequency, direct antispasmodic effect on smooth muscle. XL, Oxytrol) (B) Precautions – narrow angle glaucoma, elderly. DDI – CYP3A4 substrate & inhibitor Active metabolite – N-desethyloxybutynin ADRs – dry mouth, dry skin, blurred vision, sedation, change in mental status, nausea, constipation (severity of ADRs increases w/ dosage) 2. Oxytrol transdermal System (Expensive) Dose: 3.9 mg/day system applied 2x/ week (every 3-4 days), Because of dosing delivery, less incidence of dry mouth than other oxybutynin products. applied to dry, intact skin on abdomen, hip, or buttock, application site should be rotated w/ each application, avoiding re-application to the same site w/in seven days. 3. Oxybutynin (Investigational) UROS Infusor – uses a balloon reservoir filled w/ oxybutynin. This device is inserted into the bladder and releases drug over a period of several weeks. impregnated ring for intravaginal use. The drug would be released during a 28 day period. 4. Propantheline (ProBanthine)(C) MOA – inhibit involuntary detrusor muscle contractions. Prototype for Anticholinergic agents used for urologic conditions. Precautions – Narrow angle glaucoma, elderly ADRs – urinary retention, blurred vision, dry mouth, nausea, constipation, tachycardia, drowsiness & confusion 5. Tolterodine (Detrol, Detrol XL) (C) MOA – inhibits involuntary detrusor muscle contractions. Has greater affinity for muscarinic receptors in bladder than saliva ADRs – urinary retention, blurred vision, dry mouth, nausea, constipation, headache, drowsiness and confusion. Precautions – narrow angle glaucoma, elderly DDIs: CYP2D6 & CYP3A4 substrate 6. Darifenacin (Enablex) & Solifenacin (Vesicare) MOA – selective M3 receptor antagonist. Same precautions as other Anticholinergics ADRs – same as others, but less severs. Less CNS effects b/c does not cross blood brain barrier (especially solifenacin). DDis – CYP450 substrate 7. Tropsium Cl (Sanctura) MOA – M2 and M3 receptor blocker (similar to tolterodine) ADRs – same as others, less CNS side effects. Renally excreted – NO CYP450 drug interactions 8. Dicyclomine (Bentyl) (B) MOA – Direct Antispasmodic Smooth Muscle Relaxan t. Not as effective as other Anticholinergic agents. More often used for GI disorders like Irritable Bowel Syndrome. Tricyclic Antidepressants: Imipramine (Tofranil) More commonly used to treat nocturnal enuresis Useful b/c have Anticholinergic properties Not FDA-approved for incontinence Calcium Channel Blockers: Nifedipine (Procardia) May be useful b/c calcium is involved in urinary muscle contractions. Not FDA approved, not many clinical studies Nifedipine often used for Urinary Incontinence Estrogen Therapy Estrogen (oral or vaginal) as adjunct for postmenopausal women w/ stress incontinence or mixed incontinence. Conflicting data – some trials suggest hormone therapy may contribute to incontinence. Conjugated estrogens and medroxyprogesterone may be used. Alpha – 1 antagonists Used to treat overflow incontinence b/c will decrease sphincter tone. “azosin” drugs Nocturnal Enuresis – Pediatrics Desmopressin (DDAVP) (nasal spray) (PO) MOA – Enhances reabsorption of water in kidneys by increasing cellular permeability of the collecting ducts Dose: 100 mcg/mL nasal solution – Administer 10 – 40 mcg (0.1 – 0.4 ml) at bedtime. Give ½ the dose in each nostril. Usually tried for up to 6 months Doxepin (Sinequan) Amitriptyline (Elavil)