* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Drug discovery wikipedia , lookup
Pharmaceutical marketing wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Specialty drugs in the United States wikipedia , lookup
Pharmacogenomics wikipedia , lookup
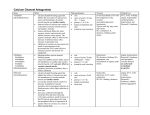
Orphan drug wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug interaction wikipedia , lookup
VASCULAR SYSTEM VASOACTIVE DRUGS February 2017 THE VASCULAR SYSTEM Overview • Concerned with the pharmacology of blood vessels. • The walls of arteries, arterioles, venules and veins contain smooth muscle whose contractile state is controlled by circulating hormones and by mediators released locally from sympathetic nerve terminals (refer to Chemical Mediators & the Autonomic Nervous system) and endothelial cells. • These work mainly by regulating Ca2+ in vascular smooth muscle cells. (refer to How drugs act: cellular aspects-excitation, contraction and secretion) 2 Overview • This topic will consider the following: control of vascular smooth muscle by the endothelium and by the renin-angiotensin system, the actions of vasoconstrictor and vasodilator drugs Clinical uses of vasoactive drugs in some important diseases, namely:1. Hypertension (systemic and pulmonary) 2. Heart failure 3. Shock 4. Peripheral vascular disease 5. Raynaud’s disease NB: the use of vasoactive drugs to treat angina has been discussed (e.g. calcium antagonists) 3 Introduction • Need to understand and describe the structure and function of the vascular system • Actions of drugs on the vascular system can be broken down into effects on: 1. Total systemic (‘peripheral’) vascular resistance, one of the main determinants2+ of arterial blood pressure 2. The resistance of individual vascular beds, which determines the local distribution of blood flow to and within different organs; such effects are relevant to the drug treatment of angina, Raynauds phenomenon, pulmonary hypertension and circulatory shock. 3. Aortic compliance and pulse wave reflection, which are relevant to the treatment of cardiac failure and 4 angina Introduction • Actions of drugs on the vascular system can be broken down into effects on:….. 4. Venous tone and blood volume (the ‘fullness’ of the circulation), which together determine the central venous pressure and are relevant to the treatment of cardiac failure and angina; diuretics (which reduce blood volume) 5. Atheroma and thrombosis 6. New vessel formation (angiogenesis)important for example, in diabetic retinopathy and in treating malignant disease 5 Introduction… • Drug effects considered in this topic are caused by actions on vascular smooth muscle cells • Like other muscles, vascular smooth muscle contracts when cytoplasmic Ca2+ ([Ca2+]i) rises but the coupling between [Ca2+]i and contraction is less tight than striated or cardiac muscle. • Vasoconstrictors and vasodilators act by increasing or reducing [Ca2+]i and/or by altering the sensitivity of the contractile machinery to [Ca2+]i 6 Read on the following: • Vascular Structure and Function • Control of Vascular Smooth Muscle Tone -Two important physiological system regulate vascular tone, namely;1. The vascular endothelium 2. The renin-angiotensin system 7 VASOACTIVE DRUGS 8 Vasoactive Drugs • • • • Drugs can affect vascular smooth muscle by acting either directly on smooth muscle cells, or indirectly, for example on endothelial cells, on sympathetic nerve terminals or on the central nervous system (CNS) Mechanisms of directly acting vasoconstrictors and vasodilators are summarised in Figure 4.10 (p. 61 Rang & Dale’s 7th edition). Many indirectly acting drugs are discussed in other chapters. We concentrate here on agents that are not covered 9 elsewhere. Vasoactive Drugs… • 1. 2. 3. • 1. 2. Vasoconstrictor Drugs Angiotensin II Antidiuretic hormone Endothelin Vasodilator Drugs Directly acting vasodilators Vasodilators with unknown mechanism of action 3. Indirectly acting Vasodilator drugs 10 Vasoconstrictor Drugs • The α1-adrenoceptor agonists and drugs that release noradrenaline from sympathetic nerve terminals or inhibit its reuptake (sympathomimetic amines) cause vasoconstriction (refer to Noradrenergic transmission) • Some eicosanoids (e.g. thromboxane A2; and several peptides, notably endothelin, angiotensin and ADH, are also predominantly vasoconstrictor. • Sumatriptan and ergot alkaloids acting on certain 5-hydroxytryptamine receptors (5-HT2 and 5-HT1D) also cause vasoconstriction. 11 Vasoconstrictor Drugs.. • 1. 2. 3. Read on:Angiotensin II Antidiuretic hormone Endothelin 12 Vasodilator Drugs • Vasodilator drugs may play a major role in the treatment of common conditions including hypertension, cardiac failure and angina pectoris, as well as several less common but severe diseases including pulmonary hypertension and Raynaud’s disease. 13 Vasodilator Drugs 1. Direct acting Vasodilators • Targets on which drugs act to relax vascular smooth muscle include plasma membrane voltage-dependent calcium channels, sarcoplasmic reticulum channels (Ca2+ release or reuptake), and enzymes that determine Ca2+ sensitivity of the contractile proteins. • e.g. 1. Calcium antagonists 2. Drugs that activate potassium channels 3. Drugs that act via cyclic nucleotides 14 Vasodilator Drugs… 2. Vasodilators with unknown mechanism of action 1. Hydralazine • Hydralazine acts mainly on arteries and arterioles, causing a fall in blood pressure accompanied by reflex tachycardia and an increased cardiac output. • It interferes with the action of inositol trisphosphate on Ca2+ release from the sarcoplasmic reticulum. 15 Hydralazine… • Its original clinical use was in hypertension. • It is still used for short-term treatment of severe hypertension in pregnancy but can cause an immune disorder resembling systemic lupus erythematosus, so alternative agents are now usually preferred for long-term treatment of hypertension. • Recent evidence has, however, suggested that it has a place in treating heart failure in patients of African origin in combination with a long-acting organic nitrate. 16 Vasodilator Drugs… 2. Vasodilators with unknown mechanism of action… 2. Ethanol • Ethanol dilates cutaneous vessels, causing the familiar drunkard's flush. • Several general anaesthetics (e.g. propofol) cause vasodilatation as an unwanted effect . 17 Vasodilator Drugs… 3. Indirectly acting Vasodilator drugs • The two main groups of indirectly acting vasodilator drugs are inhibitors of: 1. sympathetic vasoconstriction 2. the renin-angiotensin-aldosterone system. NB: Read 18 CLINICAL USES OF VASOACTIVE DRUGS 19 Clinical Uses of Vasoactive Drugs • The conditions that can be treated by these drugs are: • systemic hypertension • cardiac failure • Shock • Peripheral vascular disease • Raynaud's disease • Pulmonary hypertension. 20 References Read • Rang & Dale’s Pharmacology-7th Edition Chapter 22. 21