* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Gut Tube and Digestion
Liver support systems wikipedia , lookup
Fecal incontinence wikipedia , lookup
Hepatocellular carcinoma wikipedia , lookup
Wilson's disease wikipedia , lookup
Hepatic encephalopathy wikipedia , lookup
Liver cancer wikipedia , lookup
Liver transplantation wikipedia , lookup
Cholangiocarcinoma wikipedia , lookup
Glycogen storage disease type I wikipedia , lookup
Surgical management of fecal incontinence wikipedia , lookup
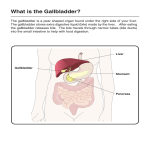
Gut Tube and Digestion Path of Food Esophagus Stomach Small intestines Large intestines Rectum and anus Liver and Pancreas Digestion function Role in glucose metabolism Path of Food Mouth--chewing Pharynx--conscious swallowing Esophagusu--transport to stomach Stomach--mechanical and chemical breakdown Small Intestines-chemical digestion and absorption Large Intestines-resorb water, form feces Rectum---collect and expel feces Esophagus Pharynx to stomach Smooth muscle (conscious swallowing is in pharynx) Passes through esophageal hiatus in diaphragm, stomach against inferior diaphragm Cardiac orifice, with esophageal hiatus guard opening to stomach, prevent regurgitation GERD--gastroesophageal reflux disease Sometimes due to hiatal hernia Lower esophagus becomes ulcerous and precancerous Treat with antacids and other acid-reducing drugs Stomach STRUCTURE J-shaped but varies from “steerhorn” (high and horizontal) to vertically elongate (down to pelvis on tall, thin people) From esophagus (cardiac orifice) to small intestine (pyloric sphincter) Greater, lesser curvatures FUNCTION Mechanical breakdown of food--smooth muscle in wall Protein breakdown--pepsin secreted by epithelial lining Acidic conditions--for pepsin to work and to kill bacteria Absorption of water, ions and some drugs (e.g., aspirin, alcohol) Digestive Tract (adult gut tube) Wall Internal = Mucosa Epithelium Lamina propria Muscularis mucosae Middle = Submucosa CT w/ elastic fibers, nerves, vessels Outer = Muscularis Externa Inner circular layer Outer longitudinal layer Internal Anatomy of Stomach Mucosa Rugae: mucosal folds allow expansion Typical Submucosa Muscularis externa Oblique layer Circular layer Pyloric sphincter Longitudinal layer Serosa pg 648 Small Intestines Duodenum C-shaped initial piece (5% of total) Entries for pancreatic, bile ducts Jejunum Fan-shaped coil (40% of total) at superior left abdomen Ileum Inferior right part of coil End of appendix at lower right quadrant Location of Duodenum Small Intestine: Modifications for absorption Length Increase surface area Plicae circularis Transverse ridges of mucosa Increase surface area Slow movement of chyme Villi Move chyme, increase contact Contain lacteals: remove fat Microvilli: Increase surface area Modifications decrease distally pg 653 Large Intestines Frame around rest of gut Ascending, transverse, descending Starts at cecum/appendix Ends at rectum, anal canal Teniae coli “ribbons” or strips of muscle along length of colon (three around tube) Tension in teniae coli forms haustra or sacs Little continuous movement, but mass peristaltic movement several times daily to force feces towards rectum Resorption of water from food Rectum + Anal Canal Rectum descends into pelvis no teniae coli longitudinal muscle layer complete rectal valves Anal Canal (more with pelvis) passes through levator ani muscle releases mucus to lubricate feces Internal anal sphincter involuntary, smooth m. External anal sphincter pg 655 voluntary, skeletal m. Blood supply--ventral branches off of aorta Celiac a.--to stomach, liver, pancreas, spleen, duodenum Superior (cranial mesenteric a.--to small intestines and most of colon Inferior (caudal) mesenteric a.--to descending colon, rectum Innervation of gut Parasympathetic What nerve? VAGUS With aorta Where does it run? Sympathetic Only thoracic output from spinal cord Splanchnic nerves from thorax lateral to vertebral bodies bring posteriorly to abdominal cavity and gut Synapse in celiac and superior mesenteric ganglia Both Para- and Sympathetic follow aa. out to organs High level of local control with network of synapses within ganglia and around gut Liver STRUCTURE Large ventral organ of abdominal cavity with multiple lobes (learn them!!) Sets against inferior surface of diaphragm on left side Forms as outpocketing of gut--common bile duct is left as connection Bile duct is two-way street (bile from hepatic duct is stored in gall bladder and later expelled to common bile duct to duodenum) FUNCTION Digestion--bile is digestive enzymes plus RBC breakdown product Removes nutrients and toxins from blood (hepatic portal system brings gut blood directly to liver) Glucose metabolism (with pancreas--see below) Gallbladder Muscular sac Between right + quadrate liver lobes Bile is stored + concentrated Bile: breaks down fats = emulsification Bile Produced by liver Stored in gallbladder pg 659 Bile Ducts Cystic duct carries bile from gallbladder Hepatic duct carries bile from liver Common Bile duct joins cystic and hepatic carries bile into duodenum pg 652 Movement of Bile pg 652 Bile secreted by liver continuously Hepatopancreatic (Vater) ampulla common bile + main pancreatic duct meet and enter duodenum Sphincter of Oddi around it closed when bile not needed for digestion Bile then backs up into gallbladder via cystic duct When needed gallbladder contracts, sphincters open Liver: External Features Diaphragmatic surface Right lobe (larger) Left lobe Falciform ligament between Fissure between Visceral surface Quadrate lobe Caudate lobe Both part of left lobe pg 659 Liver: Blood Supply Hepatic Vein from inferior vena cava Hepatic Artery from abdominal aorta Hepatic Portal Vein Carries nutrient-rich blood from stomach + intestines to liver Portal system = 2 capillary beds! pg 660 Hepatic Portal System--concept Fig. 19.22, M&M Directs blood that has already been through gut capillaries into liver capillaries (or sinusoids) Allows nutrients and toxins to be removed from blood Hepatic Portal System--anatomy Pancreas STRUCTURE Smaller, diffuse gland Head in C of duodenum Tail extends towards spleen FUNCTION Digestion--produces most digestive enzymes Glucose metabolism-Islets of Langerhans make insulin Glucose metabolism Liver receives blood from intestines (don’t forget hepatic portal system After meal, in response to insulin from pancreas, glucose stored as complex carbohydrate--glycogen--in liver Between meals, in response to glucagon from pancreas, glucose is released Pancreas releases insulin when sugar levels in blood go up Inadequate or zero insulin production results in hyperglycemia or high blood sugar Overproduction or over-dosing of insulin results in hypoglycemia or low blood sugar--insulin shock Diabetes is insufficient production of insulin Type I--juvenile onset with elimination of Islets of langerhans and zero insulin production Type II--adult onset with gradual loss of insulin production “How Stuff Works” Diabetes: http://www.howstu ffworks.com/diabet es1.htm