* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download MODELING THE DYNAMICS OF THYROID HORMONES AND
Survey
Document related concepts
Hormone replacement therapy (male-to-female) wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Hypopituitarism wikipedia , lookup
Hypothalamus wikipedia , lookup
Transcript
MODELING THE DYNAMICS OF THYROID HORMONES AND RELATED
DISORDERS
by
Oylum Şeker
B.S., Industrial Engineering, Boğaziçi University, 2009
Submitted to the Institute for Graduate Studies in
Science and Engineering in partial fulfillment of
the requirements for the degree of
Master of Science
Graduate Program in Industrial Engineering
Boğaziçi University
2012
ii
MODELING THE DYNAMICS OF THYROID HORMONES AND RELATED
DISORDERS
APPROVED BY:
Prof. Yaman Barlas
...................
(Thesis Supervisor)
Assist. Prof. Gönenç Yücel
...................
Assoc. Prof. Ata Akın
...................
DATE OF APPROVAL: 17.09.2012
iii
ACKNOWLEDGEMENTS
First and foremost, I would like to express my sincere and immense gratitude to Prof.
Yaman Barlas, my thesis supervisor, for his guidance, patience and support throughout this
study. Anything that I could have humbly learnt and hopefully continue to learn from him
as an excellent professor, as an intellectual, and as a friend have been and will be
invaluable assets to me.
I would like to thank to Assist. Prof. Gönenç Yücel and Assoc. Prof. Ata Akın for
taking part in my thesis committee and providing valuable comments, which I surely will
benefit in my future research.
I wish to extend my sincere thanks and appreciation to Prof. Faruk Alagöl for readily
offering his vast knowledge and experience about thyroid, and for his deep interest in this
study.
I am grateful to Nükhet Barlas, who inspired the onset of this work, for kindly
sharing her personal blood test results to support this study.
I would like to express my gratitude to Prof. Çetin Önsel for being so kind to answer
my exhaustive questions about thyroid.
I wish to express special acknowledgements to my colleagues at SESDYN
Laboratory. I would like to thank to Nisa Önsel for her sympathetic, soothing and warm
companion, to Onur Özgün for kindly offering his never-ending help and support on all the
otherwise unsolvable methodological and technological issues, to M. Emre Keskin for
genially answering my endless questions about every single topic in industrial engineering
courses, and finally to Can Sücüllü for cheering us up with his improvised shows.
iv
I owe my special thanks to O. Kaan Drağan for his irreplaceable friendship and
sympathy, and for patiently being my one and only voluntary therapist.
Lastly, I wish to thank to Google and to some undisclosed third parties which
generously provided me numerous papers and books about the subject of my study.
v
ABSTRACT
MODELING THE DYNAMICS OF THYROID HORMONES AND
RELATED DISORDERS
In this study, a dynamic simulation model for thyroid hormone system is constructed.
The objective of this work is to first generate the dynamics of the hormones involved in
thyroid hormone system in healthy body, and then to adapt the model to portray the
dynamics of certain common thyroid disorders. The ultimate aim is to provide a platform
for scenario analysis to support medical education, training and research, without risking
patients’ health. Initially, the model structure is tested by standard structure validity tests.
After the validation part, four common thyroid disorders are simulated. Firstly, Graves’
disease, the most common source of hyperthyroidism, is addressed. Goiter formation,
effect of iodine availability on the severity of the disease, and increased T3/T4 –a
commonly used diagnostic measure in hyperthyroidism– are all well captured by the
model. Other typical behaviour of hormones and glands are also well mimicked by
simulations. Secondly, iodine deficiency, one prevailing cause of hypothyroidism, is
discussed for two different levels of daily iodine intake. The model was able to depict all
the characteristic changes including the goiter formation and increase in T3/T4 in these
two scenarios, both independently and comparatively. Thirdly, the transient inhibitory
effect of excessive iodine intake on thyroid gland is discussed. The model is able to
demonstrate the enlargement in thyroid volume and the mild decline in thyroid hormones.
Lastly, a condition called subacute thyroiditis, a common disorder in which thyroid gland
is exposed to inflammation, is analysed. The typical triphasic clinical course of subacute
thyroiditis, comprised of thyrotoxicosis, hypothyroidism and normal thyroid functioning is
well represented by the model. In conclusion, with respect to both qualitative and
quantitative information in literature, and interviews with the medical doctors, the model
exhibits an acceptable degree of validity and is able to cover a wide range of thyroidrelated disorders.
vi
ÖZET
TİROİT HORMONLARININ VE İLGİLİ HASTALIKLARIN
DİNAMİKLERİNİN MODELLENMESİ
Bu çalışmada, tiroit hormon sistemi için dinamik bir benzetim modeli kurulmuştur.
Çalışmanın amacı, öncelikle sağlıklı vücutta tiroit hormon sisteminin işleyişinde rol alan
hormonların dinamiğini üretmek ve ardından yaygın görülen bazı tiroid rahatsızlıklarının
dinamiklerinin gösterilebilmesi için modeli uyarlamaktır. Nihai amaç, hastaların hayatını
tehlikeye atmaksızın tıbbi eğitim, çalışma ve araştırmayı senaryo analizleriyle
destekleyecek bir ortam sunmaktır. Öncelikle, modelin yapısı standart geçerlilik testleri ile
analiz edilmiştir. Geçerleme safhası bittikten sonra, yaygın görülen dört tane tiroid
hastalığının benzetimi yapılmıştır. İlk olarak, hipertiroidizmin sık görülen sebeplerinden
biri olan Graves’ hastalığı ele alınmıştır. Model, guatr oluşumunu, mevcut iyot miktarının
hastalığın şiddetine etkisini, bu hastalığın teşhisinde sıklıkla kullanılan artmış T3/T4
oranını ve diğer hormon ve bezlerin tipik davranışlarını tutarlı bir biçimde
sergileyebilmiştir. İkinci olarak, hipotiroidizmin sıkça görülen sebeplerinden biri olan iyot
eksikliği iki farklı günlük iyot alımı seviyesi için incelenmiştir. İki iyot alım seviyesinde
guatr oluşumu ve T3/T4 oranındaki değişimler gibi tipik göstergeler hem karşılaştırmalı
hem de bağımsız olarak model tarafından üretilebilmiştir. Üçüncü olarak, aşırı iyot
alımının geçici kısıtlayıcı etkileri ele alınmış, tiroit hacmindeki büyüme ve tiroit
hormonlarındaki hafif düşüş elde edilebilmiştir. Son olarak, tiroit bezinin iltihaplanması
sonucu ortaya çıkan subakut tiroidit adlı hastalık analiz edilmiştir. Model, hastalığın
tirotoksikoz, hipotiroidizm ve ardından normal işleyişin kazanılmasından oluşan üç
aşamalı tipik klinik gidişatını başarılı bir biçimde yansıtabilmiştir. Sonuç olarak, literatürde
yer alan nitel ve nicel bilgiler ile tıp doktorlarlarıyla yapılan görüşmelerin ışığında,
modelin makul seviyede geçerli olduğu ve geniş yelpazedeki tiroit hormon hastalıklarını
kapsayabildiği söylenebilir.
vii
TABLE OF CONTENTS
ACKNOWLEDGEMENTS .................................................................................................. iii
ABSTRACT........................................................................................................................... v
ÖZET .................................................................................................................................... vi
LIST OF FIGURES .............................................................................................................. ix
LIST OF ACRONYMS/ABBREVIATIONS ....................................................................... ix
1. INTRODUCTION ............................................................................................................. 1
2. LITERATURE REVIEW AND RESEARCH OBJECTIVE ............................................ 4
3. RESEARCH METHODOLOGY ...................................................................................... 7
4. OVERVIEW OF THE MODEL ...................................................................................... 10
5. DESCRIPTION OF THE MODEL ................................................................................. 13
5.1. Hypothalamus Sector ............................................................................................... 13
5.1.1. Background Information ................................................................................ 13
5.1.2. Fundamental Approach and Assumptions ..................................................... 15
5.1.3. Description of the Structure ........................................................................... 18
5.2. Pituitary Sector ......................................................................................................... 25
5.2.1. Background Information ................................................................................ 25
5.2.2. Fundamental Approach and Assumptions ..................................................... 27
5.2.3. Description of the Structure ........................................................................... 27
5.3. Thyroid Sector .......................................................................................................... 31
5.3.1. Background Information ................................................................................ 31
5.3.2. Fundamental Approach and Assumptions ..................................................... 34
5.3.3. Description of the Structure ........................................................................... 35
5.4. Iodine Sector ............................................................................................................ 52
5.4.1. Background Information ................................................................................ 52
5.4.2. Description of the Structure ........................................................................... 53
6. VALIDATION AND ANALYSIS OF THE MODEL .................................................... 58
6.1. Equilibrium Behaviour ............................................................................................. 59
viii
6.2. Base Run .................................................................................................................. 59
6.3. TRH Injection Test ................................................................................................... 61
6.4. Ten-Fold Increase in T4 Secretion for One Hour .................................................... 62
6.5. Zero T4 Secretion for One Hour .............................................................................. 65
6.6. Hypophysectomy ..................................................................................................... 67
7. THYROID DISORDERS ................................................................................................ 70
7.1. Graves’ Disease ........................................................................................................ 70
7.1.1. Graves’ Disease with Normal Daily Iodine Intake ........................................ 71
7.1.2. Graves’ Disease with Relatively High Daily Iodine Intake ........................... 76
7.2. Iodine Deficiency ..................................................................................................... 79
7.2.1. Severe Iodine Deficiency ............................................................................... 80
7.2.2. Moderate Iodine Deficiency........................................................................... 86
7.3. Iodine Excess ........................................................................................................... 89
7.4. Subacute Thyroiditis ................................................................................................ 95
8. CONCLUSION .............................................................................................................. 103
APPENDIX: Model Equations .......................................................................................... 105
REFERENCES .................................................................................................................. 118
ix
LIST OF FIGURES
Figure 1.1.
Basic structure of the thyroid hormone system. ............................................. 2
Figure 3.1.
Stock-flow diagram of a simple population model. ....................................... 9
Figure 4.1.
Simplified causal loop diagram of the model. .............................................. 11
Figure 5.1.
Stock-flow diagram of the hypothalamus sector. ......................................... 19
Figure 5.2.
Effect of thyroid hormones on TRH secretion. ............................................ 20
Figure 5.3.
Graphical function for the effect of capacity on TRH secretion. ................. 22
Figure 5.4.
Graphical function for the effect of implied TRH secretion on hypothalamus
weight........................................................................................................... 23
Figure 5.5.
Graphical function for effect on hypothalamic adjustment time. ................. 25
Figure 5.6.
Stock-flow diagram of the pituitary sector. .................................................. 28
Figure 5.7.
Graphical function for the effect of TRH on TSH secretion. ....................... 30
Figure 5.8.
Graphical function for the effect of thyroid hormones on TSH secretion. ... 30
Figure 5.9.
Stock-flow diagram of the thyroid sector. .................................................... 36
Figure 5.10.
Graphical function for the effect of thyroid hormone store capacity. .......... 38
Figure 5.11. The graphical function for the effect of TSH on thyroid hormone secretion.
..................................................................................................................... 39
Figure 5.12.
Graphical function for the effect of iodine on thyroid capacity. .................. 40
Figure 5.13.
Graphical function for the effect of preferential T3 synthesis on reduction in
T3 synthesis. ................................................................................................ 47
Figure 5.14. Graphical function for the effect of T3 concentration on peripheral
conversion. ................................................................................................... 49
Figure 5.15. Graphical function for the effect of thyroid stimulation on T3 secretion
fraction. ........................................................................................................ 51
Figure 5.16.
Graphical function for the fraction of T3 secretion. .................................... 52
Figure 5.17.
Stock-flow diagram of the iodine sector. .................................................... 54
Figure 5.18.
Graphical function for desired trapping fraction. ........................................ 55
Figure 5.19.
Graphical function for the effect of TSH on iodide trapping. ..................... 56
x
Figure 5.20.
Graphical function for the effect of thyroid weight on iodide trapping. ..... 56
Figure 5.21.
Simplified stock-flow diagram of the model. .............................................. 57
Figure 6.1.
T3 (left top), T4 (right top), TRH (lower left), and TSH (lower right)
concentrations at equilibrium....................................................................... 59
Figure 6.2.
T4 concentration in base run. ....................................................................... 60
Figure 6.3.
T3 concentration in base run. ....................................................................... 60
Figure 6.4.
TSH concentration in base run. .................................................................... 60
Figure 6.5.
TRH concentration in base run. .................................................................... 61
Figure 6.6.
Average TSH concentration of six normal subjects when 25 µg TRH is
injected at t=0 (Snyder and Utiger, 1972).................................................... 62
Figure 6.7.
TSH concentration when 25 µg TRH is injected at t=0. .............................. 62
Figure 6.8.
T4 concentration when its secretion is increased ten-fold for one hour. ...... 63
Figure 6.9.
T3 concentration when T4 secretion is increased ten-fold for one hour. ..... 63
Figure 6.10.
TRH concentration when T4 secretion is increased ten-fold for one hour. . 64
Figure 6.11.
TSH concentration when T4 secretion is increased ten-fold for one hour. .. 64
Figure 6.12.
T4 concentration when T4 secretion is stopped for one hour. ..................... 65
Figure 6.13.
T3 concentration when T4 secretion is stopped for one hour. ..................... 66
Figure 6.14.
TSH concentration when T4 secretion is stopped for one hour. .................. 66
Figure 6.15.
T3 concentration in case of hypophysectomy. ............................................. 67
Figure 6.16.
TRH concentration in case of hypophysectomy. .......................................... 67
Figure 6.17.
Thyroid weight in case of hypophysectomy. ................................................ 68
Figure 6.18.
Hypothalamus weight in case of hypophysectomy. ..................................... 69
Figure 7.1.
T3 concentration in Graves’ disease with normal iodine intake. ................. 71
Figure 7.2.
T4 concentration in Graves’ disease with normal iodine intake. ................. 72
Figure 7.3.
Iodine in thyroid in Graves’ disease with normal iodine intake. .................. 73
Figure 7.4.
T3 to T4 ratio in Graves’ disease with normal iodine intake. ...................... 73
Figure 7.5.
TRH concentration in Graves’ disease with normal iodine intake. .............. 74
Figure 7.6.
TSH concentration in Graves’ disease with normal iodine intake. .............. 74
Figure 7.7.
Thyroid weight in Graves’ disease with normal iodine intake. .................... 75
Figure 7.8.
Hypothalamus weight in Graves’ disease with normal iodine intake. ......... 75
xi
Figure 7.9.
Pituitary weight in Graves' disease with normal iodine intake. .................. 76
Figure 7.10.
T3 concentration in Graves’ disease with relatively high iodine intake. .... 77
Figure 7.11.
Iodine in thyroid in Graves’ disease with relatively high iodine intake. ..... 77
Figure 7.12.
T3 to T4 ratio in Graves’ disease with relatively high iodine intake. ......... 78
Figure 7.13.
TSH concentration in Graves’ disease with relatively high iodine intake. . 78
Figure 7.14.
Thyroid weight in Graves’ disease with relatively high iodine intake. ....... 79
Figure 7.15.
Pituitary weight in Graves’ disease with relatively high iodine intake. ...... 79
Figure 7.16.
T3 concentration when daily iodine intake is 30 µg. .................................. 81
Figure 7.17.
T4 concentration when daily iodine intake is 30 µg. .................................. 81
Figure 7.18.
T3 to T4 ratio when daily iodine intake is 30 µg. ....................................... 82
Figure 7.19.
Iodine in thyroid when daily iodine intake is 30 µg. ................................... 82
Figure 7.20.
T3 store when daily iodine intake is 30 µg. ................................................ 83
Figure 7.21.
T4 store when daily iodine intake is 30 µg. ................................................ 83
Figure 7.22.
TSH concentration when daily iodine intake is 30 µg. ............................... 84
Figure 7.23.
Thyroid weight when daily iodine intake is 30 µg. ..................................... 84
Figure 7.24.
Hypothalamus weight when daily iodine intake is 30 µg. .......................... 85
Figure 7.25.
Pituitary weight when daily iodine intake is 30 µg. .................................... 85
Figure 7.26.
T3 concentration when daily iodine intake is 50 µg. .................................. 86
Figure 7.27.
T4 concentration when daily iodine intake is 50 µg. .................................. 86
Figure 7.28.
T3 to T4 ratio when daily iodine intake is 50 µg. ....................................... 87
Figure 7.29.
T3 store when daily iodine intake is 50 µg. ................................................ 88
Figure 7.30.
TSH concentration when daily iodine intake is 50 µg. ............................... 88
Figure 7.31.
Thyroid weight when daily iodine intake is 50 µg. ..................................... 89
Figure 7.32.
Average free T4 concentration of ten subjects receiving 27 mg iodine
supplementation for 28 days (Namba et al., 1993). ..................................... 90
Figure 7.33. Free T4 concentration (in pmol/l) in case of 27 mg iodine supplementation
for 28 days. .................................................................................................. 91
Figure 7.34.
T3 concentration in case of 27 mg iodine supplementation for 28 days. ..... 91
Figure 7.35. Average TSH concentration of ten subjects receiving 27 mg iodine
supplementation for 28 days (Namba et al., 1993). ..................................... 92
xii
Figure 7.36.
TSH concentration in case of 27 mg iodine supplementation for 28 days. .. 92
Figure 7.37. Average thyroid volume (as % of normal volume) of ten subjects receiving
27 mg iodine supplementation for 28 days (Namba et al., 1993). ............... 93
Figure 7.38.
Thyroid weight in case of 27 mg iodine supplementation for 28 days. ....... 94
Figure 7.39. Average serum iodine levels of ten subjects receiving 27 mg iodine
supplementation for 28 days (Namba et al., 1993). ..................................... 94
Figure 7.40.
Iodine in blood in case of 27 mg iodine supplementation for 28 days. ........ 95
Figure 7.41.
Modified structure of thyroid sector for subacute thyroiditis....................... 97
Figure 7.42.
Modified structure of iodine sector for subacute thyroiditis. ....................... 98
Figure 7.43.
The assumed course of inflammation status in subacute thyroiditis. ......... 100
Figure 7.44.
TSH and T4 concentrations in subacute thyroiditis. .................................. 100
Figure 7.45.
Data from a patient with subacute thyroiditis (Lazarus, 2009). ................. 101
Figure 7.46.
Data from a patient with subacute thyroiditis (secondary axis: TSH). ...... 101
Figure 7.47.
T3 to T4 ratio in subacute thyroiditis. ........................................................ 102
xiii
LIST OF ACRONYMS/ABBREVIATIONS
abs
absorption
adj
adjustment
avail
availability
cap
capacity
chg
change
clear
clearance
conc
concentration
cons
consumption
conv
conversion
deiod
deiodination
del
delay
des
desired
disc
discrepancy
eff
effect
excr
excretion
fr
fraction
gr
graphical function
hypo
hypothalamus (or hypothalamic)
imp
implied
peri
peripheral
pit
pituitary
pos
possible
pot
potential
pref
preferential
prod
productivity
recov
recovery
red
reduction
xiv
rest
restricted
restor
restoration
stim
stimulation
thres
threshold
thy
thyroid (or thyroidal)
trap
trapping
wt
weight
AT
Adjustment Time
HAT
Adjustment Time for Hypothalamus
PAT
Adjustment Time for Pituitary
TAT
Adjustment Time for Thyroid
TH
Thyroid Hormones
TRH
Thyrotropin Releasing Hormone
TSH
Thyroid Stimulating Hormone
1
1. INTRODUCTION
There are mainly two systems in the regulation of the functions of the body: (1) the
nervous system, and (2) the endocrine system, or the hormonal system. In this study, a
hormonal system will be of interest. For the lexical meaning, the word “hormone” is
derived from the Greek word hormaein, which means to excite, arouse or stir up. As for
the biological implication, a hormone is a chemical substance responsible for conveying
messages to target cells. They are secreted by a cell or gland, and act as means of
communication among the parts of the body. Through the actions of hormones, the
endocrine system exerts physiological control on metabolic functions of the body.
Therefore, endocrine system plays a vital role in the regulation, integration and
coordination of various physiological processes (Rhoades and Bell, 2009).
A crucial point in the functioning of endocrine system is to preserve the internal
balance, or homeostasis, in the body. This is where feedback loops come into play.
Feedback loops are the principal regulators of the endocrine system. They adjust the
amount of hormones released by the gland and keep them at a desired level in order to
guarantee a healthy maintenance of bodily functions.
As far as the order of feedback loops is concerned, different forms of hormonal
regulation exist. Rather than the systems that operate under the control of a single feedback
loop, the ones involving higher order, complex feedback loops have more interesting
dynamics to study. Production and release of thyroid hormones, which comprises the main
focus in this study, is controlled by such higher order negative (balancing, compensating)
feedback loops.
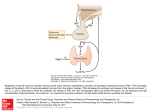
Three tiers are involved in thyroid hormone system. First tier is the hypothalamus,
second is the pituitary gland, and the third one is the thyroid gland (Kronenberg et al.,
2008). Firstly, the hypothalamus secretes thyrotropin-releasing hormone (TRH) which
2
prompts the production of thyroid-stimulating hormone (TSH) from the pituitary. Then,
TSH stimulates the thyroid gland. Upon stimulation, production and release of thyroid
hormones, which are triiodothyronine (T3) and thyroxine (T4), is triggered. After T3 and
T4 are secreted from the thyroid, they circulate in blood and reach their target tissues
(Guyton and Hall, 2006; Kronenberg et al., 2008; Rhoades and Bell, 2009). Eventually,
concentration of thyroid hormones in blood creates a double-armed negative feedback
effect. That is, thyroid hormones in blood affect negatively both the hypothalamus and the
pituitary, and consequently control the secretion of TRH and TSH to keep the thyroid
hormone concentrations at a constant desired level. Pictorially, the basic structure of the
thyroid hormone system looks as in Figure 1.1.
-
Hypothalamus
TIER I
TRH
-
Pituitary
TIER II
TSH
Thyroid
TIER III
T3 and T4
Peripheral Tissues
Figure 1.1. Basic structure of the thyroid hormone system.
The thyroid hormones play key roles in the regulation of bodily functions. They
govern the pace of metabolic functions of cells in the body by enhancing the rate of oxygen
consumption, utilization of fats, carbohydrates and proteins by the cells. In this respect, the
thyroid gland undertakes a managerial role in the regulation of metabolic functions;
3
depending on the intensity of hormone signals from the thyroid, the rate of metabolism in
the body is adjusted.
The prevalence of thyroid diseases is quite high and misdiagnosis of these diseases is
not uncommon. Since these hormones affect virtually every part of the body and regulate
some vital functions, it is important to gain an insight into the structure of this hormonal
system, the interplay between the constituent components of the system, and the dynamics
of the hormones involved under related disorders.
In the following chapter, systems-theoretic research in the modelling of thyroid
hormone system will be briefly reviewed and the research objective of this modelling study
will be described. Then, the research methodology and the rationale behind it will be
concisely explained. In the remaining chapters, the system dynamics model will be
elucidated, validity test results will be presented, and the dynamics of some well-known
disorders of thyroid hormone system will be generated and discussed.
4
2. LITERATURE REVIEW AND RESEARCH OBJECTIVE
Modelling of physiological systems has aroused considerable interest over the past
several decades. That physiological systems, in particular endocrine systems, are capable
of preserving their internal balance through the actions of feedback mechanisms connects
them to technological feedback control systems that are widely studied in engineering
fields, in the sense that their regulation abides essentially to the same principles. The
formidable complexity and large number of interactions inherent within and among
endocrine systems introduce problems of quantification that well fit to the tremendous
abilities of computers, and that (verbal) language mostly fails to suffice, whereas
modelling and simulation succeeds for both simple and complex systems, as pointed in one
of the early works of DiStefano and Chang (1971) on simulation of thyroid hormone
dynamics.
A number of studies have been conducted in which engineering principles are
applied to model the thyroid hormone system at various levels of complexity, from various
aspects, and with different research objectives. One prominent name in these studies is
Joseph J. DiStefano III. There has been a number of pioneering researches conducted by
DiStefano and colleagues to model the thyroid system with a systems-theoretical approach
and integrate it with experimental data. Some of these studies deal with hypotheses about
the underlying feedback structure (DiStefano, 1969; DiStefano and Stear, 1968), some with
parameter estimation for thyroid hormone secretion, distribution, binding, conversion and
metabolism (DiStefano and Chang, 1971; DiStefano and Mori, 1969; Wilson et al., 1977),
some with the mathematical models for secretory output of thyroid hormones in response
to TSH input (DiStefano, 1969), and some with the prescription of thyroid hormones in
hypothyroidism and after thyroidectomy (Mak and DiStefano, 1977; Eisenberg et al.,
2007; Ben-Shachar et al., 2012).
5
There are also other thyroid-related quantitative modelling studies that adopt a
systemic perspective. In the work of Khee and Leow (2007), a mathematical model is
proposed for pituitary-thyroid interaction that aims to provide a better understanding of the
sensitivity of the pituitary to the feedback effect of thyroid hormones in the context of
thyroid hormone excess and deficiency. Another work conducted by Liu et al. (1994)
proposes a new mathematical model for the secretory system of hypothalamo-pituitarythyroid axis by revising and improving the previous two works by Liu and Peng (1990)
and Liu and Liu (1992) which takes into account the interactions of the hormones in the
axis and the binding characteristics of hormones to proteins in plasma and tissues. Lastly,
the work of Degon et al. (2008) uses recent molecular-level and clinical observations to
develop a computational thyroid model which captures the known aspects of thyroid
physiology and uses it to evaluate the competing hypotheses related to the Wolff-Chaikoff
escape.
Unlike many others, our modelling study integrates all four aspects involved in the
control of thyroid hormone system; namely the hypothalamus, pituitary, thyroid, and the
essential ingredient iodine. The main focus is to depict the major macro-level causal
relationships among these four components that strive for the homeostatic regulation of the
system, rather than concentrating on the intracellular pathways and micro-level molecular
mechanisms. The model combines sufficiently many aspects involved in the regulation of
thyroid hormone system, and thus is able to cover a wide range of conditions (like
hyperthyroidism, hypothyroidism, thyroiditis, goiter, etc.) and illustrate the associated
overall descriptive behaviours of key variables in the system.
The main goal of modelling physiological systems is to provide a platform to
conduct experiments and subsequently propose policies, without any necessity to rehearse
on humans. This study aims at modelling the thyroid system to capture the dynamics of
thyroid hormones and some related diseases in order to facilitate the recognition of these
disorders. Initial goal is to develop a system dynamics model as a valid representation of
the underlying structure of thyroid hormone system so as to illustrate the dynamics of key
stimulating and thyroid hormones in healthy body. The next purpose is to modify the
6
model to represent some well-known thyroid disorders. The final goal is to capture the
typical course of behaviour of the key hormones under these disorders, hence to hopefully
offer a platform for the recognition of these disorders and for scenario analysis to assist
medical education, training and research.
7
3. RESEARCH METHODOLOGY
This study aims at modelling the thyroid hormone system to portray the dynamics of
key hormones under healthy and diseased states, particularly by stressing the role of
functional feedback mechanisms involved. Being composed of a tripartite regulatory
mechanism, the smooth functioning of thyroid hormone system can be disturbed by the
malfunctioning of any of the constituent subsystems, either due to purely internal motives,
or anomaly of essential external inputs to the system. The fact that thyroid hormone system
operates under not a simple first order but a dual feedback control, the existence of two
different thyroid hormones, one of them largely depending on the production of the other
and requiring a more sensitive modulation, and the role of iodine intake render the problem
complex enough that our intuition mostly remains incapable. The assistance of
mathematical or simulation modelling may well provide a deep insight into the structure of
the system and the behaviour of key variables under related disorders, and contribute to
medical training and research.
System dynamics methodology is an efficient tool to enhance the understanding of
the behaviour of complex, large-scale systems and study their underlying structures. The
idea is to address an issue by adopting a holistic approach, which essentially states that a
system is more than the sum of its individual constituent parts and cannot be fully
understood in terms of the properties of individual elements in isolation. So, this approach
puts a particular emphasis to the causal relationships between the constituents of the
system. In other words, it is the internal structure of a system which drives the system
behaviour. The structure can be defined as the totality of relationships that exist between
system variables and the behaviour of a system is essentially the operation of its internal
structure over time (Barlas, 2002). Once a proper and valid model structure is constructed,
the behaviour that the system would generate under various schemes can be experimented
via simulation runs, and a broad appreciation can be developed about the system as a
whole.
8
The fact that feedback relationships largely prevail in the regulation of endocrine
systems makes this engineering discipline a natural choice in such modelling studies. As
far as the dominant roles of accumulations, feedbacks, nonlinearities and time delays
inherent in the system of interest are concerned, system dynamics methodology is very
suitable for quantitative behavioural analysis of the disorders of thyroid system.
One important feature of system dynamics approach is that it particularly emphasizes
the importance of causal relations as opposed to mere statistical correlations (Barlas,
2002). It aims at developing an understanding of the overall dynamic behaviour of the
system of concern, rather than concentrating on the point prediction of the future values of
the variables involved. In this respect, it becomes an appropriate tool in the modelling of
physiological systems, for it is usually the collection of the overall pattern of the key
variables, rather than their precise point values, which characterizes a particular condition.
In system dynamics methodology, two central concepts are used in modelling. The
first one is stocks, which represent the accumulations in a system. Stocks can be used in
the conceptualization of a wide range of notions, from physical to information entities.
Some examples for stock variables can be inventory, population, knowledge level, etc. The
stocks are changed merely via their flows; that is, the net flow into a stock corresponds to
the rate of change of that stock. Examples of flow variables related to the above stock
examples can be production, sales, births, deaths, learning, forgetting, etc. (Barlas, 2002).
A stock variable and its flows together correspond to a first order differential (or
difference) equation, the stock being the system variable and the flows being the rates of
change over time.
The mathematical description of a system only entails the stocks and flows actually.
However, for the sake of clarity, a third type of variable is also used in system dynamics
which is called converter, or auxiliary variable. Converters are used to explicitly define
some intermediate parameters or variables, and thus can be constants or functions of stocks
and/or flows.
9
In model diagrams, stocks are represented by rectangular boxes, and flows by valves
on arrows that point into or out of the stock. If the arrowhead of the flow point into the
stock, that flow is called an “inflow”, and if it points out, then it is named “outflow”.
Clouds symbolize the sources and sinks for the flows if they originate from or discharge
outside the boundary of the model, and they do not induce any capacity constraint on the
related flow (Sterman, 2000). An example stock-flow diagram of a simple population
model is shown in Figure 3.1.
death fraction
birth fraction
Population
birth rate
death rate
Figure 3.1. Stock-flow diagram of a simple population model.
Population(t) = Population(t - dt) + (birth rate – death rate) × dt
(3.1)
birth rate = birth fraction × Population
(3.2)
death rate = death fraction × Population
(3.3)
In this simple model, the stock variable is Population. The inflow to the stock is birth
rate and the outflow death rate; that is, the birth rate tends to increase and death rate tends
to decrease the population from its present value. birth fraction and death fraction are
auxiliary variables. The arrows that connect the variables show the causal relationships
between the variables. The variable on the head of the arrow is defined as a function of the
variable (or the parameter) on the tail of the arrow.
10
4. OVERVIEW OF THE MODEL
The levels of all the hormones in thyroid hormone system are controlled by the
properly operating feedback loops between the components of the system as it is the case
in most other physiological systems to preserve a stable functioning. In thyroid hormone
system, two fundamental feedback loops operate on hypothalamus-pituitary-thyroid and
pituitary-thyroid axes. Both of these loops operate to keep the thyroid hormones T3 and T4
at their normal levels.
The overall model basically consists of four subdivisions: the hypothalamus, the
pituitary, the thyroid, and the iodine. Hypothalamus and pituitary sectors are basically the
same in terms of their qualitative structure; they involve one gland, its related hormone,
and relationships that have an effect on the gland and hormone. Thyroid sector, however,
involves one gland, related two hormones, the stores of the two hormones, and all the
means and links that affect the functioning of the sector. Lastly, the iodine sector, where
iodine is the main rate-limiting ingredient in the synthesis of thyroid hormones, involves
the iodine levels in blood and in the thyroid gland, and the relevant measures.
A simplified causal loop diagram depicting the main variables in the model together
with the key feedback loops is provided in Figure 4.1. A “+” sign on the head of an arrow
indicates a positive causal relationship between the variable on the tail and the variable on
the head of the arrow, and conversely a “−” sign a negative causality. A positive causal
link means that a change in the variable on the tail of the arrow (cause) induces a change in
the variable on the head of the arrow (effect) in the same direction by an amount more than
what it would have been otherwise. Conversely, a negative causal link means that a change
in the cause prompts a change in the variable on the head of the arrow in the opposite
direction by an amount more than what it would have been otherwise.
11
-
Implied TRH
secretion
+
Desired
hypothalamus
weight
Free T3 and T4 in
Blood
+
+
TRH secretion
+
+
Hypothalamus
Weight
+
TRH
1
3
T3 and T4
+
- Implied TSH
secretion
+
5
+
Thyroid
Weight
+
+
Desired
thyroid
weight
T3 and T4
secretion
TSH secretion
+
2
+
Pituitary
Weight
+
+
+
Desired
pituitary
weight
Implied T3 and T4
secretion
4
+
+
TSH
Figure 4.1. Simplified causal loop diagram of the model.
The 1st and 2nd loops demonstrate the negative feedback mechanism on
hypothalamus-pituitary-thyroid axis and pituitary-thyroid axis respectively. The hormones
involved in these loops are TRH, TSH and T3 and T4. These two main feedback loops
represent the short-term hormone control mechanisms in the body. In addition to the shortterm effects, some delayed effects on the weights of hypothalamus, pituitary and thyroid
gland may be observed. The 3rd, 4th and 5th loops display these delayed feedback effects
12
between the weight of one particular gland and the subsequent hormone secretions in the
related axis.
The model will be elucidated in detail in the next chapter; but, briefly the rationale
behind the model is as follows: The amount of a hormone secreted basically depends on
two factors; the capacity of the gland and the implied secretion rate. The capacity of the
gland is mainly imposed by the weight of the gland. The implied secretion rate is
determined by the relative amounts of stimulating hormone and inhibitory hormone, if any,
and this happens without a delay. However, changes in gland weight take place in time.
First, the body “decides” on a desired gland weight with a delay by continually considering
the induced levels of hormone demand, which actually is the implied secretion rate of that
gland. According to this target level, gland weight might be altered in the long run.
13
5. DESCRIPTION OF THE MODEL
5.1. Hypothalamus Sector
5.1.1. Background Information
Hypothalamus, a key regulator of homeostasis, is a small region of the brain located
above the brain stem. It is the central element in the regulation of endocrine function due to
its connections with the pituitary gland, which is the master gland of the endocrine system
(Rhoades and Bell, 2009). The hypothalamus synthesizes and secretes unique releasing and
inhibitory hormones which coordinate the production and secretion of hormones from
anterior pituitary, which is one of the two lobes of the pituitary gland (Melmed, 2002). The
weight of the hypothalamus in adult human is about 4000 mg (Bhagavan, 2002). The
hypothalamus secretes various hormones that affect the anterior pituitary hormones, one of
them being the TRH. TRH is synthesized and secreted by the parvicellular neurons of the
paraventricular cells (PVNparv) and the periventricular nucleus (PeriVN).
TRH is a hypothalamic hormone which principally stimulates the synthesis and
release of TSH. The connection between the hormones of the hypothalamus and the
anterior pituitary is enabled via minute blood vessels called hypothalamic-hypophysial
portal vessels. Through these portal vessels, TRH is transported to the anterior pituitary to
trigger the secretion of TSH. The rate of TRH secretion is mainly determined by the level
of free thyroid hormone levels in blood. Some portion of free T3 and T4 molecules
impinges upon hypothalamic cells and couples with the receptors on these cells (Bhagavan,
2002; Rhoades and Bell, 2009; Guyton and Hall, 2006; Werner et al., 2005). The amount
of thyroid hormone-receptor complexes is the main determinant of the rate of TRH
secretion. As aforementioned, the levels of thyroid hormones in blood negatively affect
TRH secretion. So, as the amount of thyroid hormone-receptor complexes increase on the
14
cells of the hypothalamus, the TRH output will decrease, and vice versa. In short, the rate
of TRH secretion is inversely proportional to the amount of thyroid hormones in blood.
There are two factors that affect the concentration of a hormone in blood; secretion
of that hormone and rate of removal from blood (Guyton and Hall, 2006). As most other
hormones do, TRH is cleared from the body with a certain half-life, where half-life is the
time it takes for half of the amount of a hormone to be cleared from blood in our context.
TRH has a half-life of 6.2 minutes (Motta, 1991).
In short term, changes in TRH secretion rate occur as the levels of thyroid hormones
in blood dictate. However, there might be cases where the stimulation persists at far below
or far above the baseline values. Relying upon the fact that a hormone, which provokes or
inhibits the activity of a gland, can also affect its weight over the long term in certain cases
(Donovan, 1966; Melmed, 2002; Guyton and Hall, 2006), thyroid hormones can also
influence the weight of the hypothalamus. There is not direct evidence that the weight of
the TRH-secreting section of the hypothalamus can be altered according to the circulating
thyroid hormone levels. However, there is evidence that the number of cells that secrete
CRH, which is a hypothalamic hormone analogous to TRH in the regulation of
hypothalamus-pituitary-adrenal (HPA) axis, substantially decline in subjects who
externally receive the hormones that inhibit its secretion (Erkut et al., 1998). Extrapolating
all this information to our case, the weight of the hypothalamus is taken as a variable
quantity.
First, if the magnitude of stimuli from thyroid hormones is persistently far above the
standard levels, it means that the secretory capacity of hypothalamus is consistently
underutilized. In such cases, the specific portions of hypothalamus, which are in charge of
the TRH secretion, would shrink not to retain the redundant capacity in vain. Second, if
thyroid hormones constantly circulate at considerably below normal concentrations, i.e. if
hypothalamus is persistently understimulated, then the hypothalamus would continually
operate at above-normal levels, and thereby expand to adjust its capacity. So, it adjusts its
capacity in the direction that the current needs of the body necessitate.
15
5.1.2. Fundamental Approach and Assumptions
Plasma levels of hormones normally fluctuate throughout the day or from one day to
another because of neurological, psychological, environmental, or similar factors. Though
these fluctuations and the features that influence them might count for some practical
purposes like prescribing the right dose of a drug for a patient, the primary aim of the study
is not to observe the dynamics of diurnal variations of the hormones in the body but rather
to represent the long-term dynamics of the important elements involved in thyroid
hormone system under certain conditions. Thus, the time unit of this study is taken to be
one day, the base values of the variables are taken to be an average value in the model, and
possible variations in hormone levels and neurological, psychological, environmental or
similar other effects are considered to be outside the scope of this study.
The circulating levels of all the hormones in this model are assumed to act according
to set point theory. Here, the set points of the hormones are defined to be their absolute
total quantity in blood. Though it might appear to be erroneous at first sight to take the
absolute quantities of hormones in blood as their set points rather than their concentrations,
it is not so because the blood or plasma volume cannot be too variable. Albeit so, it
wouldn’t still hurt our assumption since this study does not encompass cases where the
changes in the volumes of the fluid, which hormones float in, constitute the problem of
interest.
Secretion rates of hormones are commonly found in some mass unit (like µg, ng etc.)
per unit time. Since the net change in the value of a stock variable is the integral of the net
flow to the stock over time, the units of the flows of a stock is the unit of the stock divided
by the time unit of the model. Therefore, defining the levels of hormones in terms of their
absolute quantities renders it possible to use the secretion rates in their typically defined
units.
When the hypothalamic neurons are excited to secrete releasing hormones, that
hormone is discharged into the hypophysial portal circulation. As mentioned before, this
16
portal system is composed of small blood vessels that link the hypothalamus and the
anterior pituitary. The releasing hormones have only a small distance to travel in order to
communicate with their target cells. Thus, it is enough to release just the quantity of
hormone to the portal circulation to regulate the anterior pituitary hormone in this nearly
isolated communication space. Hence, releasing hormones of hypothalamus circulate in
almost undetectable amounts in systemic blood (Rhoades and Bell, 2009).
Throughout the literature survey, secretion rate of TRH could not be found explicitly
because hypothalamic-hypophyseal portal blood is an extremely difficult area to obtain
blood samples in humans (Rhoades and Bell, 2009). Furthermore, direct measurement of
the secretion rate of a hormone is quite a challenging task. Hence, secretion rates are
commonly inferred from the blood concentration of the hormone and its clearance rate. For
the case of TRH, related literature states that it also circulates in the cerebrospinal fluid
(CSF), which is a serumlike fluid that essentially circulates through the ventricles of the
brain. Firstly, the value for concentration of TRH in CSF, which is stated to range between
65-290 pg/ml (Werner et al., 2005) and taken approximately as 200 pg/ml, is assumed as
its concentration in portal vessels. Secondly, the volume of plasma in these portal vessels is
assumed to be 10 ml. According to these two assumptions, the normal absolute quantity of
TRH in portal vessels is calculated as 2 ng in the model.
The weight of the hypothalamus as a whole is 4000 mg, as mentioned in the previous
section. The percentage of the TRH secreting cells, however, could not be found explicitly
in literature. Thus, it is assumed that 1% of the hypothalamic cells are in charge of TRH
secretion. So, the related weight is taken as 40 mg in the model.
In general, hormones are cleared from the blood with some specific rate. Not only
the hypothalamus sector but the whole model also works according to this principle; the
clearance of each hormone from plasma occurs with respect to a certain fraction, which is
called the “clearance fraction” (clear fr) in the model. In literature, half-lives are
commonly used to quantify the clearance rate of a hormone. Thus, removal of hormones
from blood (or the related fluid) is assumed to follow a first order exponential decay in the
17
model, and the respective clearance fractions are calculated from their half-lives using the
following equation:
where
clearance fraction = ln2 / th
(5.1)
stands for the half-life in days. So, the clearance fractions are in units of
.
There are mainly three determinants of the magnitude of hormonal response of a
target tissue; concentration of the hormone, sensitivity of the target cells, and number of
functional target cells. The sensitivity of a target cell primarily depends on the number of
its operational receptors, the affinity of the receptors for the hormone, and the capacity to
amplify the post-receptor activities.
Firstly, it is the binding of the hormone molecule to its specific receptor which gives
rise to cellular response. And, the probability that a hormone molecule encounters a
receptor molecule is induced by the abundance of both the hormone and the molecule. The
availability of hormone receptors can be altered by the stimulating hormone itself or by
another hormone. For instance, it is stated that T3 decreases the sensitivity of the TSHsecreting anterior pituitary cells to TRH (Goodman, 2009). Secondly, affinity is a measure
of the tightness of binding or the likelihood of an encounter between a hormone and its
receptor that result in binding. Some sources suggest that binding of a hormone to its
receptor affects the affinity of unoccupied receptors. Thirdly, the post-receptor capacity of
a target cell implies how well the cell can react to a unit magnitude of stimuli (Goodman,
2009; Rhoades and Bell, 2009). The first two ingredients of sensitivity and the
circumstances that alter them are not explicitly included in the model, and are considered
out of the scope of this study. The third one, however, is implicitly counted by allowing the
intensity of hormonal stimulation to alter the secretory rates of the target cells to a certain
extent.
18
The number of target cells is also not explicitly incorporated in the model; the
weights of the glands are used as an indicator instead. As the weight of a gland increases,
the competence or the capacity to respond to hormonal stimuli increases too. So, only the
concentration of the hormone, the weight of the related gland or tissue, and the capacity of
cells (more precisely, the capacity of a unit weight of gland or tissue) are assumed to
dictate the response of the target tissue.
One last remark is that when using the term hypothalamus weight, the weight of the
relevant portion of the hypothalamus, i.e. the weight of the section responsible for TRH
release, will be assumed.
5.1.3. Description of the Structure
The structure constructed in this sector aims to depict the first tier in the regulation of
the thyroid hormone system. As mentioned before, the hypothalamus and the related
releasing hormone TRH are the top-level controllers of the negative feedback mechanism
in the functioning of thyroid hormone system. TRH plays a chief role in the functioning of
hypothalamic–pituitary–thyroid axis (HPT-axis) as the only positive effector of TSH
secretion from the pituitary, TSH being the only direct positive stimulant of thyroid
hormone synthesis and secretion.
The stock-flow diagram of the sector is given in Figure 5.1. The sector involves two
main stock variables; Hypo Wt (hypothalamus weight) and TRH.
To begin with TRH, the only inflow to this stock is its secretion rate, and the only
outflow from TRH is its clearance rate. The secretion rate of TRH is determined according
to both the levels of the thyroid hormones in blood and current capability of the
hypothalamus. But, before figuring out the actual TRH secretion from the hypothalamus,
implied TRH secretion (imp TRH sec) is calculated. This implied secretion merely contains
the effect of thyroid hormone concentration on secretion as if the hypothalamus has infinite
capacity to secrete. That is, the implied secretion is a measure of how much TRH secretion
19
thyroid hormones would dictate regardless of the short-term secretory capability of the
hypothalamus. Then, this implied secretion rate is exposed to the capacity restrictions of
the hypothalamus and as much TRH as the capacity permits is secreted. It is calculated
according to Equation 5.2 and 5.3.
ratio of des hypo
wt to hypo wt
normal hypo
wt
gr for eff on
HAT
HAT
des hypo wt
eff of imp TRH sec
on hypo wt
Hypo Wt
Hypo wt chg
gr for eff of imp
TRH sec on hypo wt
normal hypo
prod
ratio of smth imp
TRH sec to normal
normal TRH
sec
smth imp TRH
sec
imp TRH sec
eff of TH on
TRH sec
hypo cap
TRH clear fr
TRH
TRH clear
rate
TRH sec rate
ratio of imp TRH
sec to hypo cap
gr for hypo
cap
eff of cap on
TRH sec
gr for eff of TH
on TRH sec
MW of T3
log ratio of TH
to normal
free T3 in
blood
normal TH
total free T3
molecules
ratio of TH to
normal TH
total free T3&T4
molecules
MW of T4
total free T4
molecules
Figure 5.1. Stock-flow diagram of the hypothalamus sector.
free T4 in
blood
20
imp hypo sec = normal TRH sec × eff of TH on TRH sec
(5.2)
eff of TH on TRH sec = f (log(total TH / normal TH))
(5.3)
where f (log(total TH / normal TH)) is defined as in Figure 5.2.
10
9
eff of TH on TRH sec
8
7
6
5
4
3
2
0
-1.1
-0.8
-0.6
-0.4
-0.2
-0
0.2
0.4
0.6
0.8
1
log ratio TH to normal
Figure 5.2. Effect of thyroid hormones on TRH secretion.
When the thyroid hormone levels stay at their neutral values, the implied TRH
secretion remains at the normal secretion value. However, when the circulating levels of
thyroid hormones are disturbed from their set points, i.e. if the ratio of total circulating
unbound thyroid hormones to the normal is different than one, the implied TRH secretion
will be altered in the opposite direction of the shift in the thyroid hormone levels, as the
negative feedback regulation necessitates.
The work of Goodman (2009) suggests that the magnitude of the biological response
of a target cell can be explained as a function of the logarithm of the concentration of the
effector hormone. Thus, the logarithm of the ratio of hormone levels relative to the normal
levels is used in the model when quantifying the hormonal effect on the response of the
target tissue. So, not directly the ratio of circulating thyroid hormones to normal but the
logarithm of it is used as an input to the graphical effect function shown in Figure 5.2.
21
According to the graphical function in Figure 5.2, if the thyroid hormone levels are
far above their baseline values, the TRH secretion falls to considerably low values, though
not to zero. The reason why hormone secretion does not reset is that most hormonesecreting tissues exhibit minimal (basal) secretion in the absence of stimulatory signals, as
suggested by the related literature (Negi, 2009). The resistance of the hypothalamus not to
reset but to remain at some basal secretion values are achieved via the nonzero right
endpoint of the graphical function.
The last step in the determination of TRH secretion is to expose the implied secretion
rate to the capacity restrictions of the hypothalamus. The secretory capacity of
hypothalamus is an upper bound to the total amount of TRH that can be maximally
secreted daily. The way this capacity is defined is shown in Equation 5.4.
hypo cap = Hypo Wt × normal hypo prod × 10
(5.4)
Two main ingredients are involved in the definition of hypothalamic capacity; the
normal productivity of the hypothalamus and the weight of the hypothalamus. The term
productivity implies the production or release amount per unit weight. The normal
productivity is defined to be the amount of TRH that one unit weight of the hypothalamus
secretes under normal physiological conditions, and is a constant. This normal productivity
is then multiplied with ten because it is assumed that one unit weight of the hypothalamus
is capable of secreting ten times the normal amount maximally. And so, the overall
capacity of the hypothalamus is defined as the product of the maximal secretory capacity
of a unit weight with the current hypothalamus weight.
TRH sec rate = eff of cap on hypo prod × hypo cap
(5.5)
eff of cap on TRH sec = f (imp TRH sec / hypo cap)
(5.6)
where f (imp TRH sec / hypo cap) is defined as in Figure 5.3.
22
Figure 5.3. Graphical function for the effect of capacity on TRH secretion.
Equations 5.5 and 5.6 depict how the actual TRH secretion computed as a function of
the capacity and implied secretion. According to the graphical function shown in Figure
5.3, when the implied secretion operates appreciably away from the capacity of
hypothalamus, the capacity constraint does not become binding and the actual secretion
equals to the implied. But, as the implied levels tend to push the capacity limit, a littler
fraction of the implied secretion is allowed to realize. The secretory capacity of
hypothalamus is fully utilized only if the implied secretion considerably exceeds the
capacity. So, the extent at which the falls in thyroid hormone levels immediately influence
the TRH secretion is confined to the short-term adaptation competence of the hypothalamic
cells. If somehow a very high level of TRH secretion is demanded, the hypothalamus
would only secrete as much as its existing capacity permits. So, this means that when
necessary, the hypothalamus would utilize its maximum capacity to meet high TRH
requests immediately, but may not suffice to conform the “orders” in short term.
The formulations for the calculation of the TRH secretion provide some flexibility in
the short run. As explained in section 5.1.1, the weight of the hypothalamus can change in
conditions where it is persistently forced to over- or underfunction. In the model, this
phenomenon is constructed as such: First, implied secretion rate is calculated. This implied
23
secretion may or may not actualize depending on the capacity limits. However, it is
important to retain this piece of information because it tells how much the secretion would
have been if there were no restrictions on it. This information does not immediately show
its effect on the weight of the hypothalamus, and that’s what is meant by the term
“persistent”. Generally, hormone-secreting tissues in a way accommodate themselves to
the needs of the body after some time. That is, these tissues do not opt for weight
adjustment in case of transient and drastic shifts from the baseline values, and usually
show some inertia against weight changes. For this reason, the implied secretion levels are
smoothed with a third order information delay structure in the model, where the overall
delay duration is chosen to be 20 days. Smoothing provides a defence mechanism to
preserve the normal weight against transient switches in secretion rates. Yet, smoothing is
the first step. The second step is to check whether the smoothed implied secretion rates
exceed some limits. This is done to ensure that the hypothalamus indeed functions at levels
appreciably away from normals, and there is need for modifications in the weight. Thus,
the weight of the hypothalamus is affected only if the smoothed implied secretion values
relative to the normal values surpass some threshold values. The graphical function
depicting this effect is shown in Figure 5.4.
eff of imp TRH sec on hypo wt
3.7
3
2
1
0
0
1
2
3
4
5
6
7
8
9
10
11
12
ratio of smth imp TRH sec to normal
Figure 5.4. Graphical function for the effect of implied TRH secretion on hypothalamus
weight.
24
The input to this graphical function is the ratio of smoothed implied TRH secretion
to the normal TRH secretion, and the output turns out to be some coefficient to be
multiplied with the normal hypothalamus weight to figure the desired hypothalamus
weight. The desired hypothalamus weight constitutes a target for the current hypothalamus
weight. Gradually, the hypothalamus converges to that target value. Convergence to the
target value is facilitated through the classical stock adjustment formulation, which is
shown in Equation 5.8.
des hypo wt = normal hypo wt × eff of imp TRH sec on hypo wt
(5.7)
Hypo wt chg = (des hypo wt −Hypo Wt) / HAT
(5.8)
The above equation is the formula for the flow of the stock that stands for the
hypothalamus size. The adjustment time is a measure of how fast the hormone-secreting
tissue tends to correct the difference between the target and current value. The adjustment
time for hypothalamic weight change (HAT) is not a constant; it changes according to the
ratio of the desired hypothalamus weight to the current hypothalamus weight (ratio of des
hypo wt to hypo wt). It is not very reasonable to set the speed to correct the discrepancy
regardless of the magnitude of that discrepancy. The variable ratio of des hypo wt to hypo
wt is used as a measure of convergence speed of the hypothalamus to reach the desired
level. If the desired weight is too high relative to the current weight, then it should take
more time for the hypothalamus to adjust itself to the desired weight. In a sense, the current
weight is regarded like the capacity of hypothalamus that determines the rapidity of
approaching the desired level. Thus, as ratio of des hypo wt to hypo wt increases, the
adjustment time increases too. The graphical function for HAT is shown in Figure 5.5.
Ultimately, depending on the level of thyroid hormones in blood, and the capacity of
the hypothalamus, a certain amount of TRH is released into the portal circulation to
interact with the thyrotrophs in the anterior pituitary and trigger TSH secretion.
25
250
eff on HAT
200
150
100
30
1
1.5
2
2.5
3
3.5
4
4.5
5
ratio of des hypo wt to hypo wt
Figure 5.5. Graphical function for effect on hypothalamic adjustment time.
5.2. Pituitary Sector
5.2.1. Background Information
The pituitary gland, or alternatively called hypophysis, is a complex endocrine organ
positioned in the sella turcica, a bony cavity at the base of the brain, and is linked to the
hypothalamus by a stalk (Guyton and Hall, 2006). The weight of this gland is
approximately 600 milligrams in adult human (Donovan, 1966; Sodeman and Sodeman,
1985; Kronenberg et al., 2008; Guyton and Hall, 2006). The pituitary secretes many
hormones, which take part in various physiological processes by either acting directly on
the target cells, or stimulating other endocrine glands to secrete hormones leading to
alterations in body function. The human pituitary is comprised of two morphologically and
functionally distinct glands that are connected to the hypothalamus. These two glands are
called the neurohypophysis and the adenohypophysis, also known as the anterior pituitary.
The anterior lobe of the pituitary comprises 75% of the pituitary gland. The cells of the
anterior lobe secrete six different hormones, and a distinct specialized cluster of cells
secretes each of these hormones. TSH is one of the hormones that the anterior pituitary is
in charge of synthesizing and secreting, and the cells specialized for TSH are called
26
thyrotrophs. The thyrotrophs, i.e. TSH-secreting cells, compose 5% of the anterior
pituitary cells (Bhagavan, 2002; Guyton and Hall, 2006; Kronenberg et al., 2008; Rhoades
and Bell, 2009).
TSH, also known as thyrotropin, is the principal regulator of thyroid hormone
synthesis and secretion for it is the eventual messenger in the stimulation of the thyroid
gland. As noted earlier, TRH plays the major role in the positive regulation of TSH
secretion. Upon secretion, TRH reaches the anterior pituitary through the portal blood
system, impinges upon the thyrotrophs, and binds to specific receptors on these cells.
Binding of TRH with its receptors on thyrotrophs activates a number of intracellular
mechanisms which ultimately lead to TSH release. However, it is not only TRH that
influences the rate of TSH secretion, but also the levels of thyroid hormones in blood.
Thyroid hormones exert a suppressive, negative feedback effect on the thyrotrophs to
prevent the oversecretion of TSH, as opposed to the augmenting effect of TRH. Some
portion of circulating free thyroid hormones binds with the unique thyroid hormone
receptors, TR’s, on the thyrotrophs, and exerts a suppressive effect on TSH release. This
means that an increase in circulating thyroid hormone concentrations would lead to a
reduction in the rate of TSH secretion; and a decrease would result in a rise in TSH
secretion. Consequently, the magnitude of TSH secretion is induced by the opposing
signals to the anterior pituitary, one by TRH and the other by the thyroid hormones
(Bhagavan, 2002; Guyton and Hall, 2006).
The time it takes for the contrasting effects of TRH and thyroid hormones on TSH
release to be revealed are different indeed. TRH elicits a prompt release of TSH within
minutes (~15 minutes), while the inhibitory effect of thyroid hormones becomes evident
after several hours (Bhagavan, 2002). Still, the time lag between the effect of TRH and
thyroid hormones on TSH does not make much difference because the time unit of our
model is one day and all these occur within a day anyway. Upon stimulation of the anterior
pituitary by TRH, TSH is released into the circulation.
27
TSH is typically measured in “microunits” (µU) or “milliunits” (mU). Normal range
for TSH secretion rate is 40-150 µU/day, and for circulating TSH in plasma 0.3-4 µU/ml
(Kronenberg et al., 2008; Oertli and Udelsman, 2007). And, the half-life of TSH is about
one hour (Negi, 2009).
It is stated that long-standing hypothyroidism may lead to pituitary enlargement
(Melmed, 2002), and increasing the negative feedback by any mechanism may result in
atrophy of the thyrotrophs (Tucker, 1999). In other words, prolonged overstimulation may
lead to expansion in pituitary size, and conversely sustained understimulation to shrinkage.
5.2.2. Fundamental Approach and Assumptions
In this study, when speaking of changes in the weight of the pituitary, it will always
be referred to the thyrotrophs, i.e. cells that secrete the TSH. The assumptions about the
sensitivity of target cells explained in hypothalamus sector are valid for the pituitary too.
As aforesaid, the set points for the levels of hormones in blood are taken to be the
absolute quantities of the hormones rather than their concentrations. This is simply done by
multiplying the relative concentration of the hormone with the total plasma volume. In this
model, plasma volume is taken as 3 litres (Rhoades, 2009). This approach is qualitatively
and quantitatively valid both for TSH and the two thyroid hormones.
5.2.3. Description of the Structure
The structure of this sector is nearly the same as that of the hypothalamus sector.
Two main stock variables are involved; TSH and Pituitary Weight (see the stock-flow
diagram in Figure 5.6). The distinction is that TSH secretion has two effectors as opposed
to thyroid hormones being the single effector of TRH secretion. Here, it is not only the
circulating thyroid hormones that act on the secretion rate of TSH, but also TRH from
hypothalamus. As mentioned earlier, the functioning of the thyroid hormone system is
governed by a double-armed negative feedback mechanism. So, both the stimulant effect
28
of TRH and the inhibitory effect of thyroid hormones ought to be taken into account when
figuring the rate of TSH secretion. The impact of these two factors is formulated as the
product of two distinct effect functions. The one that counts for thyroid hormone inhibition
is a decreasing function, and the one for TRH is an increasing one.
gr for eff on
PAT
ratio of des pit wt
to pit wt
normal
pit wt
PAT
des pit wt
thres gr
for pit
<TRH>
Pit Wt
eff of smth imp
TRH on pit wt
Pit wt chg
normal pit
prod
ratio of smth
imp TSH sec
to normal
normal
TRH
smth imp
TSH sec
ratio of TRH
to normal
normal
TSH sec
eff of TRH on
TSH sec
gr for eff of TRH
on TSH sec
TSH
TSH clear rate
TSH sec rate
eff of cap on
TSH sec
imp TSH sec
log ratio of
TRH to normal
TSH clear fr
pit cap
ratio of imp TSH
sec to pit cap
gr for pit cap
eff of TH on
TSH sec
log ratio of
TH to normal
gr for eff of TH
on TSH sec
Figure 5.6. Stock-flow diagram of the pituitary sector.
The work of Guyton and Hall (2006) states that when the blood flow in portal vessels
from hypothalamus to pituitary is completely hindered, TSH secretion rate diminishes
29
substantially but isn’t cut back to zero, remains at basal levels. The qualitative and
quantitative structure of Equation 5.9 is constructed based on this statement. First, it is
ensured that the graphical function for the effect of TRH on TSH secretion does not
become zero, but yields a considerably small value when TRH stimulus is non-existent.
Second, from this statement it can be inferred that the prerequisite for significant TSH
secretion is TRH stimulation; low levels of thyroid hormones alone wouldn’t help enhance
TSH secretion. Thus, effect of thyroid hormones should in a way depend on TRH effect; it
should not be allowed to act independently. The dependency is provided by the
multiplicative formulation. By enforcing the graphical function for thyroid hormone effect
to yield the value one for all subnormal levels of thyroid hormones, they are only allowed
to abate the existing stimulatory impact of TRH on TSH secretion.
The implied secretion rates are calculated as a function of the logarithm of the ratio
of the stimulant or inhibitory hormone level to its normal level, as in the hypothalamus
sector. Here again, implied secretion is computed before the actual. The calculation of
implied secretion includes both the effect of thyroid hormones and TRH, and excludes the
capacity restriction.
imp TSH sec = eff of TRH on TSH sec × eff of TH on TSH sec × normal TSH sec (5.9)
eff of TRH on TSH sec = f (log(TRH / normal TRH) )
(5.10)
eff of TH on TSH sec = f (log(total TH / normal TH))
(5.11)
where f (log(total TH / normal TH)) and f (log(TRH / normal TRH)) are defined as in
Figure 5.7 and Figure 5.8.
And, in the exact same manner as in the hypothalamus sector, the implied secretion
rate is constrained with capacity limit according to the following set of equations:
30
TSH sec rate = eff of cap on TSH sec × pit cap
(5.12)
eff of cap on TSH sec = f (imp TSH sec / pit cap)
(5.13)
10.1
9
eff of TRH on TSH sec
8
7
6
5
4
3
2
0
-1
-0.8
-0.6
-0.4
-0.2
-0
0.2
0.4
0.6
0.8
1.1
log ratio TRH to normal
Figure 5.7. Graphical function for the effect of TRH on TSH secretion.
eff of TH on TSH sec
1
0.8
0.6
0.4
0.2
0
0
0.2
0.4
0.6
0.8
1
log ratio TH to normal
Figure 5.8. Graphical function for the effect of thyroid hormones on TSH secretion.
Variations in secretion amounts happen in a very short while, almost immediately
(Melmed, 2002). In the long run, the pituitary may adjust its weight in case over- or
understimulation lingers for a sufficiently long period of time, in the same fashion as the
31
hypothalamus does. Here again, the implied secretion rates are smoothed via a third order
information delay structure with a delay time of 20 days. In the same manner as clarified in
section 3.1.3, the ratio of these smoothed values to its normal is filtered through a graphical
function. Using the output of that function, a desired weight is calculated at every step.
As mentioned before, the weight of the entire pituitary gland is around 600 mg, and
the anterior lobe constitutes 75% of it. So, the anterior lobe weighs 450 mg. Since the
TSH-secreting cells compose 5% of the anterior lobe, the normal weight of the pituitary is
taken as 22.5 mg. The normal secretion rate of TSH is set to nearly 110 mU/day, and
circulating TSH levels, i.e. the value of the stock, to 6.6 mU (i.e., 2.2 mU/l or µU/ml).
5.3. Thyroid Sector
5.3.1. Background Information
Thyroid hormones are the primary regulators of metabolic functions in the body, and
almost all cells of the body are regularly subjected to the actions of thyroid hormones.
They are vital for proper development and differentiation of the cells of the human body,
and their deficiency result in serious or even life-threatening diseases.
The human thyroid gland, located just below the larynx, is one of the largest
endocrine glands, and is comprised of two lobes attached to either side of and anterior to
the trachea. The thyroid gland in a healthy adult normally weighs about 20 grams. The
gland is composed of spherical follicles filled with a gel-like substance called colloid, and
surrounded by follicular cells (alternatively called thyrocytes). The primary ingredient of
colloid is a large protein called thyroglobulin, which is the site where the thyroid hormones
are formed and stored (Guyton and Hall, 2006; Rhoades and Bell, 2009).
The synthesis and secretion of thyroid hormones initiates upon the stimulation of the
thyroid by TSH. Binding of TSH with TSH receptors on follicular cells triggers a series of
intracellular functions in these cells to synthesize and release thyroid hormones. For the
32
synthesis of thyroid hormones, iodide is indispensable. So, the first step in the formation of
these hormones is the uptake of available iodide into follicular cells. There, iodide is
converted into an active form called iodine, which is the constituent part of thyroid
hormones. Then, iodine attaches to tyrosine residues within thyroglobulin molecules. This
process, i.e. binding of iodine to tyrosine residues within thyroglobulin, is called
organification. Coupling of one iodine atom with a tyrosine molecule creates
monoiodotyrosine (MIT). When MIT is iodized once more, a diiodotyrosine (DIT)
molecule is formed. So, tyrosine is first iodized to monoiodotyrosine and then to
diiodotyrosine. And, thyroid hormones are formed from these two kinds of molecules.
When one MIT and one DIT molecule couples, one molecule of triiodothyronine, T3, is
formed; and when two DIT’s come together, one molecule of thyroxine, T4, is created
(Bhagavan, 2002; Guyton and Hall, 2006; Rhoades and Bell, 2009). So, formation of one
unit of T4 necessitates double the amount of iodine used for the production of one unit of
T3. The molecular weights of T3 and T4 are 651 and 777 Da, respectively (Bhagavan,
2002), where Da (Dalton) is a unit commonly used to measure mass on atomic or
molecular scale, and has a value of about 1.66054 × 10-24 g (Raymond, 2009).
After being synthesized, thyroid hormones reside in thyroglobulins, unless cleaved
from them on demand. Stimulation of thyroid glandular cells by TSH not only promotes
the synthesis of thyroid hormones, but also the secretion of them. In fact, the most rapid
impact of TSH stimulation on the thyroid is the initiation of breakdown of thyroglobulin,
which results in the secretion of T3 and T4 within half an hour. For this to happen,
follicular cells engulf bits of the colloid, internalizes the colloid droplet into the cells,
disintegrates it by the help of enzymes, allow the hormones to discharge from the storage
element thyroglobulin, and release them into the blood circulation. So, TSH stimulation
simultaneously activates all the secretory mechanisms of thyroid glandular cells, but the
fastest among them is the secretion process. Though synthesis requires a relatively longer
time compared to the secretion process, it still happens within one day under normal
conditions (Guyton and Hall, 2006; Werner et al., 2005; Rhoades and Bell, 2009).
33
One unique characteristic of thyroid gland, in contrast to most endocrine glands, is
that it has a considerably large capacity to store thyroid hormones in itself. In literature, it
is stated that the thyroid gland is able to store approximately two months’ supply of thyroid
hormones in it. Thus, if synthesis of thyroid hormone ceases, the physiologic effects may
not be recognized for about two months (Molina, 2004; Guyton and Hall, 2006;
Kronenberg et al., 2008). In a sense, these stores serve as buffers to guard against sudden
and transient dysfunctions in the thyroid system and thus helps preserve the healthy state of
the body.
Normally, T4 constitutes 93% of the thyroid hormones released daily from the
thyroid gland, and only 7% is T3. The functions of these two hormones are qualitatively
the same; however, they differ from each other in terms of rapidity and intensity of action.
T3 is said to be physiologically active form of the thyroid hormones (Guyton and Hall,
2006; Rhoades and Bell, 2009). T4 can only be synthesized in the thyroid gland and is the
major secretory product of the thyroid gland. The normal production and secretion rate of
T4 from the thyroid is approximately 90 µg/day. On the other hand, only 20% of T3 is
produced directly by the thyroid; the rest is generated by enzymatic removal of one iodine
atom (deiodination) of T4 molecules in peripheral tissues. The production rate of T3,
including the peripheral conversions, is 35 µg/day (Braunwald et al., 2001; Bhagavan,
2002).
Upon stimulation by TSH, T3 and T4 are released into the blood stream. Most of the
T3 and T4 molecules become bound to plasma proteins, only less than 1% of them
circulate in free form. Normally, the range for total plasma concentration is 4-11 µg/dl for
T4, and 75-220 ng/dl for T3. Specifically, 0.02% of T4 and 0.3% of T3 circulates in
unbound form. Merely the free portion of the hormones is biologically active and able to
interact with target cells (Rhoades and Bell, 2009). And so, it is the circulating free
hormones that feed back to the hypothalamus and pituitary to reduce the secretion of TRH
and TSH (Bhagavan, 2002; Rhoades and Bell, 2009).
34
In general, hormones are “cleared” from the plasma by various means involving
metabolic destruction by the tissues, binding with the tissues, excretion by the liver into the
bile, and excretion by the kidneys into the urine (Guyton and Hall, 2006). For our case, it
was recognized early that T4 and T3 were dispersed widely into tissues in addition to the
blood (Hays, 2009). It is stated that about 40% of plasma T4 is converted to T3 and about
40% to reverse triiodothyronine (rT3), which is a metabolically inactive form. The half-life
of T4 in the bloodstream is approximately 7 days, whereas that of circulating T3 is about 1
day (Rhoades and Bell, 2009).
Like the hypothalamus and pituitary, the weight of thyroid gland may also be altered
under certain circumstances. The work of Vassart and Dumont (1992) asserts that
hypophysectomy, hypopituitarism, or an isolated TSH deficiency, i.e. the conditions that
clearly abate the thyroid function, leads to thyroid atrophy. Conversely, chronic stimulation
of the thyroid for some reason is stated to enhance thyroid growth.
5.3.2. Fundamental Approach and Assumptions
The stock variables for the blood levels of thyroid hormones represent the total
circulating amount of them, both bound and unbound (free). Bound and unbound hormones
are in a dynamic equilibrium with each other. However, only the free portion is
biologically active. So, it is merely the small unbound portion of thyroid hormones that is
able to diffuse into peripheral tissues, induce metabolic effects, and that undergoes
deiodination or degradation. When free hormones disperse out of the blood stream, the
equilibrium is disturbed. Thus, the carrier proteins free additional thyroid hormones until
the equilibrium state is restored (Kronenberg et al., 2008; Rhoades and Bell, 2009; Martini,
2007). As far as the scope and the objective of this study are concerned, this process is not
explicitly modeled. Instead, for each case, e.g. diffusion of the hormone into peripheral
tissues, conversion into some other form etc., it is simply assumed that some fraction of the
total circulating thyroid hormones leave the blood stream and diffuse into relevant parts of
the body.
35
Related literature suggests that under certain physiological or pathological conditions
the total circulating hormone content and amount of plasma transport proteins may change,
while the free hormone concentration may remain relatively normal. In the model,
however, the quantity of each thyroid hormone that is unbound is assumed some given
constant fraction of total circulating hormones.
As mentioned earlier, under certain circumstances the weight of the thyroid may
change. There are studies, however, where the volume of the thyroid is measured rather
than its weight (probably because volume measurement does not require the ablation of the
gland as in the assessment of the weight). It is assumed that changes in the volume of the
thyroid go parallel with the changes in the weight. These two notions will be used
interchangeably when necessary.
5.3.3. Description of the Structure
This sector tries to illustrate the structure of the third and last tier in the control of
thyroid hormone system. The stock-flow diagram of thyroid sector is given in Figure 5.9. It
involves five main stock variables; Thy Wt (thyroid weight), T4 Store, T3 Store, T4 in
Blood and T3 in Blood.
As mentioned before, the thyroid synthesizes and secretes two hormones, T3 and T4.
The structures that represent the mechanisms in the synthetic and secretory regulation of
T3 and T4 are quite similar, though not the same. To begin with T4, there are two stocks
and their associated flows that involve the main measures about T4 in the model. The stock
variable named T4 in Blood represents the overall amount, both bound and unbound, of
circulating T4 in blood. It is subject to a single inflow, and four different outflows. The
single inflow to this stock is the secretion rate of T4. Under normal conditions, T4
secretion rate is set to 90 µg/day.
36
gr for eff of
imp TH sec
on thy wt
<TSH>
TAT
ratio of
smth imp
TH sec to
normal
normal
TSH
ratio of TSH
to normal
smth imp TH sec
log ratio
of TSH
short smth imp
TH sec
<normal
TH sec>
ratio of
short smth
imp TH sec
to normal
<I in Thy>
gr for eff
on TAT
I inhib thres
des thy wt
normal I
in thy
Thy Wt
Thy wt chg
normal
TH sec
imp TH sec
<imp TH sec>
ratio of des thy wt
to thy wt
eff of imp
TH sec on normal
thy wt
thy wt
eff of
TSH on
TH sec
ratio of imp
TH sec to
thy cap
gr for
thy cap
normal thy
prod
thy cap
eff of cap
on TH sec
ratio of I in thy to
thres
eff of I on
thy cap
pot TH sec
gr for eff of
I on cap
fr of
T4 sec
<fr of
T3 sec>
pot T4 sec
gr for eff
of TSH
ratio of
on TH sec
pos to pot
gr for TH
<disc btw pot TH syn
T4 sec
store cap
gr forand I rest TH syn>
Conv
thy stim
pos
T4
Abs rate
<T3
syn
sec
rate to
on T3 fr
of T4 by
<pot TH syn> rate>
eff of T4
rT3
T4
tissues
store cap
clear fr
eff of
normal
thy stim
total free T3 ratio of T3
T4 in Blood
T4 Store
on T3 fr
to T4
molecules
T4 syn rate
T4 clear rate
T4 sec rate
pot
fr
of
gr
for
fr
ratio of
T4 to T3
des T4 syn
disc from
T3 sec
T3 to T4
of T3 sec
normal
conv rate
des T4 store <fr of T4 sec>
T4 to T3
conv fr
T4
store
adj
total free T4
thy syn cap
T4 to T3
for T4
conv fr
molecules fr of T3 sec
des T4 store
<fr of T4
gr for eff
sec>
ratio of
of T3 on
<gr for
AT for
des T4 syn
total
normal
TH
peri conv
thy cap>
to cap
<thy cap>
store restor
store
eff of T3 conc
on peri conv
ratio
of
<fr
of
<thy syn cap
thy syn cap
des T3
eff
of
thy
normal T3
syn
to
cap
T3
sec>
for T4>
cap on T4
for T3
syn
in blood
T3 store
des T3 syn
adj
des T3 store
eff of thy
pot T4 syn
ratio of T3
pot T3 syn
T3 from
cap on
to normal
deiod of
T3 syn
T4
disc from
<gr for
pot I cons
pot
TH
syn
thy cap>
for T4
des T3 store
T3 clear fr
pot I cons
for T3
T3 in Blood
T3 Store
T3 clear rate
T3 syn rate
disc btw pot TH syn
T3 sec rate
and I rest TH syn disc btw pot
eff of T3
T3 syn and I
Abs rate
pot T3 sec store cap
rest T3 syn eff of pref T3
ratio of
of T3 by
syn on red in pos T3 sec
pot to pos ratio of cap rest I
tissues
T3
syn
I cons
cons to pot
<fr of <pot TH
ratio of disc btw
T3 sec> sec>
I rest syn and
eff of thy
total pot syn to
pot total I
gr
for
eff
of
I cap
total pot syn
cons
ratio of <gr for TH
gr for I
under I
pref T3 syn
pos to pot store cap>
store
cap rest
T3 sec
cap
<I in Thy>
pos I cons
pot total
I cons
Figure 5.9. Stock-flow diagram of the thyroid sector.
37
As the stock-flow diagram reveals, the amount of T4 to be secreted is withdrawn
from the T4 Store stock. In general, it is not very reasonable to let the outflow of a stock to
act independent from the value of that stock. And also, the body does not utilize its
resources regardless of its present status. The thyroid hormone stores are high when
compared to the daily normal requirements. The work of Bürgi (2010) suggests that when
thyroid hormone synthesis is obstructed somehow, hormone secretion diminishes only
after significant amount of the stores is depleted, which takes several weeks in human.
Considering this proposition, it is assumed that there has to be some limit to the amount of
thyroid hormones that could maximally be withdrawn and secreted from these stores
within a day. This limit is based on the current level of the stores in the model. If the
demand dictated by the hormonal stimuli somehow exceeds or is sufficiently close to the
amount of hormone that the target tissue is willing to maximally release, it would adjust its
sensitivity according to its existing state and respond as a function of both the imposed
requirements and its current status. As the stores diminish, the amount that the gland would
be willing to release declines too. So, the potential rate of T4 secretion is constrained by an
effect function which counts for the capacity of hormone stores. The equation for T4
secretion rate is formulated as shown in Equation 5.14.
T4 sec rate = pot T4 sec × eff of T4 store cap
(5.14)
eff of T4 store cap = f (pos T4 sec / pot T4 sec)
(5.15)
where f (pos T4 sec / pot T4 sec) is defined as in Figure 5.10.
The input to the graphical effect function in Figure 5.10 is the ratio of possible T4
secretion (pos T4 sec) to potential T4 section (pot T4 sec) where possible T4 secretion is
computed by multiplying some coefficient with the current value of T4 store. Possible T4
secretion means that given the current value of T4 store, the thyroid would avoid to release
more than a certain fraction of its supplies, as explained in the preceding paragraph. This
fraction is selected to be 0.15 in the model. According to this graphical function, the entire
38
potential amount is allowed for secretion if it is not sufficiently close to the upper limit, i.e.
possible secretion. But as the potential value tends toward this maximum possible, the
thyroid becomes reluctant to push its limits, and releases the whole possible amount only
when fairly more than the maximum possible is desired. Consistent with the findings
suggested by Bürgi (2010), when daily demands are approximately at normal levels, the
constraint on daily secretion imposed by possible T4 secretion does not become a binding
one in the model until an appreciable portion of stores is exhausted.
1
eff of TH store cap
0.8
0.6
0.4
0.2
0
0
0.2
0.4
0.6
0.8
1
1.2
1.4
1.5
ratio of pos to pot T4 sec
Figure 5.10. Graphical function for the effect of thyroid hormone store capacity.
The second factor that participates in the calculation of T4 secretion is the potential
T4 secretion (pot T4 sec). It is some target amount for T4 secretion rate and is calculated
using Equation 5.16.
pot T4 sec = pot TH sec × fr of T4 sec
(5.16)
pot TH sec = eff of cap on TH sec × thy cap
(5.17)
To begin with the first element in the equation, potential thyroid hormone secretion
(pot TH sec) is some raw value for total thyroid hormone secretion not yet exposed to
hormone store limitation. It is calculated in the same way as the TRH and TSH secretions
39
have been; that is, by subjecting the implied total thyroid hormone secretion to the effect of
thyroid capacity. Here, since some additional constraints exist to possibly limit this rate
further, it is attributed to a potential value rather than actual.
imp TH sec = normal TH sec × eff of TSH on TH sec
(5.18)
eff of TSH on TH sec = f (log(TSH / normal TSH))
(5.19)
where f (log(TSH / normal TSH)) is depicted in Figure 5.11.
10.1
9
eff of TSH on TH sec
8
7
6
5
4
3
2
0
-1
-0.8
-0.6
-0.4
-0.2
-0
0.2
0.4
0.6
0.8
1.1
log ratio TSH to normal
Figure 5.11. The graphical function for the effect of TSH on thyroid hormone secretion.
The calculation of the potential thyroid hormone secretion is done by constraining
the implied thyroid hormone secretion with thyroid capacity, as just mentioned, but the
capacity of the thyroid is computed in a slightly modified way in this case (see Equation
5.20). First, as in the previous two sectors, ten times the normal thyroid productivity is
multiplied with the weight of the thyroid to find the maximal amount for secretion or
synthesis that the thyroid is capable of. Then, this term is further multiplied with the effect
of iodide on thyroid capacity (eff of I on thy cap) to count for the mild impairment in
thyroidal secretion in high intrathyroidal iodide concentrations. There are a number of
40
studies where high doses of iodine are administered to subjects for a short period of time,
and mild but significant decreases in serum T3 and T4 levels and increase in TSH levels
are observed (Vagenakis et al., 1973; Gardner et al., 1988; Paul et al., 1988; Philippou et
al., 1992; Georgitis et al., 1993; Namba et al., 1993; Lemar et al., 1995; McKonigal et al.,
2000). The decrease in thyroid hormone concentrations is attributed to high intrathyroidal
iodine concentrations. So, depending on the concentration, intrathyroidal iodine
concentration may contract the capacity of the thyroid.
thy cap = normal thy prod × Thy Wt × 10 × eff of I on thy cap
(5.20)
eff of I on thy cap = f (I in Thy / I inhib thres)
(5.21)
where f(I in Thy / I inhib thres) is defined as in Figure 5.12.
1
eff of I on thy cap
0.8
0.6
0.4
0.2
0.085
0.9
1
1.1
1.2
1.3
1.4
1.5
ratio of I in thy to thres
Figure 5.12. Graphical function for the effect of iodine on thyroid capacity.
According to the graphical function in Figure 5.12, as the iodine concentration within
the gland tends to the threshold value, the capacity of the thyroid declines. But the real
inhibitory effect takes place when the iodine levels surpass the threshold value because
only then the total capacity of the thyroid falls below the value that is necessitated for
normal hormone production. As the iodine levels exceed the threshold more, the inhibitory
41
effect on thyroid capacity rises too. To find the inhibitory threshold, firstly the thyroidal
iodine levels are smoothed with a third order information delay structure using a delay time
of 30 days, and then multiplied by 1.1. Then, the maximum of this value and 400 will be
assigned to I inhib thres because it is assumed that this threshold cannot fall below 400 µg.
The graphical function for the effect of capacity on thyroid hormone secretion (eff of
cap on TH sec) is not explicitly shown because it is the same as the ones in the previous
two sectors.
To figure only the amount of T4 secretion out of the total thyroid hormone secretion,
the potential total secretion is multiplied with the fraction of T4 secretion (fr of T4 sec). As
mentioned before, a specific fraction of secretion is reserved for each of the two thyroid
hormones. Normally, this fraction is approximately 93% (90/97) for T4 in the model.
However, it is not a constant and can be altered under certain conditions. The way this
fraction is revised will be elucidated later in this section.
As explained in section 5.3.1, the majority of T3 is obtained via deiodination of T4
molecules. Under normal conditions, the glandular secretion of T3 comprises only 20% of
the total T3 release. So, of the daily 35 µg T3 secretion, 28 µg is acquired through the
conversion of T4 to T3. The outflow named T4 to T3 conv rate serves for this purpose. As
is the fraction of T4 productivity for secretion, the fraction of T4 to be deiodinated is
variable too. The conditions under which this fraction changes will be clarified later in this
section.
Other two outflows from T4 in Blood are conversion rate to rT3 (Conv rate to rT3)
and (Abs rate of T4 by tissues). The values of these flows are computed by multiplying the
current stock value with some constant fraction. Normally, 32 µg of T4 is assumed to be
deiodinated into rT3, which comprises about 36% of the daily T4 secretion. The last
outflow, called T4 clear rate, stands for the rate of (renal) clearance of T4 (with the halflife of 7 days) from the blood.
42
The flows into and from the stock variable for the level of T3 in blood resemble to
those of T4 in blood. There are four flows that influence the level of T3 in blood. The first
inflow to T3 in blood is its secretion rate. T3 secretion rate is formulated in the same
manner as T4 secretion rate. The fraction of secretion for T3 is taken approximately 7%
(7/97) under normal conditions. This fraction may vary under certain circumstances, as
does the fraction of productivity for T4.
The second inflow to T3 in Blood is the rate of deiodination of T4 into T3. The
reason why the related outflow from T4 doesn’t directly enter into T3 in Blood stock is that
some numerical adjustment was required to account for the mass change due to departure
of iodine atoms from T4 molecules in the conversion process. As mentioned in T4 case,
the value of the outflow named Abs rate of T3 by tissues is calculated by multiplying some
coefficient with the stock value. Lastly, T3 clearance rate (T3 clear rate) is the renal
clearance rate of T3 from the blood (with a half-life of 1 day). So, the only difference from
T4 is that T3 in blood does not have an outflow analogous to the rate of conversion of T4
to rT3; all other flows are qualitatively the same as those of T4 in Blood.
As mentioned in detail in section 3.3.1, the thyroid has the capacity to store
appreciable amounts of preformed thyroid hormones. The two stocks in the model, T4
Store and T3 Store, stand for these hormone stores. Normally, these stocks contain two
months’ supply of thyroid hormones. The set point is 5400 µg for T4 store, and 420 µg for
T3 store. The only inflow to these stocks is the synthesis rate of the related hormone. To
determine the synthesis rate of either thyroid hormone, a desired synthesis rate is
calculated at first. The classical stock adjustment formulation is used when constructing
the equation for desired synthesis rate. The associated equations for T3 are shown in
Equations 5.22 - 5.24. The related equations for T4 are of the same form as T3, and
therefore will not be shown explicitly anew.
The first ingredient in desired T3 synthesis is its secretion rate which acts to
replenish the usual daily release rate from the stores. The second term is the stock
adjustment term that helps close the gap between the desired and the current level of the
43
store. So, if the T3 store were valued below the desired level, then this formulation would
not only compensate for the regular daily losses but also for the gap between the normal
and current stock value. Conversely, if the stock levels were sufficiently above the desired
levels, then the adjustment term would take a negative value to facilitate the convergence
to normal stock values.
des T3 syn rate = T3 sec rate + pot T3 store adj
(5.22)
pot T3 store adj = disc from des T3 store / AT for store restor
(5.23)
disc from des T3 store = des T3 store − T3 Store
(5.24)
The desired levels of hormone stores are not constant; they change according to the
changes in the secretory fractions of thyroid hormones. In literature, it is stated that
intrathyroidal fractions of hormone stores are in concordance with the fractional secretion
rates of T3 and T4 from the thyroid when preferential secretion of T3 is the case (Brent,
2010). Thus, the total normal amount of hormone store within the thyroid (5820 μg) is
multiplied by the related secretory fraction to figure the desired level for that hormone
store.
des T4 store = (total normal TH store) × fr of T4 sec
(5.25)
des T3 store = (total normal TH store) × fr of T3 sec
(5.26)
In cases where hormone stores are above their desired level, it is possible for the
desired synthesis rate to take negative values. Though it is conceptually not illogical for a
“desired” quantity to take a negative value, a negative actual synthesis rate is neither
plausible nor possible. In other words, the gland wouldn’t freely discharge its excessive
content just to get rid of it. Hence, when subjecting this desired value to some capacity
constraints, the maximum of this desired value and zero will be taken. Lastly, as mentioned
earlier, the adjustment time for store restoration (AT for store restor) is an indicator of how
fast the gland is thought to be likely to close the gap between the target and current stock
value, and is taken as 30 days here.
44
After the desired synthesis rate is set, it is firstly filtered through some capacity
constraint, as done in the determination of secretion rates of thyroid hormones. This
capacity is an upper bound for synthesis rate of T4 that the thyroid gland is thought to be
capable of, as it was for the secretion rates. One should note that reducing the capacity of
the thyroid only in extremely high concentrations of iodine does not mean that the cases
where the intraglandular quantity of iodine itself doesn’t suffice to meet the requirements
for the synthesis of hormones are ignored. The potential synthesis rate will be further
constrained at the time when the iodine availability is checked. The corresponding set of
equations involved in the calculation of the potential synthesis is depicted below.
pot T3 syn rate = thy syn cap for T3 × eff of thy cap on T3 syn
(5.27)
thy syn cap for T3 = thy cap × fr of T3 sec
(5.28)
eff of thy cap on T3 syn = f (max{des T3 syn , 0} / thy syn cap for T3)
(5.29)
As Equation 5.26 reveals, by multiplying the fraction of T3 secretion with the total
capacity, the relevant portion of thyroidal capacity reserved for T3 synthesis (thy syn cap
for T3) is taken to restrain the (nonnegative) desired amount of T3 synthesis. And, the
nominator of the input to the effect of thyroid capacity on T3 synthesis is taken as the
maximum of the desired T3 synthesis and zero in order to be able to discard negative
synthesis rates. The graphical function for this capacity effect is the same as the others,
and thus not presented over again.
The last step that needs to be taken before deciding on the actual synthesis rates is to
check the iodine availability. If the iodine demand for thyroid hormone synthesis cannot be
fully met, the available amount of iodine is redistributed for the synthesis of two thyroid
hormones not according to the former fractions but rather in favor of T3.
The maintenance of normal levels of T3 in the body is of primary importance for its
being the biologically active form, i.e. the one that is utilized by the cells, of thyroid
hormones. So, the deficiency of T3 becomes more of an issue as compared to that of T4,
45
and necessitates effective balancing mechanisms to guard against life-threatening
situations. Related literature suggests that unless the impairment of thyroid hormone
production is severe, T3 levels in blood remain within normal limits (Werner et al., 2005).
Thus, the measurement of blood T3 levels does not provide differentiating information in
the diagnosis of hypothyroidism.
It is stated that numerous intrathyroidal and extrathyroidal mechanisms act in concert
in order to retain T3 availability. Within the thyroid gland, both the secretion and synthesis
of T3 is favored to T4. Moreover, peripheral conversion of T4 to T3 increases in the
hypothyroid state. So, at the expense of decreasing the circulating T4 concentrations, the
mentioned compensatory mechanisms operate to preserve normal, healthy T3 levels
(Brent, 2010; Werner et al., 2005; Greenstein and Wood, 2011). One of the most common
causes of hypothyroidism is iodine deficiency. So, if an implication of iodine deficiency is
detected during the availability check, synthesis of T3 will be favored. But the point where
iodine availability checked is not the only one where T3 is favored; the preferential T3
synthesis will again become a current issue when the secretory fractions of thyroid
hormones are revised.
After determining the potential synthesis rate, the amount of iodine necessitated is
calculated by simply multiplying that amount with the weight percentage of iodine in T3
molecule. The same procedure that is explained up to this point is applied for determining
T4 synthesis rate too. So, at this point, the total amount of iodine required for total
potential thyroid hormone synthesis is at hand. To check the adequacy of iodine supplies,
the overall amount of necessary iodine is compared to the possible amount. If consumption
of this potential quantity is not fully permitted, the fractions of productivity reserved for
each hormone is revised in favor of T3 to mitigate the vital implications of iodine
deficiency.
The rationale behind the constrained utilization of intraglandular hormone stores is
extrapolated to the consumption of iodine stores too. The first step to examine the
availability of iodine supplies is to send the ratio of the potential iodine consumption (pot
46
total I cons) to the maximum possible amount (pos I cons) to a graphical effect function as
input. The graphical function is the same as the functions that stand for the effect of
hormone store capacities, and thus is not shown explicitly. The maximum possible amount
of daily iodine consumption is presumably set as 15% of the existing intrathyroidal iodine
stock. The value that this function yields is then multiplied with the maximum permissible
amount to obtain the potential iodine consumption under iodine restriction (pot total I cons
under I cap rest), as illustrated in Equation 5.30.
pot total I cons under I cap rest = pos I cons × eff of thy I cap
(5.30)
If the potential iodine consumption lies decently below the maximum tolerable
amount, then all the iodine demanded can be delivered. As the sought quantity approaches
to the limit, the gland tends to act more economical and agrees to give the daily maximum
only when fairly higher quantities are requested. This kind of control on the outflow of the
stock is also implemented in the thyroid hormone stores, as explained before.
Following the determination of accessible quantity of iodine, the synthesis rate
allocated to each hormone is to be revised. For this purpose, the discrepancy between the
synthesis with the permitted amount of iodine and the potential synthesis is calculated.
Then, this discrepancy is divided to the value of potential synthesis rate (ratio of disc btw I
rest TH syn and pot TH syn to pot TH syn). In the model, this ratio is regarded as an
indicator of the severity of iodine deficiency, and thus the potential hypothyroidism. A
graphical effect function is defined that uses this ratio as input (see Figure 5.13).
The decreasing function in Figure 5.13 is used to attenuate the amount that will be
subtracted from the potential T3 synthesis due to iodine availability constraint. If the
preferential synthesis of T3 were not the case, the potential synthesis rates of each
hormone would be multiplied with ratio of cap rest I cons to pot to find the actual
synthesis rates. Since T3 is the critical hormone, in cases where the iodine supply is a
binding constraint, the reduction in T3 synthesis should be relatively smaller than that of
47
T4. The function eff of pref T3 syn on red in T3 syn is created to decrease the quantity that
is subtracted from the potential T3 synthesis rate. Because the value that the function in
Figure 5.13 yields ranges from one to zero, the resultant fraction declines as the
discrepancy increases, i.e. as the consumable quantity of iodine declines.
eff of pref T3 syn on red in T3 syn
1
0.8
0.6
0.4
0.2
0
0
0.2
0.4
0.6
0.8
1
ratio of disc btw I rest TH syn and pot TH syn to pot TH syn
Figure 5.13. Graphical function for the effect of preferential T3 synthesis on reduction in
T3 synthesis.
When correcting the shares of production rates for T3 and T4, two conditions must
be satisfied. First, the synthesis rate of the hormone under iodine restriction should not
exceed its potential synthesis rate. Second, the revised synthesis rate should not go beyond
the total potential synthesis rate. Subtracting some fraction of the discrepancy from the
total potential synthesis rate is enough to satisfy the first condition, but not the second one.
The second situation can happen when the total iodine-constrained synthesis rate is below
the initial one necessitated by T3. The denominator of Equation 5.31 helps hinder this
situation.
The nominator of Equation 5.31 will always be less than or equal to the potential T3
synthesis rate (which is the rate not yet confined to iodine adequacy). And, the
denominator of the equation can take a value greater than one when the second condition
explained above is active. So, as the allowable total synthesis rate approaches to zero, the
48
nominator of the ratio within the maximum operator and the nominator of the equation
tend to cancel out each other. Thereby, the resultant synthesis rate is prevented to exceed
the feasible rate.
T3 syn rate =
pot T3 syn disc btw pot T3 syn and I rest T3 syn eff of pref T3 syn on red in T3 syn
pot T3 syn
max 1,
pot TH syn - disc btw pot TH syn and I rest TH syn
(5.31)
Since T4 is the secondary hormone in the calculations, its synthesis rate is just the
remaining of the total permissible synthesis rate. The related equation is shown below.
T4 syn rate = pot TH syn − disc btw pot TH syn and I rest TH syn − T3 syn rate
(5.32)
One should note that after checking the possible amount, altering the potential
synthesis rates in favor of T3 does not hurt the initial principle of obtaining a feasible
amount of thyroidal iodine to be consumed because less iodine is required for unit T3
synthesis as compared to T4. So, the ultimate amount of iodine expended will always be
less than or equal to the quantity that is found to be feasible after the availability check.
Another mechanism that operates to preserve T3 availability is the adaptability of the
conversion fraction of T4 to T3. To ensure the T3 availability, this fraction increases to
some extent in hypothyroid state. The fraction is adjusted as a function of the circulating
T3 levels relative to its set point. The related graphical effect function is illustrated in
Figure 5.14. As the ratio of currently circulating T3 levels to the normal levels decrease,
the value that the function yields increases and then saturates after some point. This means,
if the T3 level falls below its set point, the rate of conversion rises to compensate for the
gap.
49
eff of T3 conc on peri conv
1.7
1.2
0.8
0.4
0
0
0.2
0.4
0.6
0.8
1
ratio of T3 to normal
Figure 5.14. Graphical function for the effect of T3 concentration on peripheral
conversion.
As mentioned earlier in this section, fractions of T3 and T4 secretion are not
constant. The modifications in these fractions are done in three phases. Firstly, circulating
T3 and T4 levels don’t necessarily differ from their set points with the same proportion.
Thus, it is thought that it wouldn’t be very reasonable to allocate the total secretion rate
regardless of the individual differences from the set points by using just some constant
fractions. For this purpose, the overall thyroidal secretion is distributed inversely
proportional (because thyroid hormones feed back negatively) to the ratio of the related
hormone to its normal value. Equation 5.33 shows how the formulation for this first part is
derived. For ease of demonstration, variable name x is used for the fraction of T3 secretion
not yet undergone the second and third steps.
As mentioned earlier in this section, 7/97 and 90/97 are the normal thyroidal
secretion fractions of T3 and T4, respectively. This first part of the formulation does not
explicitly lead to preferential secretion of T3 in hypothyroid state; it just fairly distributes.
After redistributing the fractions according to the individual deviations of two
hormones from their set points, the second step is to consider the effect of the level of
thyroid stimulation on the fractions. Normally, T3 of thyroidal origin comprises 20% of
50
total T3 production in the body. However, related literature reports that in patients with
thyroid hyperfunction or hypofunction, a relatively higher fraction of the total T3 is
delivered by the thyroid (Laurberg, 1984; Brent, 2008; Brent, 2010). Equation 5.34 shows
the second step in the calculation of fraction of T3 secretion.
7/97
normal ratio of T3 to T4
x
90/97
1 x
ratio of T3 to T4
1
ratio of T3 to T4
1
7
x
normal ratio of T3 to T4
90
(5.33)
7
normal ratio of T3 to T4
90
x
7
ratio of T3 to T4 normal ratio of T3 to T4
90
7
normal ratio of T3 to T4
90
pot fr of T3 sec =
eff of thy stim on T3 fr
7
ratio of T3 to T4 + normal ratio of T3 to T4
90
(5.34)
The findings about preferential synthesis and secretion of T3 in hypothyroid state
were previously mentioned in this section. Besides, it has been documented that in the
thyroids of patients with Graves’ disease, a common source of hyperthyroidism, T3/T4 was
consistently higher and was not due to iodine deficiency (Izumi and Larsen, 1977), and that
thyroidal secretion of T3 rises from approximately 20% to 30% in Graves’ disease (Brent,
2008). The common point for cases where thyroidal secretion of T3 is relatively higher
compared to the normal physiological conditions is that the thyroid is overstimulated.
Depending on the capability of the thyroid, this hyperstimulation may result in
hyperthyroidism or hypothyroidism, but the “potential demand” that the thyroid faces is
51
high in either case. In this respect, the ratio of implied thyroidal secretion to the normal can
be taken as an indicator of stimulation level. But, it is thought that sudden shifts in the
level of thyroid stimulation should not alter these fractions instantaneously; persistence in
hyperstimulation must be sought. Thus, the smoothed version of this ratio rather than its
instantaneous value is allowed to affect these fractions. Smoothing is achieved through a
third order information delay structure with a delay time of 10 days.
eff of thy stim on T3 fr
2.5
2
1.5
1
1
1.5
2
2.5
3
3.5
4
4.5
5
ratio of short smth imp TH sec to normal
Figure 5.15. Graphical function for the effect of thyroid stimulation on T3 secretion
fraction.
Lastly, the fraction of T3 secretion is calculated as a function the potential value for
this fraction. This final step is performed to prevent fr of T3 sec from exceeding the value
one in potential (unrealistically) extreme cases because of multiplication with the
coefficient that the effect of thyroid stimulation yields. The related graphical function is
shown in Figure 5.16.
The above mentioned mechanism directly counts for preferential T3 secretion. In
addition, as aforementioned, the synthesis fractions are also modified in favor of T3 in
cases of iodine deficiency. Hence, when that is the case, T3 stores will surely persist
longer than T4 stores and availability of hormone supplies won’t easily become a binding
constraint on T3 release, which in fact is an indirect reference to preferential secretion too.
52
1
fr of T3 sec
0.98
0.96
0.94
0.92
0.9
0.9
0.92
0.94
0.96
0.98
1
1.02
1.04
1.06
1.08
1.1
pot fr of T3 sec
Figure 5.16. Graphical function for the fraction of T3 secretion.
As the hypothalamus and pituitary do, the thyroid can change its weight under
certain circumstances. The structure related to thyroid weight adjustments functions in the
same manner as in the previous two sectors. So, the stock that stands for the weight of the
thyroid is subjected to a single adjustment flow. This adjustment flow is formulated in the
same way as the adjustment flow of the hypothalamus and pituitary, and thus will not be
explained anew.
5.4. Iodine Sector
5.4.1. Background Information
Iodine is a requisite substrate for the synthesis of thyroid hormones. It is present in
foods usually as iodide, which is the inorganic form of iodine. Iodide is available in the
form of iodized table salt, and also various kinds of food exist which are rich in iodide; e.g.
seafood, kelp, spinach, soybeans, garlic etc. After being ingested, iodide is absorbed nearly
completely in the stomach and duodenum. Related literature suggests that the absorption of
dietary iodide is greater than 90% in healthy adults (Zimmermann, 2009). The absorbed
iodide then diffuses in blood. Iodide is cleared from circulation mainly by the thyroid and
53
kidney. The clearance of circulating iodide by the thyroid is called iodide trapping. Within
the thyroid gland, iodides are converted into an oxidized form of iodine. Once iodides
undergo oxidation process, they are ready to participate in the production of thyroid
hormones (Guyton and Hall, 2006).
Due to its vital role in the functioning of the whole body, the thyroid gland is
equipped with buffers to preserve the healthy state in case thyroid function is somehow
impaired. As mentioned before, the thyroid reserves a considerably large amount of
preformed thyroid hormones in it which is available for secretion on demand. Besides the
hormone stocks, the thyroid gland has a large iodine supply which allows to maintain
thyroid hormone synthesis in lack of iodine intake for some time. That is, in case of
inadequate iodine intake, hormone synthesis persists until the available iodine stores has
been depleted, unless, of course, the thyroid itself dysfunctions. In literature, it is stated
that the normal dietary iodine intake is 150 µg/day, and the amount of intrathyroidal iodine
stores range from 10 to 20 milligrams (Van Vliet and Polak, 2007).
Iodide uptake from the circulation into the thyroid is primarily controlled by TSH
(Guyton and Hall, 2006; Nyström et al., 2011). The rate of iodide trapping by the thyroid is
altered depending on the magnitude of TSH stimulation; if TSH signals increase, amount
of iodide trapped also rises, and if the stimuli decline, iodide trapping diminishes too. In
addition to this, related literature postulates that the thyroid is able to “sense” its iodine
content and adjust its sensitivity to TSH stimulation (Yadav, 2008). So, the intrathyroidal
iodine supply can be autoregulated by an internal feedback mechanism which controls the
intraglandular utilization of iodine and the thyroid response to TSH stimulation (Bhagavan,
2002).
5.4.2. Description of the Structure
The iodine sector is composed of three stocks. Two of these stocks have real physical
counterparts in the body, but the third one serves as an intermediate step in the calculation
of iodide trapping rate. The stock-flow diagram of this sector is depicted in Figure 5.17.
54
I from T3 conv
I from rT3
I from T4 in tissues
retained I
I from T3 in tissues
I from deiod
abs fr of I
I intake
excr fr
Del for trap fr
I in Blood
Pot Trap Fr
I excr
I abs rate
chg in trap fr
gr for eff of
TSH on I trap
Trap rate
gr for eff
of thy wt
on I trap
disc
eff of thy wt
on I trap
eff of TSH on I
trapping
des trap fr
log ratio of
TSH to
normal
I in Thy
gr for des
trap fr
ratio of thy I conc
to normal
normal I in thy
I cons
I cons for T4
I cons for T3
Figure 5.17. Stock-flow diagram of the iodine sector.
As can be seen in Figure 5.17, the stock Iodine in Blood is altered via two inflows
and two outflows. The first inflow to the stock is the absorbed portion of dietary iodine (I
abs rate), and the retained iodine from the deiodination or peripheral catabolism of thyroid
hormones (I from deiod) is the second one. The normal dietary iodine intake is taken as
150 µg and the absorption fraction as 95%. The outflow Excretion of I represents the renal
clearance of plasma iodine, and Trap rate the rate of clearance of iodide by the thyroid.
The thyroid can accommodate itself to the current iodine status of the body. If there
is inadequate iodine intake, then the thyroid traps a higher percentage of iodine, and vice
versa. Since the impact of TSH on synthetic and secretory activities of the thyroid is
55
evident within a short period of time as mentioned earlier, in the model TSH exerts its
effect on iodide trapping rate instantaneously too. But, in case intrathyroidal iodine
concentration is not at its normal, the adaptation of the trapping rate is assumed to occur
with one-day delay. The stock Pot Trap Fr serves for this purpose. First, a desired trapping
fraction is calculated as a function of the ratio of current intrathyroidal iodine content to
the normal (see Figure 5.18). According to this desired fraction, the value of the
adjustment flow to the stock is revised (as in the adjustment flows of gland weights). But,
the value of the stock is some raw value for trapping fraction and is not yet exposed to the
effect of TSH stimuli. Equation 5.35 shows the formulation for trapping rate (Trap rate).
0.5
des trap fr
0.4
0.3
0.2
0.1
0
0
0.5
1
1.5
2
2.5
3
3.5
4
4.5
5
ratio of thy I conc to normal
Figure 5.18. Graphical function for desired trapping fraction.
Trap rate = Pot Trap Fr × I in Blood × eff of TSH on I trap × eff of thy wt on trap cap
(5.35)
According to Equation 5.35, the trapping fraction is either amplified or contracted
depending on the magnitude of TSH stimuli. TSH and intrathyroidal regulatory
mechanisms alter the trapping fraction to a certain extent. In addition to these two factors,
it is stated that the enlargement of the thyroid to raises its capacity to accumulate iodide
from the blood (Rhoades and Bell, 2009). Bearing this in mind, the potential trapping
fraction is further multiplied with an effect function (eff of thy wt on trap cap) that aims at
56
depicting the dependency of trapping capacity on the weight of the thyroid. The graphical
function is depicted in Figure 5.20.
1.4
gr for eff of TSH on I trap
1.2
1
0.8
0.6
0.4
0.2
0
-1
-0.8
-0.6
-0.4
-0.2
-0
0.2
0.4
0.6
0.8
1
log ratio of TSH to normal
Figure 5.19. Graphical function for the effect of TSH on iodide trapping.
gr for eff of thy wt on I trap
1.3
1
0.8
0.6
0.4
0.2
0
0
0.5
1
1.5
2
2.5
3
Thy Wt / normal thy wt
Figure 5.20. Graphical function for the effect of thyroid weight on iodide trapping.
Lastly, the outflow I cons represents the total iodine loss from available stores due to
its usage in thyroid hormone synthesis and is simply the sum of the iodine consumptions
necessitated by T3 synthesis rate and T4 synthesis rate.
57
To summarize this chapter, a simplified stock flow diagram of the whole model is
given in Figure 5.21.
Pit Wt
Hypo Wt
Hypo
wt chg
des hypo
wt
Pit wt
chg
TRH clear fr
des pit wt
hypo cap
TRH
clear rate
eff of TH on
TSH sec
eff of TSH
on TH sec
Thy Wt
Thy
wt chg
des
thy wt
<T4 in Blood>
eff of TH on
TRH sec
<T3 in Blood>
I from
deiod
<pot T3 syn>
fr of T3 sec
des T4
store
<thy cap>
I in Blood
TSH
clear rate
TSH
sec rate
imp TSH sec
eff of TRH
on TSH sec
<I in Thy>
fr of T4 sec
imp
TH sec
thy cap
T4 Store
T4 syn rate
T4 in Blood
Trap rate
pos I cons
I cons
for T3
T4 to T3
conv rate
ratio of cap
rest I cons
to pot
I in Thy
I cons
T4
clear fr
T4 clear
rate
T4 sec rate
pot total I cons
<Thy Wt>
<TSH>
Abs rate
of T4 by
tissues
Conv
rate to
rT3
pot T4 syn
pot TH syn
I abs
rate
pit cap
TSH
TRH
TRH
sec rate
imp TRH sec
I intake
TSH
clear fr
<thy cap> <imp TH sec>
eff of pref
T3 syn on
red in T3 syn
I cons
for T4
pot T3 syn
<T4 syn rate>
<T3 syn rate>
T3 in Blood
T3 Store
T3 syn rate
des T3
store
T3
clear fr
T3 clear
rate
T3 sec rate
<fr of T3 sec>
Abs rate
of T3 by
tissues
<thy cap>
Figure 5.21. Simplified stock-flow diagram of the model.
58
6. VALIDATION AND ANALYSIS OF THE MODEL
Model validation is a procedure to check if the model is able to adequately illustrate
the real problem, as far as the purpose of the modelling study is concerned. Model validity
is tested both in structural and behavioural aspects, structural being of primary importance
in system dynamics models. So, the logical course of model validation is first to test the
validity of the structure, and then begin to check the behaviour accuracy. Structural
validity tests check if the structure of the model is able to satisfactorily reflect the actual
relations that exist in the real system. Once the model succeeds in the structural tests and
sufficient confidence is established in the model structure, behaviour validity tests are
implemented to check if the dynamic behaviours produced by the model can sufficiently
reflect the real patterns of concern (Barlas, 2002; Barlas 1996).
The validity check, especially the structural one, is in fact continuously achieved
during the development of the model, and should not be perceived as a completely isolated
phase. In this study, a significant portion of structural validation has been done during the
process of model construction. It is done by verifying the structure both with the existing
information in literature and through the interviews with medical doctors. The aim of this
chapter is to represent the outputs of the simulations conducted under certain scenarios to
further check the structural validity of the model that is described in the preceding chapter.
The model is simulated using Vensim software. As mentioned before, the time unit
of the model is one day. The time horizon of the simulations is selected long enough to
observe the system behaviour evidently, ranging from a few days to several years. For all
the simulation runs, a sufficiently small time step is selected (DT=1/128).
59
6.1. Equilibrium Behaviour
When all the variables are initially set to their equilibrium (normal) levels, all
0.2
10
0.175
9
micrograms/dL
micrograms/dL
hormones stay constant at their equilibrium values, as expected.
0.15
0.125
7
6
0.1
0
1
2
3
Time (Day)
4
0
5
0.3
3
0.25
2.5
microunits/ml
nanograms/ml
8
0.2
0.15
1
2
3
Time (Day)
4
5
2
1.5
1
0.1
0
1
2
3
Time (Day)
4
5
0
1
2
3
Time (Day)
4
5
Figure 6.1. T3 (left top), T4 (right top), TRH (lower left), and TSH (lower right)
concentrations at equilibrium.
6.2. Base Run
Here, the initial value of T4 in blood is set to three times its normal value (720 µg).
All the other variables are set to their normal values initially.
Firstly, since T4 is above its equilibrium value initially, it gradually decays to restore
the equilibrium value and stabilizes there. It takes a few days for T4 to converge to the
equilibrium value because its half-life is seven days. Secondly, since T3 is largely obtained
via the deiodination of T4, T3 concentration also rises with the initial shift in T4.
60
micrograms/dL
30
22.5
15
7.5
0
0
0.60
1.20
1.80
2.40
Time (Day)
3
3.60
Figure 6.2. T4 concentration in base run.
micrograms/dL
0.4
0.3
0.2
0.1
0
0
0.60
1.20
1.80
2.40
Time (Day)
3
3.60
Figure 6.3. T3 concentration in base run.
microunits/ml
3
2.25
1.5
0.75
0
0
0.60
1.20
1.80
2.40
Time (Day)
3
3.60
Figure 6.4. TSH concentration in base run.
61
Due to the negative feedback effect of thyroid hormones on the release of TRH and
TSH, their concentrations decline too. As thyroid hormones converge to the equilibrium,
TSH and TRH restore their normal levels (see Figure 6.4 and Figure 6.5).
nanograms/ml
0.24
0.18
0.12
0.06
0
0
0.60
1.20
1.80
2.40
Time (Day)
3
3.60
Figure 6.5. TRH concentration in base run.
6.3. TRH Injection Test
In the work of Snyder and Utiger (1972), a TRH stimulation test is performed on six
normal healthy subjects. 25 µg TRH is injected to each of the six subjects at t=0, and blood
samples are collected to measure the TSH levels in blood (see Figure 6.6).
To replicate this test, all the variables are set to their equilibrium levels initially, and
25 µg TRH is assumed to be injected at t=0. For the model output to be comparable to real
data, only the first three-hour portion of the simulation run is displayed in Figure 6.7.
Comparing the two graphs in Figure 6.6 and Figure 6.7, it can be said that the overall
behaviour and even the value of the peak point of TSH from the model highly matches
with those of real data. The time of the hormone to reach its maximum takes somewhat
longer in the model; but since the time unit of the model is one day and relatively longterm dynamics of hormones are the point of interest in this study, this slight difference
does not hurt the validity of the model.
62
Figure 6.6. Average TSH concentration of six normal subjects when 25 µg TRH is injected
at t=0 (Snyder and Utiger, 1972).
microunits/ml
20
15
10
5
0
0
0.019
0.038
0.058 0.077
Time (Day)
0.096
0.115
Figure 6.7. TSH concentration when 25 µg TRH is injected at t=0.
6.4. Ten-Fold Increase in T4 Secretion for One Hour
In literature, it is stated that if T4 secretion were increased ten-fold for one hour, we
would expect the total T4 concentration in blood to increase by 12% (Goodman, 2009).
63
Here, it is assumed that from t=0 to t=1/24, T4 secretion rate is ten times its normal value,
i.e. 900 µg. After t=1/24, no external intervention is applied on T4 secretion. The
behaviour of T4 under this scenario is shown in Figure 6.8.
micrograms/dL
9.5
9
8.5
8
7.5
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.8. T4 concentration when its secretion is increased ten-fold for one hour.
micrograms/dL
0.17
0.165
0.16
0.155
0.15
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.9. T3 concentration when T4 secretion is increased ten-fold for one hour.
Increasing the T4 secretion for one hour causes T4 levels to rise until the end of the
first hour, as expected. The amount of increase in T4 in the model outputs is about 13%
which is quite consistent with the data in literature. Since no component of the system is
64
interfered with after the first day, T4 levels start to decrease thereafter, and reach
equilibrium in about one day.
Under this scenario, it is not only T4 whose value is disturbed from equilibrium. A
significant portion of T3 in the body is formed via conversion of T4 to T3. Because of this,
T3 levels also rise in this case. But after a very short while, it drops to values that are
below the baseline values to compensate for the high circulating T4 and then returns
almost to normal at the end of the first day (see Figure 6.9).
nanograms/ml
0.22
0.195
0.17
0.145
0.12
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.10. TRH concentration when T4 secretion is increased ten-fold for one hour.
microunits/ml
2.5
2
1.5
1
0.5
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.11. TSH concentration when T4 secretion is increased ten-fold for one hour.
65
As a result of negative feedback effect of thyroid hormones on both the
hypothalamus and pituitary, TRH and TSH levels decline. As seen in Figure 6.10 and
Figure 6.11, TRH and TSH levels in the body first decline and then rise so as to enable the
body to restore the equilibrium state.
6.5. Zero T4 Secretion for One Hour
The work of Goodman (2009) suggests that if T4 secretion were stopped for one
hour, we would expect its concentration to decrease by only 1%. So, in this scenario, the
secretion rate of T4 is set to zero for one hour at t=0, and after one hour the model is left to
operate by its own.
micrograms/dL
8.050
8
7.95
7.9
7.85
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.12. T4 concentration when T4 secretion is stopped for one hour.
As the secretion rate of T4 cannot be modulated with the feedback loops for the first
hour, its concentration rises initially inevitably. As the external intervention ceases,
circulating T4 levels quickly restore to normal levels. The lowermost point in T4
concentration shown in Figure 6.12 gives a 1.45% reduction in T4 concentration.
As in the previous scenario, the change in T3 concentration goes parallel with the
change in T4 concentration as the primary source of circulating T3 is the deiodination of
66
T4 to form T3. Since a number of mechanisms work in concert to preserve the T3
availability in body, it starts to rise to values that are above normal and returns to normal
values as T4 stabilizes (see Figure 6.13).
micrograms/dL
0.17
0.169
0.168
0.167
0.166
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.13. T3 concentration when T4 secretion is stopped for one hour.
TRH and TSH concentrations show qualitatively the same behaviour in this scenario.
Thus, only TSH is pictorially shown in Figure 6.14. As expected, TSH initially rises to
compensate for the decline in thyroid hormone levels, and then gradually reaches the
equilibrium.
microunits/ml
2.4
2.345
2.29
2.235
2.18
0
0.20
0.40
0.60 0.80
Time (Day)
1
1.20
1.40
Figure 6.14. TSH concentration when T4 secretion is stopped for one hour.
67
6.6. Hypophysectomy
Hypophysectomy, as stated before, means the complete removal of the pituitary
gland. In reality, a person cannot survive long in the absence of such a critical gland
without any therapeutic intervention. However, for the sake of the validation of the model,
we assume that the person continues to live.
micrograms/dL
0.2
0.15
0.1
0.05
0
0
6
12
18
24 30 36
Time (Day)
42
48
54
60
Figure 6.15. T3 concentration in case of hypophysectomy.
nanograms/ml
2.4
1.8
1.2
0.6
0
0
6
12
18
24 30 36
Time (Day)
42
48
54
60
Figure 6.16. TRH concentration in case of hypophysectomy.
68
Since the pituitary is completely removed, no TSH exists in the body. And since
there is no TSH in the body, only minimal amounts of thyroid hormones are secreted. Low
levels of thyroid hormones in blood cause TRH secretion to rise. However, since the
medium of communication between the hypothalamus and the thyroid gland is no longer
present, thyroid hormones in blood continue to drop. The behaviours of circulating T3 and
T4 in this scenario are qualitatively the same; thus, only that of T3 is shown pictorially in
Figure 6.15.
The work of Smith (1930) suggests that the thyroids of rats start to regress in weight
soon after hypophysectomy, evident in ten days and pronounced in thirty days. The
diminution in the weights of the rat thyroids is observed to be usually about by half or even
more. A similar work conducted by White (1933) investigates the effect of
hypophysectomy on rabbits and shows that the average shrinkage in the thyroids is 30% in
male rabbits, and 20% in females.
21
grams
18.5
16
13.5
11
0
20
40
60
80 100 120 140 160 180 200
Time (Day)
Figure 6.17. Thyroid weight in case of hypophysectomy.
The simulation outputs regarding the thyroid weight is consistent with the findings in
literature explained above. Since low levels of thyroid hormones persist because of the
absence of pituitary gland, the hypothalamus persistently over-functions due to scantiness
of inhibition by thyroid hormones. This, in turn, leads to an increase in the weight of the
69
hypothalamus, which turns out to be about three-fold in our case (see Figure 6.18). The
opposite is seen in thyroid gland. Since no TSH exists in the body, thyroid gland is no
longer stimulated. Due to prolonged “idling”, the gland shrinks (Donovan, 1966; Melmed,
2002). As seen in Figure 6.17, the weight of the thyroid is contracted almost by half. The
time scale of the output graphs for thyroid weight and hypothalamus weight is taken as 200
days in order to be able to evidently depict the changes in the sizes.
130
mg
105
80
55
30
0
20
40
60
80 100 120 140 160 180 200
Time (Day)
Figure 6.18. Hypothalamus weight in case of hypophysectomy.
70
7. THYROID DISORDERS
Once the model is believed to be structurally and behaviourally valid, the last step is
to analyse the model via simulation experiments. In this chapter, the model will be
simulated under some common thyroid-related disorders, and the dynamics of the key
variables will be illustrated.
7.1. Graves’ Disease
Graves’ disease is an autoimmune disease which causes excessive thyroid hormone
production. It affects approximately 0.5% of population and counts for the 50 to 80% of
cases of hyperthyroidism (Bürgi, 2010). This disorder is caused by thyroid-stimulating
immunoglobulins, TSIs, which are proteins that mimic the actions of TSH, bind to the
receptors on thyroid cells and stimulate the production of thyroid hormones. In Graves’
disease, TSH and TRH concentrations are less than normal, and often essentially zero. It is
the negative feedback effect of the elevated concentrations of circulating thyroid hormones
that results in low levels of TRH and TSH. Yet, thyroid hormones cannot feed back to
inhibit excessive TSI stimulation. Thus, despite the scarcity of TRH and TSH,
oversecretion of thyroid hormones persists, for independently acting TSIs continue to
trigger the formation and secretion of thyroid hormones. Due to prolonged overstimulation,
the thyroid enlarges and forms a specific type of goiter, called diffuse toxic goiter (Guyton
and Hall, 2006; Rhoades and Bell, 2009).
In this section, the outputs of two simulation runs will be presented. Firstly, the daily
iodine intake will be assumed normal, i.e. 150 µg. Secondly, the iodine intake will be set to
400 µg/day. In these two cases, the amount of TSIs will be kept at the same level. For the
outputs to be comparable, the horizontal and vertical scales of the graphs will be retained
throughout the two runs (except for the graph of thyroidal iodine).
71
7.1.1. Graves’ Disease with Normal Daily Iodine Intake
Here, the daily iodine intake is set to 150 µg, and the values of all the variables are
initially set to their equilibrium levels.
In this scenario, the thyroid hormone concentrations rise with the stimulatory effect
of TSIs, and persistently stay elevated since the negative feedback loop is interrupted
because of the independently acting agents. However, at approximately halfway of the
simulation run, the thyroid hormones start to drop and stabilize at a level above the normal.
The reason behind this that the TSIs demand more than what the thyroid gland can
synthesize using only the given daily iodine intake. So, consumption rate the iodine
exceeds the rate of uptake which leads to the gradual exhaustion of thyroidal iodine stores.
Yet, the drop in thyroid hormone concentrations is not immediately followed by that. After
the depletion of these stores, the preformed hormone stores are used to meet the residuary
demand of TSIs that the thyroidal synthesis rate cannot fulfil.
micrograms/dL
0.6
0.45
0.3
0.15
0
0
28
56
84
112 140 168 196 224 252 280
Time (Day)
Figure 7.1. T3 concentration in Graves’ disease with normal iodine intake.
Related literature suggests that in hyperthyroid patients taking drugs that block
thyroid hormone synthesis stores of thyroid hormones are more rapidly depleted, and the
therapeutic effect of these drugs may require several weeks to become evident (Carruthers
72
et al., 2000). So, if thyroid hormone synthesis is blocked or reduced for some reason, the
hormone stores are depleted before the severity of the disease attenuates. Consistent with
these findings, when both iodine and preformed hormone stores are exhausted in the
simulation, the thyroid hormones start to decline to a level still higher than normal and
stabilize there.
As an example to the levels of hormones in patients with Graves’ disease, a clinical
case has been illustrated in which a 35-year-old woman with this disease presented with
very high T4 concentration (total T4: 320 nmol/l, normal range: 70–150 nmol/l) and
suppressed serum TSH concentration (<0.05 mU/l, normal range: 0.5–4.0 mU/l) (Nussey
and Whitehead, 2001). Consistent with this case, T4 concentration is rises maximally to
three times the normal value (before being suppressed by the above-mentioned
constraints).
micrograms/dL
28
21
14
7
0
0
28
56
84
112 140 168 196 224 252 280
Time (Day)
Figure 7.2. T4 concentration in Graves’ disease with normal iodine intake.
The amount of iodine in the thyroid in euthyroid individuals is suggested to normally
vary between about 3 and 20 mg. In hyperthyroidism due to Graves’ disease, the amount of
iodine in the thyroid is suggested to be low, rarely above 3 mg (Nyström et al., 2011). As
illustrated in Figure 7.3, the thyroidal iodine drops to very low levels in Graves’ disease (to
about 600 µg).
73
16,000
micrograms
12,000
8,000
4,000
0
0
42
84
126
168
Time (Day)
210
252
Figure 7.3. Iodine in thyroid in Graves’ disease with normal iodine intake.
One characteristic feature of Graves’ disease is that T3/T4 is high compared to
normal physiological conditions. As depicted in Figure 7.4, the ratio of serum T3 to T4
ratio rises above normal value (which is 0.0208 in the model) with the introduction of
TSIs, and climbs further with the increase in TSH and depletion of iodine stores.
0.03
0.0275
0.025
0.0225
0.02
0
42
84
126
168
Time (Day)
210
252
Figure 7.4. T3 to T4 ratio in Graves’ disease with normal iodine intake.
As one might expect, TRH and TSH concentrations fall to very low values because
of the inhibitory effect of elevated thyroid hormones. Since measurement of TRH
concentrations is impossible, only TSH concentrations are available numerically. Albeit so,
74
the output graphs for both TRH and TSH are presented here in order to demonstrate their
general course of behaviour.
nanograms/ml
0.2
0.15
0.1
0.05
0
0
28
56
84
112 140 168 196 224 252 280
Time (Day)
Figure 7.5. TRH concentration in Graves’ disease with normal iodine intake.
In the first phase of the simulation run (when the stores are not yet exhausted), the
minimal value of TSH concentration is approximately 0.028 µU/ml, quite consistent with
the data given above where TSH concentration was found to be <0.05 µU/ml.
microunits/ml
2.4
1.8
1.2
0.6
0
0
28
56
84
112 140 168 196 224 252 280
Time (Day)
Figure 7.6. TSH concentration in Graves’ disease with normal iodine intake.
75
One common finding about Graves’ disease is thyroid gland growth due to
overstimulation (Melmed and Conn, 2005). When the patient with Graves’ disease whose
hormone concentrations were given above was examined, it is realized that she had
moderate diffuse goiter. As Figure 7.7 reveals, the thyroid enlarges to a certain extent in
Graves’ disease (note that the time scale of the graphs for gland weights is longer).
23
grams
22.25
21.5
20.75
20
0
50
100
150 200
Time (Day)
250
300
350
Figure 7.7. Thyroid weight in Graves’ disease with normal iodine intake.
40
mg
36
32
28
24
0
50
100
150
200
Time (Day)
250
300
350
Figure 7.8. Hypothalamus weight in Graves’ disease with normal iodine intake.
Finally, the weights of the hypothalamus and pituitary regress as a result of the low
TRH and high thyroid hormones, respectively. The relative remission in the atrophy results
76
from the relative decrease in thyroid hormones and rise in TRH and TSH following the
hormone store depletion.
30
mg
22.5
15
7.5
0
0
50
100
150
200
Time (Day)
250
300
350
Figure 7.9. Pituitary weight in Graves' disease with normal iodine intake.
7.1.2. Graves’ Disease with Relatively High Daily Iodine Intake
All other things being the same as the previous scenario, the iodine intake is set to
400 µg/day here, and the model is simulated again. This experiment is done to show the
behaviour of the system when the iodine is no longer a binding constraint for the synthesis
of thyroid hormones in Graves’ disease.
For the sake of brevity, not every single output of the previous case will be shown;
only the descriptive ones will be selectively presented in this scenario.
With the increase in daily iodine intake, no shift in thyroid hormone concentrations is
observed in the middle of the run (see Figure 7.10). As implied by the stable behaviour of
T3 throughout the run, the thyroidal iodine stores do not get depleted in this case because
the increased daily iodine intake suffices to meet the demand imposed by the TSIs.
77
micrograms/dL
0.6
0.45
0.3
0.15
0
0
28
56
84
112 140 168 196 224 252 280
Time (Day)
Figure 7.10. T3 concentration in Graves’ disease with relatively high iodine intake.
16,000
micrograms
15,500
15,000
14,500
14,000
0
42
84
126
168
Time (Day)
210
252
Figure 7.11. Iodine in thyroid in Graves’ disease with relatively high iodine intake.
Figure 7.12 shows the ratio of T3 to T4 for this scenario. Because of overstimulation
of the thyroid, the ratio of T3 to T4 is higher than normal in this case too. As opposed to
the previous case, no further shift can be witnessed here because TSH levels do not show a
relative increase and thus do not cause the ratio to grow any further.
As depicted in Figure 7.13, TSH concentration ultimately stabilizes at a subnormal
level (0.028 µU/ml).
78
0.03
0.0275
0.025
0.0225
0.02
0
42
84
126
168
Time (Day)
210
252
Figure 7.12. T3 to T4 ratio in Graves’ disease with relatively high iodine intake.
microunits/ml
2.5
1.875
1.25
0.625
0
0
50
100
150
200
Time (Day)
250
300
350
Figure 7.13. TSH concentration in Graves’ disease with relatively high iodine intake.
Finally, the weights of the thyroid and pituitary are depicted in Figure 7.14 and
Figure 7.15. The time scales of these graphs are again longer than the previous ones (the
same as the time scales of the graphs of gland weights in the previous section) in order to
be able to depict the complete behaviour evidently. The convergence of the thyroid to the
ultimate value is smoother in this case. As for the pituitary, no remission in the atrophy can
be observed since no change in neither the thyroid hormones nor TRH occurs once they
stabilize.
79
To summarize, it can be said that the availability of iodine may well augment the
severity of Graves’ disease depending on the amount of TSIs.
23
grams
22.25
21.5
20.75
20
0
50
100
150 200
Time (Day)
250
300
350
Figure 7.14. Thyroid weight in Graves’ disease with relatively high iodine intake.
30
mg
22.5
15
7.5
0
0
50
100
150
200
Time (Day)
250
300
350
Figure 7.15. Pituitary weight in Graves’ disease with relatively high iodine intake.
7.2. Iodine Deficiency
Iodine deficiency is a common cause of hypothyroidism. Though eradicated in many
regions of the world with salt iodization, it still is one prevailing cause of hypothyroidism.
80
Approximately 30% of the world population is encountered with iodine deficiency, about
half of them with goiter (Goldman and Hatch, 2000).
Lack of iodine, which is an indispensable ingredient for thyroid hormone synthesis
as mentioned earlier, hinders the production of thyroid hormones. Consequently, since no
or little thyroid hormone is available to inhibit the production of TSH, excessive amounts
of TSH is secreted. Excessive TSH overstimulates the thyroid gland. But, because of
scarcity of iodide, formation of T3 and T4 does not occur and consequently TSH secretion
cannot be suppressed. In the long run, since the overstimulation by TSH lingers, the
thyroid gland grows larger. Enlarged thyroid gland due to iodine deficiency is called
endemic colloid goiter (Guyton and Hall, 2006).
In this section, the outputs of two simulation runs will be presented; severe iodine
deficiency and moderate iodine deficiency. In the first case, the daily iodine intake will
assumed to be 30 µg. And in the second case, the iodine intake will be increased to 50
µg/day. In both cases, the model is run for 800 days. For the outputs to be comparable, the
horizontal and vertical scales of the graphs will be retained throughout the two runs.
7.2.1. Severe Iodine Deficiency
Here, the daily iodine intake is set to 30 µg by leaving all the other variables at their
normal values initially.
In the initial phase of the run, the concentrations of hormones persevere at their
normal equilibrium levels since the body utilizes the iodine and hormone stores before the
implications of iodine deficiency become apparent. Except for thyroidal iodine, variables
stay at their set-points for a long while. To be able to explicitly demonstrate the dynamics
of the variables, the interval from t=350 to t=750 will be shown in all the output graphs but
the thyroidal iodine.
81
micrograms/dL
0.27
0.23
0.19
0.15
0.11
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.16. T3 concentration when daily iodine intake is 30 µg.
micrograms/dL
10
7.5
5
2.5
0
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.17. T4 concentration when daily iodine intake is 30 µg.
Evidence in literature suggests that serum thyroid hormone levels change in a
characteristic pattern with iodine deficiency, typically showing a low T4 and a normal or
increased serum T3 concentration (Braverman, 2003). It is stated that T3 concentrations
also decline, but not until hypothyroidism, or the iodine deficiency is severe (Werner et al.,
2005; Brent, 2010). In this case, i.e. when iodine intake is 30 µg/day, the body fails to
maintain the serum T3 levels at normal levels. When the equilibrium state is disturbed with
the depletion of iodine and then hormone stores, T3 levels rise above the normal levels for
82
a short while but cannot survive there with the given level of iodide. So, it falls to a
subnormal level and stabilizes there (see Figure 7.16).
As mentioned above, the impact of iodine deficiency on T4 concentrations is more
drastic. The proportional decrease in T4 is much more than that of T3 (see Figure 7.16 and
Figure 7.17). As a consequence, the ratio of serum T3 to T4 is elevated in iodine
deficiency (see Figure 7.18).
0.16
0.12
0.08
0.04
0
350
410
470
530
590
Time (Day)
650
710
Figure 7.18. T3 to T4 ratio when daily iodine intake is 30 µg.
15,000
micrograms
11,250
7,500
3,750
0
0
100
200
300 400 500
Time (Day)
600
700
Figure 7.19. Iodine in thyroid when daily iodine intake is 30 µg.
83
If iodine intake diminishes, hormone secretion remains constant until available stores
of the mineral are depleted (Garrison and Somer, 1995). Consistent with this statement, in
the model, the effects of iodine deficiency become apparent shortly after the depletion of
these stores. The time lag between the depletion of iodine stores results from the fact that
the thyroid makes use of the preformed hormone stores, and is able to release sufficient
amount of thyroid hormones in that interval before a significant portion of these stores are
consumed. Figure 7.19 depicts the dynamics of thyroidal iodine (note that the horizontal
scale begins from t=0).
440
micrograms
360
280
200
120
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.20. T3 store when daily iodine intake is 30 µg.
6,000
micrograms
4,500
3,000
1,500
0
350
410
470
530
590
Time (Day)
650
710
Figure 7.21. T4 store when daily iodine intake is 30 µg.
84
As mentioned before, both the synthesis and secretion of T3 is favoured in
hypothyroid state. Hence, the degree of diminution in T3 reserves is less severe than that of
T4 (see Figure 7.20 and Figure 7.21). One should note that the decrease in hormone stores
shows itself after thyroidal iodine is considerably emptied.
microunits/ml
24
18
12
6
0
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.22. TSH concentration when daily iodine intake is 30 µg.
62
grams
51
40
29
18
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.23. Thyroid weight when daily iodine intake is 30 µg.
As the nature of the negative feedback necessitates, TSH concentrations rise in
parallel with the diminishment in thyroid hormones, as presented in Figure 7.22. Since the
85
behaviour of TRH is qualitatively the same as that of TSH, the related output graph is not
shown separately in this case.
The last thing to mention is the alterations in the weights of the glands. The thyroid
gland starts to be stimulated more than normally when the thyroid hormone levels drop and
TSH levels rise subsequently. As seen in Figure 7.23, the weight of the thyroid increases to
about three times its normal weight.
44
mg
42.75
41.5
40.25
39
350
410
470
530
590
Time (Day)
650
710
Figure 7.24. Hypothalamus weight when daily iodine intake is 30 µg.
48
mg
41
34
27
20
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.25. Pituitary weight when daily iodine intake is 30 µg.
86
In parallel with the persistent drop in thyroid hormones and rise in TRH and TSH,
both the hypothalamus and the pituitary also grow in size (see Figure 7.24 and Figure
7.25).
7.2.2. Moderate Iodine Deficiency
In this case, the daily iodine intake is set to 50 µg. Again, for the sake of brevity, not
all the outputs shown in the severe deficiency case, but only some descriptive ones will be
selected and presented.
micrograms/dL
0.27
0.23
0.19
0.15
0.11
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.26. T3 concentration when daily iodine intake is 50 µg.
micrograms/dL
10
7.5
5
2.5
0
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.27. T4 concentration when daily iodine intake is 50 µg.
87
It was previously explained that unless the iodine deficiency is severe, the
characteristic pattern of serum thyroid hormones is normal or elevated T3, and low T4
concentrations. In the case where iodine intake was 30 µg/day, T3 levels couldn’t hold on
to the normal levels and dropped below the set point. Here however, since the deficiency is
not as severe, T3 succeeds to stabilize at a level above the normal. The diminution in the
severity is reflected to T4 concentration too; it becomes stable at a level higher than the
previous case.
0.16
0.12
0.08
0.04
0
350
410
470
530
590
Time (Day)
650
710
Figure 7.28. T3 to T4 ratio when daily iodine intake is 50 µg.
Though milder than the previous case, 50 µg iodine intake is still inadequate and
causes insufficient synthesis and secretion of thyroid hormones. So, the hypothyroid state
still exists and therefore T3/T4 is higher than normal in this case. As can be observed in
Figure 7.28, this ratio starts to rise with the decrease in thyroid hormone concentrations but
stabilizes at a point which is smaller than the one in the 50 µg-case. So, it can be said that
this ratio is proportional to the severity of the deficiency.
Another important thing to note is that the implications of the deficiency become
evident later than the previous case for the relatively higher intake of iodine helps the preexisting stores to bear longer here. Also, the hormone stores equilibrate at a higher level as
compared to the previous case (see Figure 7.29).
88
440
micrograms
360
280
200
120
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.29. T3 store when daily iodine intake is 50 µg.
Upon the depletion of hormone stores, TSH concentration starts to rise to
compensate for the thyroid hormone deficiency (see Figure 7.30).
6,000
micrograms
4,500
3,000
1,500
0
350
410
470
530
590
Time (Day)
650
710
Figure 7.30. TSH concentration when daily iodine intake is 50 µg.
The behaviours of the weights of the glands are basically the same as in the previous
case; the only difference is that they stabilize at a lower level in this case. As a
representative one, only the graph for thyroid weight is shown in Figure 7.31.
89
62
grams
51
40
29
18
350 390 430 470 510 550 590 630 670 710 750
Time (Day)
Figure 7.31. Thyroid weight when daily iodine intake is 50 µg.
7.3. Iodine Excess
As mentioned earlier, sufficient iodine intake is crucial for the maintenance of
healthy thyroid functioning and severe iodine deficiency obstruct thyroid hormone
production and induces goiter formation. Interestingly, functioning of the thyroid is also
impaired when the dietary iodine intake is far above the physiological needs.
It is postulated that identical iodine excess may cause hyperthyroidism in some
persons and hypothyroidism in others (Bürgi, 2010). Iodine-induced hyperthyroidism is
suggested to happen often due to the autonomy in thyroid function, because of some
therapeutic intervention for some pre-existing thyroid disease, or as a result of the disease
itself. In this study, the effects of iodine excess on thyroids with prior pathological
conditions are considered out of scope; only the impacts on normal thyroids will be of
interest.
A number of studies are conducted to demonstrate the inhibitory effect of excessive
iodine intake on thyroids of healthy subjects, as mentioned before. In one of such studies,
Namba et al. (1993) investigate the effect of 27 mg iodine administration to ten normal
male volunteers on thyroid function and volume. Thyroid volume was measured before
90
treatment, on the day of the last treatment, and 1 month after the treatment. It is found that
there was a significant rise in serum TSH levels, with a small decline in serum free T4
concentration during iodide administration; the values remained within the normal range
except for two subjects. The volume of the thyroid gland is found to be significantly
enlarged after 28 days of iodide intake. And it is stated that when iodide was discontinued,
thyroid volume and function returned to baseline levels within one month for all subjects.
Here, it is assumed that 27 mg iodine is supplemented for 28 days starting at t=0. As
in all the previous scenarios, the variables are initially set to their equilibrium levels. For
the model outputs to be comparable to real data graphs, the model is simulated for 56 days.
Figure 7.32. Average free T4 concentration of ten subjects receiving 27 mg iodine
supplementation for 28 days (Namba et al., 1993).
The average free T4 levels of the ten subjects are depicted in Figure 7.34. T4 levels
decline after the introduction of excessive iodine supplementation and start to rise soon
before the withdrawal of the iodine supplementation. The dynamics of free T4 in the
simulation run is demonstrated in Figure 7.33 and is highly consistent with that of the real
data (note that the horizontal scales do not linearly increase).
91
Figure 7.33. Free T4 concentration (in pmol/l) in case of 27 mg iodine supplementation for
28 days.
micrograms/dL
0.19
0.1775
0.165
0.1525
0.14
0
8
16
24
32
Time (Day)
40
48
56
Figure 7.34. T3 concentration in case of 27 mg iodine supplementation for 28 days.
The behaviour of T3 is shown in Figure 7.34. As opposed to T4, the rising trend in
T3 concentration becomes apparent in T3 after about t=7. The early improvement of T3 is
a consequence of the mechanisms that operate to preserve T3 availability in body. These
mechanisms even lead to elevated T3 levels transiently, to compensate for the subnormal
levels of T4. So, consistent with the findings of Namba et al., the concentrations of both
T3 and T4 return to normal within one month after the discontinuation of iodine
supplementation.
92
Figure 7.35. Average TSH concentration of ten subjects receiving 27 mg iodine
supplementation for 28 days (Namba et al., 1993).
Figure 7.36. TSH concentration in case of 27 mg iodine supplementation for 28 days.
In concordance with the lowered levels of thyroid hormones, the average TSH
concentration of the subjects increases (see Figure 7.35), and restores the normal level
within one month after the excessive iodine intake is stopped. The model output shown in
Figure 7.36 matches well with the dynamics of the real data (note that the horizontal scales
do not linearly increase). The maximum level that the average TSH of the subjects reaches
93
is about 2-2.5 times the normal levels, whereas that of the simulation model is a bit higher,
about three times the normal level.
It was mentioned earlier that the changes in the weight of the thyroid will be
presumably accompanied by the changes in the volume of the thyroid. The average thyroid
volume of ten subjects measured before, during and one month after the supplementation is
shown in Figure 7.37. Since only three data points are available, the data is not exactly
comparable to the model output.
Though not significantly different, the average thyroid volume of the ten subjects is
slightly higher than the volume before the supplementation. In our simulation run, the
weight of the thyroid gland does not restore to normal as much as the average thyroid
volume of the subjects does after one month (at t=56), but it does so in about three to four
months (which is not explicitly shown here).
Figure 7.37. Average thyroid volume (as % of normal volume) of ten subjects receiving 27
mg iodine supplementation for 28 days (Namba et al., 1993).
94
25
grams
23.5
22
20.5
19
0
8
16
24
32
Time (Day)
40
48
56
Figure 7.38. Thyroid weight in case of 27 mg iodine supplementation for 28 days.
Lastly, serum iodine levels of the subjects remain elevated until the iodine
supplementation is discontinued. After the cessation of excessive iodine intake (day 28),
the serum iodine starts to drop. The related data and simulation output are depicted in
Figure 7.39 and Figure 7.40. The units of the real data and the model output are different;
but the overall dynamics of the two match well.
Figure 7.39. Average serum iodine levels of ten subjects receiving 27 mg iodine
supplementation for 28 days (Namba et al., 1993).
95
Figure 7.40. Iodine in blood in case of 27 mg iodine supplementation for 28 days.
7.4. Subacute Thyroiditis
The term thyroiditis refers to the inflammation of the thyroid gland. Inflammation is
the response of tissues to harmful stimuli, and can be caused by viral infections or
autoimmune processes. Here, we are not interested in the causes of the inflammation, but
rather in the consequences of it.
Inflamed cells of the thyroid lose their secretory and synthetic abilities. Moreover,
the inflammatory reaction within the gland causes the follicles to lose their integrity by
disrupting them and results in the release of preformed hormones and iodine into the
peripheral circulation (Grossman, 1998, Werner et al., 2005). The release of the preformed
hormones is not a controlled discharge like the secretion process, but rather a leakage.
The inflammatory reaction in the thyroid gland might be temporary or persistent. In
this section, an instance of temporary thyroiditis, namely subacute thyroiditis, will be of
interest. Subacute thyroiditis is the most common reason of the painful thyroid gland and
may account for up to 5% of clinical thyroid abnormalities. In subacute thyroiditis, the
thyroid gland is exposed to a transient course of inflammation, which usually lasts several
weeks and then ameliorates.
96
Subacute thyroiditis demonstrates a triphasic clinical course of thyrotoxicosis,
hypothyroidism and restoration of normal thyroid functioning. Thyrotoxicosis, which
means an excess of thyroid hormones in the body, is a result of destruction of thyroid cells
and uncontrolled release of hormone stores into the circulation. Since thyroid cells cannot
synthesize hormones during the inflammation phase and leakage of preformed hormones
persist due to inflammation, hormone stores get depleted after some time. As a result,
hypothyroidism is observed. As the name suggests, hypothyroidism is a condition in which
too little thyroid hormone is circulating throughout the body. After the inflammation
subsides, levels of circulating hormones restore their normal levels and hormone stores are
replenished gradually (Van den Berghe, 2008; Grossman, 1998).
In the model, the notion of inflammation is quantified by using a stock which is
allowed to vary between zero and one. The name of that stock is Inflammation Status.
Inflammation Status being one means that the gland is completely inflamed, and being zero
means that the gland is functioning properly. In a sense, this variable gives the inflamed
proportion of the gland.
In this case, two separate sources of thyroid hormone release exist; secretion by the
normally functioning cells, and leakage from the inflamed cells. Having defined the
inflammation status stock as the percentage of dysfunctioning gland, some distinction will
be made for the utilization of hormone stores for secretion and leakage purposes. If some
portion of the thyroid is inflamed, then that portion should leak out thyroid hormones
according to the amount of preformed thyroid hormones covered by that portion, but not
secrete any because it is not capable of doing it yet. Conversely, recovered or healthy
portion of the gland should only be in charge of secreting, not leaking, and be allowed to
consume the amount of preformed hormones that they “own”. For this purpose, three new
stocks are defined in the model; two of them for the thyroid hormones, and one for
thyroidal iodine. For all three substructures, the rationale behind is the same. To begin with
the thyroid hormones, these stocks serve as the amount of hormone stores that the inflamed
portion of the gland encapsulates. And, the old stocks for hormone stores stand for the
amount of hormone stores enveloped by the recovered portion. Two things count for the
97
loss from the new stocks; one is the leakage of hormones, the other is the transition from
the coverage area of inflamed cells to the healthy ones with the recovery of those inflamed
cells. The modified portion of stock flow diagram and related equations for T3 are shown
in Figure 7.41.
Recov of
T4 cont
portion
Leaking T4
Store
Conv
rate to
rT3
T4 Store
T4 syn rate
T4 leak
Abs rate
of T4 by
tissues
T4 in Blood
T4 clear rate
T4 sec rate
T4 to T3
conv rate
Recov rate
Inflammation
Status
T3 from
deiod of
T4
T3 Store
T3 in Blood
T3 clear rate
Abs
rate of
T3 by
tissues
T3 sec rate
T3 syn rate
Recov of
T3 cont
portion
Leaking T3
Store
T3 leak
Figure 7.41. Modified structure of thyroid sector for subacute thyroiditis.
Recov of T3 cont portion = Leaking T4 Store × Recov rate
(7.1)
T3 leak = Leaking T3 Store × 0.02
(7.2)
98
As the above equations reveal, a certain fraction of preformed hormones that are
covered by the inflamed portion of cells leak out of the gland into the circulation, and some
fraction of preformed hormones flows into the regular hormone store stock with the
recovery of inflamed cells. Also, since only healthy cells are capable of synthesizing, the
newly synthesized thyroid hormones flow into the regular hormone store and do not get
mixed with the hormones enclosed by the inflamed portion.
I from
deiod I excr
I in Blood
I abs rate
I leak
Trap
rate
Leaking I
Recov rate
Inflammation
Status
I in Thy
Recov of cells
I cons
Figure 7.42. Modified structure of iodine sector for subacute thyroiditis.
The iodine sector is modified in the same manner as explained above so as to
distinguish the portion of intrathyroidal iodine that is to be consumed for synthetic
purposes and that leaks out of the gland into the blood. The old stock for the thyroidal
99
iodine stands for the amount of iodine to be consumed in a controlled manner, and the new
one for iodine enclosed by the inflamed cells (see Figure 7.42).
There are few last remarks that have to be mentioned to fully elucidate the revised
structure of the model under subacute thyroiditis. Firstly, the stock for thyroid weight (Thy
Wt) represents not the whole but the properly functioning part of the gland (i.e. not
exposed to inflammatory reaction). Secondly, it is assumed that the gland cannot expand in
size during the course of the simulation run. Having zeroed the weight adjustments in the
thyroid, the only inflow to Thy Wt becomes the recovery of the inflamed portions of the
gland (Recov of inflamed thy).
Recov of inflamed thy = 20 × Recov rate
(7.3)
Since the gland is completely inflamed at the beginning, the normal weight of the
thyroid is multiplied with the rate of recovery of inflammation to figure the correspondent
recovery in thyroid weight (see Equation 7.3). Thirdly, the capacity of one unit weight of
the properly functioning part of the gland is taken as one fourth of the normal capacity, i.e.
2.5 times the normal productivity level. The second and third assumptions are related to
the idea that the cells that newly recover from the inflammatory reaction may not perform
as well as in the healthy state, at least over the course of the simulation run. Lastly, the
effect of iodine on thyroid capacity is not taken into account in this case because the
presumed mechanism of impairment for iodine in healthy subjects may not be the same in
an inflamed gland.
Having done all the modifications in model structure and parameters, the model is
run for 150 days assuming a course of inflammation status as depicted in Figure 7.43. The
simulation output showing the TSH and T4 concentrations are shown in Figure 7.44.
Figure 7.45 and Figure 7.46 shows the real data from patients with subacute thyroiditis.
100
1
0.75
0.5
0.25
0
0
20
40
60
80
100
Time (Day)
120
140
Figure 7.43. The assumed course of inflammation status in subacute thyroiditis.
20
10
10
5
0
0
0
20
40
60
80
100
Time (Day)
120
140
TSH conc : Current
T4 conc : Current
Figure 7.44. TSH and T4 concentrations in subacute thyroiditis.
The curves depicting FTI and TSH levels in Figure 7.45 are the ones that we
basically compare our results to. The curve showing TG levels is commonly used as an
indicator for thyroid damage. TG being high implies that the thyroid gland is damaged
(Rubin, 2006). In this case, it returns to normal range (shaded region) near the end of the
time horizon. This is consistent with our presumed Inflammation Status for this case. FTI
is an indicator of free T4 levels in blood, but not the direct amount of it. In the model
output shown in Figure 7.44, the total T4 level is shown. Since the real data uses a
101
different measure for T4 levels in blood, the output of out model is numerically not
comparable to the real data. In subacute thyroiditis, not the behaviour or the course, but the
levels of hormones may show variability from patient to patient. So, even if the units did
match, it would not be very reasonable to try to exactly match to the data points of only
one patient. And, since the ultimate aim of this study is not point prediction, it can be said
that the model gives reasonable results by matching the typical dynamical behaviour.
Figure 7.45. Data from a patient with subacute thyroiditis (Lazarus, 2009).
6
5
TSH
4
3
2
1
0
FT4
1.8
1.6
1.4
1.2
1
0.8
0.6
0.4
0.2
0
Figure 7.46. Data from a patient with subacute thyroiditis (secondary axis: TSH).
102
The name FT4 in Figure 7.46 refers to the free T4 concentration. Though not as
obvious as the data shown in Figure 7.45, the overall course of behaviour that TSH and
FT4 follows is essentially the same. The patient first presents with very low TSH and
elevated FT4 values. With the decline in FT4 concentrations, TSH rises and then stabilizes
(except for the last data point) at a normal level.
Lastly, the work of Werner et al. (2005) states that in the thyrotoxic phase of
subacute thyroiditis, the T3 to T4 ratio is lower than in Graves' thyrotoxicosis. Since the
reason behind the thyrotoxic phase is the uncontrolled leakage of preformed hormones, the
effect of thyroidal stimulation on the preferential secretion of T3 is non-existent in this
case. Therefore, the ratio of T3 to T4 is lower in the thyrotoxic phase of subacute
thyroiditis, as can be seen in Figure 7.47.
0.03
0.0275
0.025
0.0225
0.02
0
20
40
60
80 100
Time (Day)
120
140
Figure 7.47. T3 to T4 ratio in subacute thyroiditis.
103
8. CONCLUSION
In this study, a model for the thyroid hormone dynamics is constructed. Thyroid
hormones are the primary regulators of metabolic functions in the body, and disorders
related to thyroid hormone system are commonly seen. The aim of this study is first to
model the dynamics of the thyroid hormones and the stimulating hormones in healthy
body, then to adapt the model to portray some common abnormalities/disorders, finally to
capture the characteristic dynamics of the hormones involved under these circumstances
and to provide a platform to test possible scenarios.
For model validation, standard model structure and behaviour validity tests have
been applied. In this study, validity tests are illustrated by four runs to demonstrate the
consistency of the model outputs with the information in literature. First, the equilibrium
behaviour is shown to depict the equilibrium state in the body under normal conditions.
Then, the equilibrium state is disturbed with the administration of TRH and the outputs are
compared to the real data. Thereafter, the model is run under two scenarios where the
secretion rate of T4 is increased ten-fold and zeroed for one hour. The outputs are highly
consistent with the numerical data suggested by the related literature. Finally, the effects of
hypophysectomy, the complete removal of the pituitary gland, are shown. The behaviour
of the model under all these scenarios reasonably matches the qualitative and quantitative
data in literature.
After the validation tests, four different conditions related to the thyroid are
addressed. Firstly, Graves’ disease, the most common cause of hyperthyroidism, is
addressed in two different levels of iodine intake. In Graves’ disease; the formation of
goiter, effect of iodine availability on the severity of the disease, and other typical changes
in hormones and glands are well mimicked by the model. Increased T3/T4, which is often
used as a diagnostic criterion in Graves’ disease, is also captured by the simulations.
Secondly, iodine deficiency, one prevailing cause of hypothyroidism, is discussed for two
104
different levels of daily iodine intake. The model was able to depict all the characteristic
changes including the goiter formation and increase in T3/T4 in these two scenarios, both
independently and comparatively. Thirdly, the transient inhibitory effect of excessive
iodine intake on thyroid gland is discussed. The increase in thyroid volume and the mild
decline in thyroid hormones are captured well. Lastly, a disorder called subacute
thyroiditis is analysed. Subacute thyroiditis is a common disorder in which thyroid gland is
exposed to inflammation. The model is shown to reproduce well the behaviour of
hormones during the typical triphasic clinical course of subacute thyroiditis, composed of
thyrotoxicosis, hypothyroidism and normal thyroid functioning.
As far as the information in literature and interviews with the medical doctors are
concerned, the model structure exhibits a reasonable degree of validity. As future work,
more real data can be collected, parameters can be adjusted to reflect more precisely
quantitative and qualitative real data, and some extensions in the model structure can be
done to be able to model medical interventions and drug therapy.
105
APPENDIX: MODEL EQUATIONS
abs fr of I = 0.95 {dimensionless}
Abs rate of T3 by tissues = T3 in Blood × (35 − 5 × LN(2)) / 5 {µg / day}
Abs rate of T4 by tissues = T4 in Blood × ((5334 − 7440 × LN(2)) / 217) / 240 {µg / day}
AT for store restor = 30 {day}
chg in trap fr = disc / del for trapping fr {dimensionless}
Conv rate to rT3 = T4 in Blood × 32 / 240 {µg / day}
del for trapping fr = 1 {day}
des hypo wt = normal hypo wt × eff of imp TRH sec on hypo wt {mg}
des pit wt = normal pit wt × eff of imp TSH sec on pit wt {mg}
des T3 store = total normal TH store × fr of T3 sec {µg}
des T3 syn = T3 sec rate + T3 store adj {µg / day}
des T4 store = total normal TH store × fr of T4 sec {µg}
des T4 syn = T4 sec rate + T4 store adj {µg / day}
des thy wt = normal thy wt × eff of imp TH sec on thy wt {g}
des trap fr = LOOKUP EXTRAPOLATE(gr for des trap fr, ratio of thy I conc to normal)
{dimensionless}
disc = des trap fr − Pot Trap Fr {dimensionless}
disc btw pot T3 syn and I rest T3 syn = pot T3 syn × (1 − ratio of cap rest I cons to pot)
{µg / day}
disc btw pot TH syn and I rest TH syn = pot TH syn × (1 − ratio of cap rest I cons to pot)
{µg / day}
disc from des T3 store = des T3 store − T3 Store {µg}
disc from des T4 store = des T4 store − T4 Store {µg}
eff of cap on TH sec = LOOKUP EXTRAPOLATE(gr for thy cap, ratio of imp TH sec to
thy cap) {dimensionless}
eff of cap on TRH sec = LOOKUP EXTRAPOLATE(gr for hypo cap, ratio of imp TRH
sec to hypo cap) {dimensionless}
106
eff of cap on TSH sec = LOOKUP EXTRAPOLATE(gr for pit cap, ratio of imp TSH sec
to pit cap) {dimensionless}
eff of I on thy cap = LOOKUP EXTRAPOLATE(gr for eff of I on thy cap, ratio of I in thy
to thres) {dimensionless}
eff of imp TH sec on thy wt = LOOKUP EXTRAPOLATE(gr for imp TH sec on thy wt,
ratio of smth imp TH sec to normal) {dimensionless}
eff of imp TRH sec on hypo wt = LOOKUP EXTRAPOLATE(gr for eff of imp TRH sec
on hypo wt, ratio of smth imp TRH sec to normal) {dimensionless}
eff of imp TSH sec on pit wt = LOOKUP EXTRAPOLATE(gr for eff of imp TSH sec on
pit wt, ratio of smth imp TSH sec to normal) {dimensionless}
eff of pref T3 syn on red in T3 syn = LOOKUP EXTRAPOLATE(gr for eff of pref T3 syn
on red in T3 syn, ratio of disc btw I rest TH syn and pot TH syn to pot TH syn)
{dimensionless}
eff of T3 conc on peri conv = LOOKUP EXTRAPOLATE(gr for eff of T3 on peri conv,
ratio of T3 to normal) {dimensionless}
eff of T3 store cap = LOOKUP EXTRAPOLATE(gr for eff of TH store cap, ratio of pos to
pot T3 sec) {dimensionless}
eff of T4 store cap = LOOKUP EXTRAPOLATE(gr for eff of TH store cap, ratio of pos to
pot T4 sec) {dimensionless}
eff of TH on TRH sec = LOOKUP EXTRAPOLATE(gr for eff of TH on TRH sec, log
ratio of TH to normal) {dimensionless}
eff of TH on TSH sec = LOOKUP EXTRAPOLATE(gr for eff of TH on TSH sec, log
ratio of TH to normal) {dimensionless}
eff of thy cap on T3 syn = LOOKUP EXTRAPOLATE(gr for thy cap, ratio of des T3 syn
to cap) {dimensionless}
eff of thy cap on T4 syn = LOOKUP EXTRAPOLATE(gr for thy cap, ratio of des T4 syn
to cap) {dimensionless}
eff of thy I cap = LOOKUP EXTRAPOLATE(gr for I store cap, ratio of pot to pos I cons)
{dimensionless}
107
eff of thy stim on T3 fr = LOOKUP EXTRAPOLATE(gr for eff of thy stim on TH fr, ratio
of short smth imp TH sec to normal) {dimensionless}
eff of thy wt on I trap = LOOKUP EXTRAPOLATE(gr for eff of thy wt on I trap, Thy Wt
/ 20) {dimensionless}
eff of TRH on TSH sec = LOOKUP EXTRAPOLATE(gr for eff of TRH on TSH sec, log
ratio of TRH to normal) {dimensionless}
eff of TSH on I trapping = LOOKUP EXTRAPOLATE(gr for eff of TSH on I trap, log
ratio of TSH to normal) {dimensionless}
eff of TSH on TH sec = LOOKUP EXTRAPOLATE(gr for eff of TSH on TH sec, log
ratio of TSH to normal) {dimensionless}
excr fr = 103.358 / 150 {1 / day}
fr of T3 sec = LOOKUP EXTRAPOLATE(gr for T3 sec fr, pot fr of T3 sec)
{dimensionless}
fr of T4 sec = 1 − pot fr of T3 sec{dimensionless}
free T3 in blood = 0.003 × T3 in Blood {µg}
free T4 in blood = T4 in Blood × 0.0002{µg}
gr for des trap fr = ([(0, 0) − (5, 0.6)], (0, 0.5), (0.1, 0.5), (0.386965, 0.491429), (0.661914,
0.47619), (0.824847, 0.460952), (1, 0.419131), (1.16208, 0.329825), (1.22324, 0.245614),
(1.2844, 0.154386), (1.43731, 0.0877193), (1.67006, 0.0333333), (1.96538, 0.0152381),
(2.27088, 0.0104762), (2.59674, 0.00761904), (2.99389, 0.0057143), (3.5336, 0.001),
(4.95927, 0.0005), (5, 0.0005)) {dimensionless}
gr for eff of I on thy cap = ([(0.9, 0) − (1.5, 1)], (0.9, 1), (0.91, 1), (0.920183, 0.964912),
(0.925662, 0.866667), (0.936697, 0.70614), (0.958656, 0.447619), (0.970876, 0.319048),
(0.977064, 0.263158), (0.98554, 0.195238), (0.997248, 0.140351), (1.01009, 0.098),
(1.02661, 0.0894737), (1.05596, 0.087), (1.09817, 0.086), (1.49, 0.085), (1.5, 0.085))
{dimensionless}
gr for eff of imp TRH sec on hypo wt = ([(0, 0) − (1, 4)], (0.02, 0.3), (0.021, 0.3),
(0.030581, 0.403509), (0.04058, 0.5316), (0.0814664, 0.723809), (0.224033, 0.8),
(0.366972, 0.9), (0.550459, 1), (0.733198, 1), (1, 1), (2, 1), (4.86762, 1.02857), (5.23014,
1.06667), (5.74338, 1.08571), (6.13442, 1.12381), (6.5499, 1.21905), (6.89206, 1.29524),
108
(7.18534, 1.37143), (7.55193, 1.48571), (7.96741, 1.58095), (8.28513, 1.69524), (8.77393,
1.90476), (9.28717, 2.15238), (9.75153, 2.4381), (10.1181, 2.7619), (10.3381, 3.00952),
(10.6558, 3.29524), (10.9491, 3.46667), (11.3157, 3.65714), (11.7067, 3.69524), (12, 3.7))
{dimensionless}
gr for eff of imp TSH sec on pit wt = ([(0, 0) − (12, 4)], (0.02, 0.3), (0.021, 0.3),
(0.030581, 0.403509), (0.04058, 0.5316), (0.0814664, 0.723809), (0.224033, 0.8),
(0.366972, 0.9), (0.550459, 1), (0.733198, 1), (1, 1), (2, 1), (4.86762, 1.02857), (5.23014,
1.06667), (5.74338, 1.08571), (6.13442, 1.12381), (6.5499, 1.21905), (6.89206, 1.29524),
(7.18534, 1.37143), (7.55193, 1.48571), (7.96741, 1.58095), (8.28513, 1.69524), (8.77393,
1.90476), (9.28717, 2.15238), (9.75153, 2.4381), (10.1181, 2.7619), (10.3381, 3.00952),
(10.6558, 3.29524), (10.9491, 3.46667), (11.3157, 3.65714), (11.7067, 3.69524), (12, 3.7))
{dimensionless}
gr for eff of pref T3 syn on red in T3 syn = ([(0, 0) − 1, 1)], (0, 1), (0.0001, 1), (0.0203666,
0.980952), (0.0305499, 0.966667), (0.0610998, 0.909524), (0.0916497, 0.838095),
(0.120163, 0.766667), (0.167006, 0.661905), (0.211813, 0.566667), (0.258656, 0.490476),
(0.297352, 0.438095), (0.329939, 0.4), (0.372709, 0.352381), (0.423625, 0.3), (0.484725,
0.252381), (0.560081, 0.195238), (0.623218, 0.147619), (0.672098, 0.114286), (0.729124,
0.0857143), (0.784114, 0.0619048), (0.828921, 0.047619), (0.881874, 0.0285714),
(0.936864, 0.0190476), (0.9999, 0), (1, 0)) {dimensionless}
gr for eff of T3 on peri conv = ([(0, 0.8) − (1, 1.7)], (0.0112016, 1.64762), (0.0492872,
1.648), (0.0940937, 1.64333), (0.147862, 1.62714), (0.199389, 1.58667), (0.264358, 1.53),
(0.329328, 1.47333), (0.387576, 1.41905), (0.445825, 1.36), (0.501833, 1.31143),
(0.55112, 1.26286), (0.613849, 1.20619), (0.676578, 1.14952), (0.737067, 1.10095),
(0.802037, 1.06333), (0.858045, 1.03619), (0.923014, 1.01333), (0.9999, 1), (1, 1))
{dimensionless}
gr for eff of TH on TRH sec = ([(−1.1, 0) − (1, 10)], (−1.09572, 10), (−1.04012, 9.90476),
(−0.997248, 9.7807), (−0.952294, 9.69298), (−0.900917, 9.38597), (− 0.860489, 9.14286),
( − 0.813442, 8.7619), (−0.759633,
8.42105),
7.04762), (−0.566972, 6.31579), (−0.451376,
(−0.693686,
5.13158),
7.71429),
(−0.393578,
(−0.629532,
4.51754),
(−0.284404, 3.50877), (−0.200917, 2.7193), (−0.143119, 2.2807), (−0.0660551, 1.53509),
109
(0, 1), (0.0174312, 0.868421), (0.0366972, 0.719298), (0.0489297, 0.574561), (0.0733945,
0.434211), (0.0948012, 0.315789), (0.134557, 0.22807), (0.180428, 0.153509), (0.248624,
0.118421), (0.33211, 0.100877), (0.440367, 0.0833333), (0.577982, 0.0701754),
(0.730887, 0.0657895), (0.852294, 0.0614035), (0.922936, 0.0570175), (0.999, 0.05), (1,
0.05)) {dimensionless}
gr for eff of TH on TSH sec = ([(0, 0) − (1, 1)], (0, 1), (0.0001, 1), (0.0366972, 0.982456),
(0.0519878, 0.969298), (0.0642202, 0.938596), (0.0764526, 0.903509), (0.088685,
0.850877), (0.0997963, 0.780952), (0.110092, 0.70614), (0.124236, 0.609524), (0.140673,
0.508772), (0.16208, 0.403509), (0.186544, 0.320175), (0.2263, 0.223684), (0.262997,
0.166667), (0.308868, 0.131579), (0.389002, 0.104762), (0.468432, 0.0857143),
(0.553517, 0.0745614), (0.629969, 0.0657895), (0.691131, 0.064), (0.776758, 0.063),
(0.83792, 0.0622), (0.902141, 0.0614035), (0.941896, 0.0570175), (0.99, 0.05), (1, 0.05))
{dimensionless}
gr for eff of TH store cap = ([(0, 0) − (1.5, 1)], (0, 0), (0.75, 0.75), (0.876147, 0.833333),
(0.947047, 0.87619), (1.00509, 0.919048), (1.05092, 0.942857), (1.09633, 0.960526),
(1.14679, 0.97807), (1.23, 1), (1.5, 1)) {dimensionless}
gr for eff of thy stim on TH fr([(1, 0) − (5, 2.5)], (1, 1), (1.001, 1), (1.1, 1.02), (1.39144,
1.0636), (1.67278, 1.12939), (1.96636, 1.18421), (2.3211, 1.27193), (2.54128, 1.34868),
(2.85933, 1.45833), (3.16514, 1.57895), (3.39755, 1.72149), (3.62997, 1.84211), (3.80122,
1.95175), (3.99694, 2.08333), (4.14373, 2.20395), (4.30275, 2.2807), (4.47401, 2.35746),
(4.64526, 2.42325), (4.823, 2.47368), (4.999, 2.5), (5, 2.5)) {dimensionless}
gr for eff of thy wt on I trap = ([(0, 0) − (3, 1.5)], (0, 0), (1e−005, 0), (0.0651731,
0.0285714), (0.126273, 0.0714285), (0.207739, 0.142857), (0.274949, 0.228571),
(0.360489, 0.333333), (0.427699, 0.428571), (0.519348, 0.580952), (0.629328, 0.71426),
(0.761711, 0.814286), (0.849287, 0.895238), (1, 1), (1.16701, 1.05714), (1.33198, 1.1),
(1.5096, 1.13571), (1.71079, 1.16429), (2.01629, 1.20714), (2.389, 1.25), (2.66395,
1.27143), (2.99, 1.3), (3, 1.3)) {dimensionless}
gr for eff of TRH on TSH sec = ([(−1, 0) − (1.1, 10.1)], (−1, 0.05), (−0.999, 0.05),
(−0.790428, 0.053), (−0.640733, 0.058), (−0.550917, 0.065), (− 0.478208, 0.0714286), (−
0.428135, 0.0833333), (−0.379205, 0.0921053), (−0.324159, 0.122807), (−0.272171,
110
0.153509), (−0.223242, 0.201754),
(−0.180428,
0.245614),
(−0.140673,
0.311404),
(−0.100917, 0.403509), (−0.0733945, 0.517544), (−0.0519878, 0.614035), (−0.0366972,
0.697368), (−0.0244648, 0.77193), (−0.0152905, 0.855263), (−0.00917431, 0.934211), (0,
1), (0.053211, 1.44737), (0.111009, 1.92982), (0.194495, 2.67544), (0.244603, 3.27048),
(0.308758, 3.94381), (0.355804, 4.56905), (0.406422, 5.30702), (0.449898, 6.1081),
(0.492668, 6.68524), (0.526884, 7.18857), (0.573931, 7.77143), (0.629532, 8.36857),
(0.680855, 8.84), (0.732179, 9.27714), (0.766395, 9.47476), (0.804888, 9.61905),
(0.864766, 9.81143), (0.924644,
9.90762),
(0.984521,
10.027),
(1.09572,
10.1))
{dimensionless}
gr for eff of TSH on I trap = ([( − 1, 0) − (1, 1.5)], ( − 1, 0.02), ( − 0.9999, 0.02), ( −
0.885947, 0.0357143), ( − 0.751527, 0.0785714), ( − 0.649695, 0.15), ( − 0.551935,
0.257143), ( − 0.412844, 0.440789), ( − 0.29052, 0.598684), ( − 0.155963, 0.776316), (0,
1), (0.120163, 1.1), (0.211009, 1.16429), (0.340122, 1.22143), (0.462322, 1.27143),
(0.565749, 1.308), (0.669725, 1.341), (0.828746, 1.38),
(0.9999,
1.4),
(1,
1.4))
{dimensionless}
gr for eff of TSH on TH sec = ([( − 1, 0) − (1.1, 10.1)], (−1, 0.05), (−0.999, 0.05),
(−0.790428, 0.053), (−0.640733, 0.058), (−0.550917, 0.065), (−0.478208, 0.0714286),
(−0.426884, 0.0904762), (−0.37556, 0.119048), (−0.327902, 0.144285), (−0.277189,
0.190476), (−0.23442, 0.228571), (−0.195927, 0.271429), (−0.161711, 0.338095),
(−0.131772, 0.419048), (−0.098778, 0.52381), (−0.0761711, 0.614286), (−0.0633401,
0.68), (−0.0498981, 0.761905), (−0.0291243, 0.847619), (−0.0162933, 0.92381), (0, 1),
(0.0606924, 1.34286), (0.129124, 1.77143),
(0.214664,
2.38095),
(0.278819,
3.06),
(0.334419, 3.64286), (0.381466, 4.46857), (0.419959, 5.24571), (0.462729, 6.02286),
(0.492668, 6.68524), (0.526884, 7.18857), (0.573931, 7.77143), (0.629532, 8.36857),
(0.680855, 8.84), (0.732179, 9.27714), (0.766395, 9.47476), (0.804888, 9.61905),
(0.864766, 9.81143), (0.924644, 9.90762),
(0.984521,
10.027),
(1.09572,
10.1))
{dimensionless}
gr for eff on HAT = ([(1, 30) − (5, 250)], (1, 30), (1.1, 30), (1.33028, 35.0877), (1.62385,
49.2982), (1.81957, 62.1053), (2.00306, 79.2105), (2.13761, 95.614), (2.27217, 113.684),
(2.3945, 137.632), (2.66361, 178.158), (2.84709, 200.263), (3.11621, 218.684), (3.45872,
111
228.816), (3.75229, 236.184), (4.10703, 242.632), (4.42508, 245.395), (5, 250))
{dimensionless}
gr for eff on PAT = ([(1, 30) − (5, 250)], (1, 30), (1.1, 30), (1.33028, 35.0877), (1.62385,
49.2982), (1.81957, 62.1053), (2.00306, 79.2105), (2.13761, 95.614), (2.27217, 113.684),
(2.3945, 137.632), (2.66361, 178.158), (2.84709, 200.263), (3.11621, 218.684), (3.45872,
228.816), (3.75229, 236.184), (4.10703, 242.632), (4.42508, 245.395), (5, 250))
{dimensionless}
gr for eff on TAT = ([(1, 30) − (5, 250)], (1, 30), (1.1, 30), (1.33028, 35.0877), (1.62385,
49.2982), (1.81957, 62.1053), (2.00306, 79.2105), (2.13761, 95.614), (2.27217, 113.684),
(2.3945, 137.632), (2.66361, 178.158), (2.84709, 200.263), (3.11621, 218.684), (3.45872,
228.816), (3.75229, 236.184), (4.10703, 242.632), (4.42508, 245.395), (5, 250))
{dimensionless}
gr for hypo cap = ([(0, 0) − (1.5, 1)], (0, 0), (0.75, 0.75), (0.855397, 0.838095), (0.934827,
0.9), (0.986762, 0.92381), (1.02953, 0.947619), (1.06925, 0.961905), (1.11813, 0.980952),
(1.23, 1), (1.5, 1)) {dimensionless}
gr for I store cap([(0, 0) − (1.1, 1)], (0, 0), (1e − 005, 0), (0.5, 0.5), (0.7, 0.7), (0.806517,
0.780952), (0.907332, 0.87619), (0.943177, 0.914286), (0.976782, 0.942857), (1.01039,
0.971429), (1.05, 1), (1.1, 1)) {dimensionless}
gr for imp TH sec on thy wt = ([(0, 0) − (12, 4)], (0.02, 0.3), (0.021, 0.3), (0.030581,
0.403509), (0.04058, 0.5316), (0.0814664, 0.723809), (0.224033, 0.8), (0.366972, 0.9),
(0.550459, 1), (0.733198, 1), (1, 1), (1.5, 1), (2.7156, 1.07), (3.52294, 1.19298), (4.55046,
1.36842), (5.50459, 1.54386), (6.45872, 1.73684), (7.52294, 2.03509), (8.51376, 2.40351),
(9.43119, 2.73684), (9.87156, 2.96491), (10.2018, 3.12281), (10.6055, 3.31579), (10.9725,
3.54386), (11.3157, 3.65714), (11.7067, 3.69524), (12, 3.7)) {dimensionless}
gr for pit cap = ([(0, 0) − (1.5, 1)], (0, 0), (0.75, 0.75), (0.855397, 0.838095), (0.934827,
0.9), (0.986762, 0.92381), (1.02953, 0.947619), (1.06925, 0.961905), (1.11813, 0.980952),
(1.23, 1), (1.5, 1)) {dimensionless}
gr for T3 sec fr = ([(0.9, 0.9) − (1.1, 1)], (0.9, 0.9), (0.97, 0.97), (0.97844, 0.976754),
(0.988685, 0.982456), (1.00153, 0.988596), (1.01437, 0.991667), (1.02477, 0.99386),
(1.04434, 0.99693), (1.07, 1), (1.1, 1)) {dimensionless}
112
gr for thy cap = ([(0, 0) − (1.5, 1)], (0, 0), (0.75, 0.75), (0.855397, 0.838095), (0.934827,
0.9), (0.986762, 0.92381), (1.02953, 0.947619), (1.06925, 0.961905), (1.11813, 0.980952),
(1.23, 1), (1.5, 1)) {dimensionless}
HAT = LOOKUP EXTRAPOLATE(gr for eff on HAT, ratio of des hypo wt to hypo wt)
{days}
hypo cap = Hypo Wt × normal hypo prod × 10 {ng / day}
Hypo Wt = INTEG (Hypo wt chg, 40) {mg}
Hypo wt chg = (des hypo wt − Hypo Wt) / HAT {mg / day}
I abs rate = I intake × abs fr of I {µg / day}
I cons = I cons for T3+I cons for T4 {µg / day}
I cons for T3 = T3 syn rate × 3 × 126.904 / 651 {µg / day}
I cons for T4 = T4 syn rate × 4 × 126.904 / 777 {µg / day}
I excr = I in Blood × excr fr {µg / day}
I from deiod = 0.8 × retained I {µg / day}
I from rT3 = (126.904 / 777) × Conv rate to rT3 {µg / day}
I from T3 conv = (126.904 / 777) × T4 to T3 conv rate {µg / day}
I from T3 in tissues = 3 × (126.904 / 651) × Abs rate of T3 by tissues {µg / day}
I from T4 in tissues = 4 × (126.904 / 777) × Abs rate of T4 by tissues {µg / day}
I in Blood = INTEG (I abs rate+I from deiod − I excr − Trap rate, 150) {µg}
I in Thy = INTEG (Trap rate − I cons, 15000) {µg}
I inhib thres = MAX(SMOOTH3I( I in Thy, 30, 15000 ) × 1.1, 400) {µg}
I intake = 150 {µg / day}
imp TH sec = normal TH sec × eff of TSH on TH sec {µg / day}
imp TRH sec = normal TRH sec × eff of TH on TRH sec {ng / day}
imp TSH sec = eff of TRH on TSH sec × eff of TH on TSH sec × normal TSH sec {mU /
day}
log ratio of TH to normal = LOG(ratio of TH to normal TH, 10) {dimensionless}
log ratio of TRH to normal = LOG( ratio of TRH to normal, 10 ) {dimensionless}
log ratio of TSH to normal = LOG(ratio of TSH to normal, 10) {dimensionless}
MW of T3 = 651 × 1.66054 × 10^( − 18) {µg}
113
MW of T4 = 777 × 1.66054 × 10^( − 18) {µg}
normal amount of T3 mol = 1.38759e+013 {dimensionless}
normal amount of T4 mol = 3.72024e+013 {dimensionless}
normal hypo prod = 24 × (LN(2) / (6.2 / 60)) × 2 / 40 {ng / day / mg}
normal hypo wt = 40 {mg}
normal I in thy = 15000 {µg}
normal pit prod = 24 × 6.6 × LN(2) / 22.5 {mU / day / mg}
normal pit wt = 22.5 {mg}
normal ratio of T3 to T4 = normal amount of T3 mol / normal amount of T4 mol
{dimensionless}
normal T3 in blood = 5 {µg}
normal T4 to T3 conv fr = (28 / 240) × 777 / 651 {dimensionless}
normal TH = 5.10783e+013 {dimensionless}
normal TH sec = 97 {µg / day}
normal thy prod = 97 / 20 {µg / day / g}
normal thy wt = 20 {mg}
normal TRH = 2 {ng}
normal TRH sec = 24 × (LN(2) / (6.2 / 60)) × 2 {ng / day}
normal TSH = 6.6 {mU}
normal TSH sec = 24 × 6.6 × LN(2) {mU / day}
PAT = LOOKUP EXTRAPOLATE(gr for eff on PAT, ratio of des pit wt to pit wt) {day}
pit cap = normal pit prod × Pit Wt × 10 {mU / day}
Pit Wt = INTEG (Pit wt chg, 22.5) {mg }
Pit wt chg = (des pit wt − Pit Wt) / PAT {mg / day}
pos I cons = I in Thy × 0.15 {µg / day}
pos T3 sec = T3 Store × 0.15 {µg / day}
pos T4 sec = T4 Store × 0.15 {µg / day}
pot fr of T3 sec = (normal ratio of T3 to T4 × 7 / 90) / (ratio of T3 to T4 + normal ratio of
T3 to T4 × 7 / 90) × eff of thy stim on T3 fr {dimensionless}
pot I cons for T3 = pot T3 syn × 3 × 126.904 / 651 {µg / day}
114
pot I cons for T4 = pot T4 syn × 4 × 126.904 / 777 {µg / day}
pot T3 sec = pot TH sec × fr of T3 sec {µg / day}
pot T3 syn = eff of thy cap on T3 syn × thy syn cap for T3 {µg / day}
pot T4 sec = pot TH sec × fr of T4 sec {µg / day}
pot T4 syn = eff of thy cap on T4 syn × thy syn cap for T4 {µg / day}
pot TH sec = eff of cap on TH sec × thy cap {µg / day}
pot TH syn = pot T3 syn+pot T4 syn {µg / day}
pot total I cons = pot I cons for T3 + pot I cons for T4 {µg / day}
pot total I cons under I cap rest = pos I cons × eff of thy I cap {µg / day}
Pot Trap Fr = INTEG (chg in trap fr, (62.8697 / 150)) {1 / day}
ratio of cap rest I cons to pot = pot total I cons under I cap rest / pot total I cons
{dimensionless}
ratio of des hypo wt to hypo wt = des hypo wt / Hypo Wt {dimensionless}
ratio of des pit wt to pit wt = des pit wt / Pit Wt {dimensionless}
ratio of des T3 syn to cap = MAX( des T3 syn , 0) / thy syn cap for T3 {dimensionless}
ratio of des T4 syn to cap = MAX( des T4 syn , 0) / thy syn cap for T4 {dimensionless}
ratio of des thy wt to thy wt = des thy wt / Thy Wt {dimensionless}
ratio of disc btw I rest TH syn and pot TH syn to pot TH syn = 1 − ratio of cap rest I cons
to pot {dimensionless}
ratio of I in thy to thres = I in Thy / I inhib thres {dimensionless}
ratio of imp TH sec to thy cap = imp TH sec / thy cap {dimensionless}
ratio of imp TRH sec to hypo cap = imp TRH sec / hypo cap {dimensionless}
ratio of imp TSH sec to pit cap = imp TSH sec / pit cap {dimensionless}
ratio of pos to pot T3 sec = pos T3 sec / pot T3 sec {dimensionless}
ratio of pos to pot T4 sec = pos T4 sec / pot T4 sec {dimensionless}
ratio of pot to pos I cons = pot total I cons / pos I cons {dimensionless}
ratio of short smth imp TH sec to normal = short smth imp TH sec / normal TH sec
{dimensionless}
ratio of smth imp TH sec to normal = smth imp TH sec / normal TH sec {dimensionless}
115
ratio of smth imp TRH sec to normal = smth
imp
TRH
sec
/
normal
TRH
sec
imp
TSH
sec
/
normal
TSH
sec
{dimensionless}
ratio of smth imp TSH sec to normal = smth
{dimensionless}
ratio of T3 to normal = T3 in Blood / normal T3 in blood {dimensionless}
ratio of T3 to T4 = total free T3 molecules / total free T4 molecules {dimensionless}
ratio of TH to normal TH = "total free T3&T4 molecules" / normal TH {dimensionless}
ratio of thy I conc to normal = I in Thy / normal I in thy {dimensionless}
ratio of TRH to normal = TRH / normal TRH {dimensionless}
ratio of TSH to normal = TSH / normal TSH {dimensionless}
retained I = I from rT3+I from T3 in tissues+I from T4 in tissues+I from T3 conv {µg /
day}
short smth imp TH sec = SMOOTH3I( imp TH sec, 10, 97 ) {µg / day}
smth imp TH sec = SMOOTH3I( imp TH sec, 20, 97 ) {µg / day}
smth imp TRH sec = SMOOTH3I(imp TRH sec, 20, 24 × (LN(2) / (6.2 / 60)) × 2) {ng /
day}
smth imp TSH sec = SMOOTH3I( imp TSH sec, 20, 24 × 6.6 × LN(2) ) {mU / day}
T3 clear fr = LN(2) / 1 {1day}
T3 clear rate = T3 in Blood × T3 clear fr {µg / day}
T3 conc = T3 in Blood / 30 {µg / dL}
T3 from deiod of T4 = T4 to T3 conv rate × 651 / 777 {µg / day}
T3 in Blood = INTEG (T3 from deiod of T4+T3 sec rate − Abs rate of T3 by tissues − T3
clear rate, 5) {µg}
T3 sec rate = pot T3 sec × eff of T3 store cap {µg / day}
T3 Store = INTEG (T3 syn rate − T3 sec rate,420) {µg}
T3 store adj = disc from des T3 store / AT for store restor {µg / day}
T3 syn rate = (pot T3 syn − disc btw pot T3 syn and I rest T3 syn × eff of pref T3 syn on
red in T3 syn) / MAX(1, (pot T3 syn / MAX(1e − 005,(pot TH syn − disc btw pot TH syn
and I rest TH syn)))) {µg / day}
T4 clear fr = LN( 2 ) / (7) {1 / day}
116
T4 clear rate = T4 in Blood × T4 clear fr {µg / day}
T4 conc = T4 in Blood / 30 {µg / dL}
T4 in Blood = INTEG (T4 sec rate − Abs rate of T4 by tissues − Conv rate to rT3 − T4
clear rate − T4 to T3 conv rate, 240) {µg}
T4 sec rate = pot T4 sec × eff of T4 store cap {µg / day}
T4 Store = INTEG (T4 syn rate − T4 sec rate, 5400) {µg}
T4 store adj = disc from des T4 store / AT for store restor {µg / day}
T4 syn rate = pot TH syn − disc btw pot TH syn and I rest TH syn − T3 syn rate {µg /
day}
T4 to T3 conv fr = eff of T3 conc on peri conv × normal T4 to T3 conv fr {1 / day}
T4 to T3 conv rate = T4 in Blood × T4 to T3 conv fr {µg / day}
TAT = LOOKUP EXTRAPOLATE(gr for eff on TAT, ratio of des thy wt to thy wt) {day}
thy cap = normal thy prod × Thy Wt × 10 × eff of I on thy cap {µg / day}
thy syn cap for T3 = thy cap × fr of T3 sec {µg / day}
thy syn cap for T4 = thy cap × fr of T4 sec {µg / day}
Thy Wt = INTEG (Thy wt chg, 20) {g}
total free T3 molecules = free T3 in blood / MW of T3 {dimensionless}
"total free T3&T4 molecules" = total
free
T3
molecules+total
free
T4
molecules{dimensionless}
total free T4 molecules = free T4 in blood / MW of T4{dimensionless}
total normal TH store = 5400 + 420 {µg}
Trap rate = Pot Trap Fr × I in Blood × eff of TSH on I trapping × eff of thy wt on I trap
{µg / day}
TRH = INTEG (TRH sec rate − TRH clear rate, 2) {ng}
TRH clear fr = LN(2) / (6.2 / (60 × 24)) {1 / day}
TRH clear rate = TRH × TRH clear fr {ng / day}
TRH conc = TRH / 10 {ng / ml}
TRH sec rate = eff of cap on TRH sec × hypo cap {ng / day}
TSH = INTEG (TSH sec rate − TSH clear rate, 6.6) {mU}
TSH clear fr = 24 × LN(2) {1 / day}
117
TSH clear rate = TSH × TSH clear fr {mU / day}
TSH conc = TSH / 3 {µU / ml}
TSH sec rate = eff of cap on TSH sec × pit cap {mU / day}
118
REFERENCES
Barlas, Y., 2002, “System Dynamics: Systemic Feedback Modeling for Policy Analysis”,
In Knowledge for Sustainable Development - An Insight into the Encyclopedia of Life
Support Systems, UNESCO-EOLSS Publishers, Paris, France; Oxford, UK, pp. 11311175.
Barlas, Y., 1996, “Formal Aspects of Model Validity and Validation in System
Dynamics”, System Dynamics Review, Vol. 12, No. 3, pp. 183-210.
Ben-Shachar, R., M. Eisenberg, S. A. Huang, and J. J. DiStefano III, 2012, “Simulation of
Post-Thyroidectomy Treatment Alternatives for Triiodothyronine or Thyroxine
Replacement in Pediatric Thyroid Cancer Patients”, Thyroid, Vol. 22, No. 6, pp. 595603.
Bhagavan, N. V., 2002, Medical Biochemistry (4th edn), Harcourt/Academic Press, San
Diego.
Braunwald, E., A. S. Fauci, D. L. Kasper, S. L. Hauser, D. L. Longo, and J. L. Jameson
(eds), 2001, Harrison’s Principles of Internal Medicine (15th edn), McGraw-Hill, New
York.
Braverman, L. E., 2003, Diseases of the Thyroid (2nd edn), Humana Press, New Jersey.
Brent, G. A., 2008, “Graves’ Disease”, The New England Journal of Medicine, Vol. 358,
pp. 2594-2605.
Brent, G. A., 2010, Thyroid Function Testing, Springer, New York.
119
Bürgi, H., 2010, “Iodine Excess”, Best Practice & Research Clinical Endocrinology &
Metabolism, Vol. 24, pp. 107-115.
Brown, J. H. U., and D. S. Gann (eds), 1973, Engineering Principles in Physiology,
Academic Press, New York.
Carruthers, S. G., B. B. Hoffman, K. L. Melmon, and D. W. Nierenberg (eds), 2000,
Melmon and Morrelli’s Clinical Pharmacology: Basic Principles in Therapeutics,
McGraw Hill, USA.
Conn P. M. (ed), 2008, Neuroscience in medicine. Humana Press, USA.
Dayan, C. M., and G. H. Daniels, 1996, “Chronic Autoimmune Thyroiditis”, The New
England Journal of Medicine, Vol. 335, No. 2, pp. 99-108.
Degon, M., S. R. Chipkin, C. V. Hollot, R. T. Zoeller, and Y. Chait, 2008, “A
Computational Model of the Human Thyroid”, Mathematical Biosciences, Vol. 212,
No. 1, pp. 22-53.
DiStefano III, J. J., and E. B. Stear, 1968, “Neuroendocrine Control of Thyroid Secretion
in Living Systems: A Feedback Control System Model”, Bulletin of Mathematical
Biology, Vol. 30, No. 1, pp. 3-26.
DiStefano III, J. J., 1969, “A Model of the Normal Thyroid Hormone Glandular Secretion
Mechanism”, Journal of Theoretical Biology, Vol. 22, No. 3, pp. 412-417.
DiStefano III, J. J., 1969, “Hypothalamic and Rate Feedback in the Thyroid Hormone
Regulation System: An Hypothesis”, Bulletin of Mathematical Biology, Vol. 31, No. 2,
pp. 233-246.
120
DiStefano III, J. J., and R. F. Chang, 1971, “Computer Simulation of Thyroid Hormone
Binding, Distribution, and Disposal Dynamics in Man”, American Journal Physiology,
Vol. 221, No. 5, pp. 1529-1544.
DiStefano III, J. J., and F. Mori, 1977, “Parameter Identifiability and Experiment Design:
Thyroid Hormone Metabolism Parameters”, AJP - Regulatory, Integrative and
Comparative Physiology, Vol. 233, No. 3, pp. 134-144.
Donovan, B. T., 1966, The Pituitary Gland, Volume 2. University of California Press,
California.
Eisenberg, M., M. Samuels, and J. J. DiStefano III, 2006, “L-T4 Bioequivalence and
Hormone Replacement Studies via Feedback Control Simulations”, Thyroid, Vol. 16,
No. 12, pp. 1279-1292.
Erkut, Z. A., C. Pool, and D. F. Swaab, 1998, “Glucocorticoids Suppress CorticotropinReleasing Hormone and Vasopressin Expression in Human Hypothalamic Neurons”,
The Journal of Clinical Endocrinology & Metabolism, Vol. 83, No. 6, pp. 2066-2073.
Gardner D. F., R. M. Centor, and R. D. Utiger, 1988, “Effect of Low Dose Oral Iodide
Supplementation on Thyroid Function in Normal Men”, Clinical Endocrinology
(Oxford), Vol. 28, pp. 283–288.
Garrison, R., and E. Somer, 1995, The Nutrition Desk Reference, Keats Publishing, USA.
Georgitis W. J., M. T. McDermott, and G. S. Kidd, 1993, “An Iodine Load from WaterPurification Tablets Alters Thyroid Function in Humans”, Military Medicine, Vol. 158,
No. 12, pp. 794-7.
Goldman, M. B., and M. C. Hatch, 2000, Women and Health, Academic Press, USA.
121
Goodman, H. M., 2009, Basic Medical Endocrinology (4th edn), Academic Press, China.
Greenstein, B., and D. Wood, 2011, The Endocrine System at a Glance (3rd edn), WileyBlackwell.
Grossman, A. (ed), 1998, Clinical Endocrinology (2nd edn), Blackwell Science, United
Kingdom.
Guyton, A. C., and J. E. Hall., 2006, Textbook of Medical Physiology, W.B. Saunders
Company, Philadelphia.
Hays, M., 2009, “Mathematical Models of Human Iodine Metabolism, Including
Assessment of Human Total Body Iodine Content”, In: Comprehensive Handbook of
Iodine, edited by V. R. Preedy, G. N. Burrow and R. R. Watson, Academic Press,
USA.
Izumi, M., and P. R. Larsen, 1977, “Triiodothyronine, Thyroxine, and Iodine in Purified
Thyroglobulin from Patients with Graves' Disease”, The Journal of Clinical
Investigation, Vol. 59, No. 6, pp. 1105-1112.
Khee, M., and S. Leow, 2007, “A Mathematical Model of Pituitary–Thyroid Interaction to
Provide an Insight into the Nature of the Thyrotropin–Thyroid Hormone Relationship”,
Journal of Theoretical Biology, Vol. 248, No. 2, pp. 275-287.
Kronenberg H. M., S. Melmed, K.S. Polonsky, and P. R. Larsen, 2008, Williams Textbook
of Endocrinology, Saunders, Philadelphia.
Laurberg, P., 1984, “Mechanisms Governing the Relative Proportions of Thyroxine and
3,5,3’-Triiodothyronine in Thyroid Secretion”, Metabolism, Vol. 33, No. 4, pp. 379392.
122
Lazarus, J. H., 2009. “Acute and Subacute Thyroiditis”. In The Thyroid and Its Diseases.
Available: http://www.thyroidmanager.org/Chapter19/19-frame.htm.
LeMar H. J., Georgitis W. J., and McDermott M. T., 1995, “Thyroid Adaptation to
Chronic Tetraglycine Hydroperiodide water purification tablet use”, The Journal of
Clinical Endocrinology and Metabolism, Vol. 80, pp. 220–223.
Liu, B. Z., and J. H. Peng, 1990, “A Mathematical Model of Hypothalamo-PituitaryThyroid Axis”, Acta Biophysica Sinica, Vol. 6, pp. 431-437.
Liu, Y. W., and B. Z. Liu, 1992, “An Improved Mathematical Model of HypothalamoPituitary-Thyroid Axis”, Progress in Biochemistry and Biophysics, Vol. 6 pp. 439-443.
Liu, Y. W., B. Z. Liu, J. Xie, and Y. X. Liu, 1994, “An Improved Mathematical Model of
Hypothalamo-Pituitary-Thyroid Axis”, Mathematical and Computer Modelling, Vol.
19, No. 9, pp. 81-90.
Mak, P. H., and J. J. DiStefano III, 1977, “Optimal Control Policies for
the Prescription of Thyroid Hormones”, Mathematical Biosciences, Vol. 42, No. 3-4,
pp. 159-186.
Martini, F. H., 2007, Fundamentals of Anatomy and Physiology, Pearson, Philippines.
McMonigal K. A., L. E. Braverman, J. T. Dunn, J. B. Stanbury, M. L. Wear, P. B. Hamm,
R. L. Sauer, R. D. Billica, and S. L. Pool, 2000, “Thyroid Function Changes Related to
Use of Iodinated Water in The U.S. Space Program”, Aviation Space and
Environmental Medicine, Vol. 71, No. 11, pp. 1120-5.
Melmed, S., 2002, The Pituitary, Blackwell Science, Cambridge.
123
Melmed, S., and P. M. Conn, 2005, Endocrinology: Basic and Clinical Principles,
Humana Press, New Jersey.
Molina, P. E., 2004, Endocrine Physiology, McGraw-Hill Professional, USA.
Motta, M., 1991, Brain Endocrinology, Raven Press, New York.
Namba H., S. Yamashita, H. Kimura, N. Yokoyama, T. Usa, A. Otsuru, M. Izumi, and S.
Nagataki, 1993, “Evidence of Thyroid Volume Increase in Normal Subjects Receiving
Excess Iodide”, The Journal of Clinical Endocrinology & Metabolism, Vol. 76, pp.
605–608.
Negi, C. S., 2009, Introduction to Endocrinology, PHI Learning, New Delhi.
Nussey, S., and S. Whitehead, 2001. Endocrinology: An Integrated Approach, Oxford,
London.
Nyström, E., G. E. B. Berg, S. K. G. Jansson, O. Torring, and S. V. Valdemarsson, 2011,
Thyroid Disease in Adults, Springer, Berlin.
Oertli, D., and R. Udelsman (eds), 2007, Surgery of the Thyroid and Parathyroid Glands,
Springer, Berlin.
Paul, T., B. Meyers, R. J. Witorsch, S. Pino, S. Chipkin, S. H. Ingbar, and L. E.
Braverman, 1988, “The Effect of Small Increases in Dietary Iodine on Thyroid Function
in Euthyroid Subjects”, Metabolism, Vol. 37, pp. 121–124.
Philippou G., D. A. Koutras, G. Piperingos, A. Souvatzoglou, and S. D. Moulopoulos,
1992, “The Effect of Iodide on Serum Thyroid Hormone Levels in Normal Persons, in
Hyperthyroid Patients, and in Hypothyroid Patients on Thyroxine Replacement”,
Clinical Endocrinology (Oxford), Vol.36, pp. 573–578.
124
Raymond, K. W., 2009, General Organic and Biological Chemistry, Wiley, USA.
Rhoades, R. A., and D. R., Bell, 2009, Medical Physiology: Principles for Clinical
Medicine (3rd edn), Lippincott Williams & Wilkins, Philadelphia.
Rubin, A. L., 2006, Thyroid for Dummies (2nd edn), Wiley, New Jersey.
Smith, P. E., 1930, “Hypophysectomy and a Replacement Therapy in the Rat”, American
Journal of Anatomy, Vol. 45, No. 2, pp. 205-273.
Sodeman, W. A., and T. M. Sodeman, 1985, Pathologic Physiology: Mechanisms of
Disease, Saunders, Philadelphia.
Stanbury, J. B., A. E. Ermans, P. Bourdoux, C. Todd, E. Oken, R. Tonglet, G. Vidor, L. E.
Braverman, and
G.
Medeiros-Neto,
1998,
“Iodine-Induced
Hyperthyroidism:
Occurrence and Epidemiology”, Thyroid, Vol. 8, No. 1, pp. 83-100.
Synder, P. J., and R. D. Utiger, 1972. “Inhibition of Thyrotropin Response to ThyrotropinReleasing Hormone by Small Quantities of Thyroid Hormones”, The Journal of
Clinical Investigation, Vol. 51, pp. 2077-2084.
Thapar, K., K. Kovacs, B. W. Scheithauer, and R. V. Lloyd, 2001. Diagnosis and
Management of Pituitary Tumors, Humana Press, New Jersey.
Tucker, M. J., 1999, “Pituitary Toxicology: Direct Toxicity, Secondary Changes and Effects
on Distal Target Tissues”, In: Endocrine and Hormonal Toxicology, edited by P. W.
Harvey, K. C. Rush and A. Cockburn, Wiley, England.
Van den Berghe, G., 2008, Acute Endocrinology: From Cause to Consequence, Humana
Press, New York.
125
Vagenakis A. G., P. Downs, L. E. Braverman, A. Burger, and S. H. Ingbar, 1973, “Control
of Thyroid Hormone Secretion in Normal Subjects Receiving Excess Iodides”, The
Journal of Clinical Investigation, Vol. 52, pp. 528–532.
Vassart, G., and J. E. Dumont, 1992, “The Thyrotropin Receptor and the Regulation of
Thyrocyte Function and Growth”, Endocrine Reviews, Vol. 13, No. 3, pp. 596-611.
Van Vliet, G., and M. Polak, 2007, Thyroid Gland Development and Function, Karger,
Switzerland.
Werner, S. C., S. H. Ingbar, L. E. Braverman, and R. D. Utiger, 2005, Werner & Ingbar’s
The Thyroid: A Fundamental and Clinical Text, Lippincott Williams & Wilkins,
Philadelphia.
White, W. E., 1933, “The Effect of Hypophysectomy on the Rabbit”, In: Proceedings of
the Royal Society of London, Vol. 114, No. 786, pp. 64-79.
Wilson, K. C., J. J. DiStefano III, D. A. Fisher, and J. Sack, 1977, “System Analysis and
Estimation of Key Parameters of Thyroid Hormone Metabolism in Sheep”, Annals of
Biomedical Engineering, Vol. 5, No. 1, pp. 70-84.
Yadav, M., 2008, Mammalian Endocrinology, Discovery Publishing House, New Delhi.
Zimmermann, M. B., 2009, “Iodine Deficiency”, Endocrine Reviews, Vol. 30, No. 4, pp.
376-408.