* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hib vaccine
Poliomyelitis eradication wikipedia , lookup
Brucellosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Tuberculosis wikipedia , lookup
Cysticercosis wikipedia , lookup
Trichinosis wikipedia , lookup
Anthrax vaccine adsorbed wikipedia , lookup
West Nile fever wikipedia , lookup
Rotaviral gastroenteritis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Typhoid fever wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Onchocerciasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Poliomyelitis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Neonatal infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hepatitis C wikipedia , lookup
Gastroenteritis wikipedia , lookup
Leptospirosis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Hepatitis B wikipedia , lookup
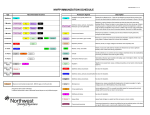
Review of childhood and Adolescent Vaccination 2010 Marie-Denise Gervais, M.D. Department of Family Medicine and Community Health University of Miami, Miller School of Medicine Childhood Vaccination The impact of routine vaccination on childhood diseases in U.S. is considered one of the major medical achievements of the 20th century… Trends in Deaths Caused by Infectious Disease (US) Mortality Rates per 100,000 US Population 900 800 700 600 500 400 300 65 60 55 50 45 40 35 30 25 1980 1984 1988 1992 1982 1986 1990 1994 200 100 0 1900 1910 1920 1930 1940 1950 1960 1970 1980 1990 Year Centers for Disease Control and Prevention. US Dept of Health and Human Services, 1998. Vaccine Development Disease Year Disease Year Smallpox Rabies Typhoid Cholera Plague Diphtheria Pertussis Tetanus Tuberculosis Influenza Yellow fever Poliomyelitis Measles 1798 1885 1896 1896 1897 1923 1926 1927 1927 1945 1953 1955 1963 Mumps Rubella Anthrax Meningitis Pneumonia Adenovirus Hepatitis B Haemophilus Influenzae type b Hepatitis A Varicella Lyme disease Rotavirus 1967 1969 1970 1975 1977 1980 1981 1985 MMWR Morb Mortal Wkly Rep. 1999;48(12):243-248. 1995 1995 1998 1998 Morbidity Pre- and PostVaccinations (US) Disease Smallpox Diphtheria Pertussis (paralytic) Tetanus Poliomyelitis Measles Mumps Rubella Haemophilus Influenzae type b Annual Morbidity Prior to Vaccine* Morbidity 1998 % Decrease 48,164 175,885 0 1 100% >99.9% 147,271 1,314 16,316 503,282 152,209 47,745 6,279 34 0 89 606 345 95.7% 97.4% 100% >99.9% 99.6% 99.3% 20,000 54 99.7% MMWR Morb Mortal Wkly Rep. 1999;48(12):243-248. Principles of Vaccination Immunity Self vs non- self Protection from infectious diseases Active Immunity Protection produced by a person’s own immune system Usually permanent Trigerred by Antigens Passive Immunity Protection transferred from another person or animal as antibody Wanes over time (weeks,months) Active immunity Stimulation of immune system to produce Ag- specific humoral(Ab) and cellular immunity through : Natural disease : immunity is long through immunologic memory Vaccination : similar memory without the risk of disease Classification of vaccines Live attenuated – Must replicate to be effective – Usually effective with 1 dose – Severe reactions possible – Interference with circular Ab – MMR, Varicella,nasal Flu, OPV Inactivated – – – – Heat / Formalin Cannot replicate Requires 3-5 doses Immune response mostly humoral – Ab titer falls overtime – Principal Ag may not be defined (hib) – IPV,DTaP, Hep B,A Pertussis Most hospitalizations and complications occur in infants 1/2 cases occur in infants, 3/4 in children ≤ 5y/o Complication: pneumonia*(15%), seizures(2.2%) , encephalopathy (0.7%) and permanent brain damage Source: respiratory droplets from adults and adolescents Highly contagious Pertussis cont’d Contagiosity is long (7days post exposure to 3 weeks after symptoms onset) Incubation: 5 to 21 days (7-10) Immunity is lifelong Transplacental immunity wanes rapidly after birth Recent outbreaks in US since 1990’s Pertussis vaccine DTP 70% to 90% effective. DTP adverse reactions: persistent crying, unusual high-pitched cry, seizures, hypotonichyporesponsive episodes. Protection wanes with time ≤ 12 years. DTaP has1/4 to 1/2 the adverse reactions. DTaP not recommended after age 7. 2006: Tdap adolescent prep 11-12 y/o. Tetanus and Diphteria Hundreds of thousands of tetanus deaths worldwide – Only 26 cases of Tetanus in 2000 in US – Spasms of jaw muscles( trismus) and back muscles(opisthotonos). In the 1920’s, 14,000 deaths/year to diphteria – Only 2 cases of diphteria in 2000 in US – Tonsillitis, myocarditis, heart failure and neuritis Td / Tdap Tdap recommended for 1st booster dose then Td every 10 years for persons ≥ 12 y/o. Contains same quantity of tetanus toxoid as DTP , DTap and DT. Contains only 1/11 as much diphteria toxoid. Arthrus-type hypersensitivity reaction or fever ≥ 103ºF should not receive Td more often than every 10 years. Haemophilus Influenzae type B Most common cause of bacterial meningitis in children≤5 y/o. Peak incidence 6- 12 months of age. Meningitis has 2%-5% mortality rate even with appropriate treatment Neurologic sequelae in 30% of survivors Epiglottitis, facial, orbital and periorbital cellulitis, pneumonia, osteomyelitis,septic arthritis and pericarditis. Hib vaccine Hib organism is encapsulated in polysaccharide capsule. Unencapsulated H-flu colonize the respiratory tract (sinusitis, otitis media, bronchitis). Vaccines against Hib do not protect against other strains of Hflu. Immature immune systems of infants do not respond to polysaccharide Ag Ag of Hib capsule is linked to other proteins (diphteria, tetanus, meningococcal) to improve recognition. Hib vaccine (cont’d) Hib not given before 6 weeks of age (may induce tolerance to Ag) Efficacy 95% to 100 % Also decreases nasopharyngial carriage Unimmunized children acquire natural immunity by age 5. No serious adverse reactions. Poliomyelitis 18,000 paralytic cases in 1954 in US. Last case of indigenous polio : 1979 US, 1994 Peru. Recent outbreak in D.R and Haiti due to a revertant virus. Enterovirus, 3 serotypes, feco-oral route,75% to 95% transmission in household contacts. Subclinical infection(95%), non specific viral illness(5%), nonparalytic meningitis, paralysis. Polio Vaccines IPV-Salk (inactivated) – Cannot cause VAPP – Safe for immunocompromized – IM injection – Less GI immunity OPV (attenuated) – Easier administration – Cohort effect – Can revert and cause VAPP ( 1 case per 2.4 million doses of OPV.) – No longer recommended in US MMR Combination of 3 live attenuated vaccines – Contains neomycin, gelatin, sorbitol, human albumin, and is produced in chick cells. Maternal Ig persist until 9-11 months. – 1st dose is recommended at 12-15 months. – Ab persist ≥ 17 years (life!) Adverse reactions: pain ,irritation, redness. Specific delayed reactions: – Measles..fever and rash. – Mumps…transient orchitis – Rubella…lymphadenopathy and arthralgia. Ongoing Mumps outbreaks in Iowa Hepatitis B 128,000 to 320,000 infected annually in U.S. HBV infection more likely to become chronic when acquired early in life: • 90% as infants • 30% to 60% if less than 4 y/o • 5% to 10% as adults 36% of all HBV infection contracted the infection in childhood HBV is the 2nd cause of cancer worldwide Rationale for HepB vaccination HBV infection high morbidity and mortality. HBV infection from child to child reported in schools, daycare centers, families. No risk factor was identified in 30% of infected persons. Cost effectiveness of vaccine. Protective Ab levels ( ≥ 10mIU) in 95% of children. Standing orders for Hep B vaccines at birth. Streptococcus Pneumoniae Encapsulated organism, 90 serotypes Most common bacterial cause of meningitis*, bacteremia, pneumonia, otitis media in US Incidence highest in infants then declines with age and increases in the elderly Risk factors; age, race, recent use of Abx, daycare, exposure to tobacco smoke, chronic medical conditions; sickle-cell and HIV Pneumococcal conjugate vaccines 3 vaccines are available : – Pneumovax, 23-valent, polyssacharide . – Prevnar, 7-valent,conjucated. - (new) Prevnar,13-valent, conjugated. Pneumovax ( only stimulates B lymphocytes) not effective in children ≤ 2y/o. Prevnar elicits T-dependant immune response. – $108 per dose… most expensive routine infant immunization series to date. – No serious adverse reaction with Prevnar. Varicella 4 millions cases of VZV infection per year in US. Hospitalization rate: 5/1000 cases. Death rate: 0.7/100,000 cases. Secondary attack rates: 90%. Complications: Impetigo , pneumonia , ataxia , encephalomeningitis, glomerulonephritis … Most severe in neonates and adults. Varicella vaccine Live attenuated virus 97% effective against severe disease 85% protective for any infection; for ≥ 7years Less immunogenic in older children Ab levels have persisted 20 y in Japan Adverse reaction 25% after 1st dose, 47% after 2nd dose Possible postexposure prophylaxis 2005-10 New Vaccines Rota Teq: live oral rotavirus; 2- 4- 6m. ProQuad: MMRV Hepatitis A: Havrix; 2 doses 6 months apart after 1 year. Influenza: expanded indication 6- 59 m (23) Meningococcal MCV4 age 11-12y/o Pediarix: (DTaP+ IPV+ HepB) HPV *:3 doses after age 9 (0,2,6m) cdc.gov cdc.gov cdc.gov cdc.gov Recommended Childhood Immunization Recommended Childhood Immunization Catch-up Schedule Catch-up Schedule Thank You!