* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chronic Liver Diseases
Survey
Document related concepts
Transcript
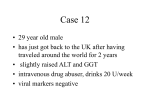
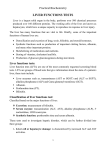
Chapter 8 Diagnostic Enzymology And Other Biochemical Markers Of Organ Damage Lixia Zhang Contents • • • Basic Concepts For Diagonostic Enzymology Enzyme Assay Procedures Liver Diseases * Markers Of Liver Diseases * Patterns Of Liver Enzymes And Markers For Interpretation Of Disease * Myocardial And Skeletal Muscle Disease * Pancreatic Diseases • Miscellaneous Enzymes • Suggested Readings * Important ● ● Diagnostic enzymology involves the measurement of enzymes in body fluids for the diagnosis of disease. In most cases, serum or blood levels are the most useful, although urine, cerebrospinal, and extracellular fluid levels are sometimes important. This chapter focuses on the analytical aspects and clinical significance of important enzymes that are measured for diagnostic purposes. ● The major emphasis is on the use of these enzymes for the diagnosis of diseases involving the liver, myocardium, skeletal muscle, pancreas, and bone. In the case of myocardial infarction and skeletal muscle injury, nonenzyme markers such as myoglobin and troponin are also discussed. BASIC CONCEPTS FOR DIAGONOSTIC ENZYMOLOGY Pathologic Role of Enzymes in Blood Pathologic Role of Enzymes in Blood -1 ● Most enzymes that are used for diagnostic purposes have no direct physiologic role in the blood: Their presence under normal circumstances is the result of natural aging and turnover of cells. Pathologic Role of Enzymes in Blood -2 ● ● The normal level of activity of these enzymes in the serum is a function of the rate of release and clearance. The half-lives of these enzymes vary greatly from an estimated 2 hours for the BB isoenzyme of creatine kinase (CK) to 170 hours for placental alkaline phosphatase (ALP). Pathologic Role of Enzymes in Blood -3 ● ● High levels of enzymes in the blood can indicate increased cellular turnover and tissue necrosis caused by disease. An equally important and largely overlooked cause of high enzyme levels in blood is tissue synthesis of new enzymes that occurs in response to disease, induction by various drugs, and carcinogenesis. ENZYME ASSAY PROCEDURES ENZYME ASSAY PROCEDURES ● Single-Reagent Kinetic Assays ● Start Reagent Activity Assays ● Enzyme Activity Calculations ● Mass Measurements Mass Measurements ● These assays are particularly useful for isoenzyme analysis, as antisera can be directed toward specific isoenzymes, isoforms, or subunits. ● Mass measurements are also used to measure the concentration of protein markers (e.g., myoglobin) that do not possess enzymatic activities. LIVER DISEASES LIVER ANATOMY LIVER LIVER DISEASES ● ● The enzymes ALT and AST, ALP, LDH, GGT, and (to a lesser extent) 5'-nucleotidase (5'NT) are commonly measured for the assessment of liver function. None of these markers is specific for any single liver disorder. LIVER DISEASES ● This section covers liver dysfunction, describes individual liver enzymes and their laboratory measurement , and explains how patterns of liver enzyme data can be used to aid in the diagnosis of liver diseases. LIVER DISEASES Inclusion: ● Acute Hepatocellular Injury ● Cholestatic Liver Diseases ● Chronic Liver Diseases ● Alcoholic Liver Disease Liver Diseases -1 Acute Hepatocellular Injury Name of Diseases Markers viral hepatitis Bilirubin AST,ALT Acute liver failure AST,ALT Various substances that can induce acute liver failure Solvents Mushrooms Metals Drugs Metabolic Carbon tetrachloride Trichloroethylene Amanita phalloides Yellow phosphorus Acetaminophen Halothane Isoniazid Rifampicin Reye’s syndrome Wilson’s disease Galactosemia α-Antitrypsin deficiency Liver Diseases -2 Cholestatic Liver Diseases Name of Diseases Intrahepatic Obstruction Extrahepatic Obstruction Markers Bilirubin ALP,GGT,5’-NT Bilirubin ALP,GGT,5’-NT Liver Diseases – 3 Chronic Liver Diseases Name of Diseases Chronic hepatitis Liver Cancer Markers Liver enzymes (in active form) Liver enzymes , AFP Liver Diseases – 4 Alcoholic liver disease Name of Diseases Fatty Liver Alcoholic Cirrhosis Markers Liver enzymes within normal AST, ALT are increased ALP, AST, ALT and GGT are elevated MARKERS OF LIVER DISEASES Specific enzymes of liver ● ALP ( Alkaline Phosphatase) and ALP Isoenzymes ● GGT ( g-glutamyl-peptide : amino acid γ- glutamyltransferase) ● 5'-NT ( 5'-ribonucleotide phosphohydrolase) ● AST ( L-aspartate : 2- oxoglutarate amino- transferase ) ● ALT (L-alanine: 2-oxoglutarate amino-transferase) ALT 20%AST GGT 80% AST ALP Specific enzymes of liver -1 ■ ALP And ALP Isoenzymes Enzyme ALP distribution important indication liver, bone, hepatobiliary disease, Intestine, kidney skeletal disease Adrenals, placenta ALP Isoenzymes liver, bone, Intestine, kidney placenta differentiating between bone and liver sources Plasma alkaline phosphatase activity as a function of age and sex(—men;……, women). Horizontal lines refer to multiples of the adult upper reference limit. Specific enzymes of liver -2 ■ GGT distribution reference indication liver (most) men 9-50 U/L hepatobiliary Prostate (little) women 8-40 U/L diseases Prostate (little) (in 37°C) alcoholism * Located in the cell membrane Specific enzymes of liver -3 ■ 5'-NT distribution indication cytosolic membrane-bound increased activity enzyme that 5'-phosphate in the serum reflects esters of nucleotides. hepatobiliary diseases Specific enzymes of liver -4 ■ ALT and AST distribution reference ALT liver AST liver heart 10-40 U/L 10-40 U/L indication parenchymal diseases of liver AMI parenchymal diseases of liver and skeletal muscle diseases PATTERNS OF LIVER ENZYMES AND MARKERS FOR INTERPRETATION OF DISEASE ● Unlike some disorders such as acute pancreatitis and myocardial infarction, for which there are enzyme markers that are primarily used for one disorder and have high diagnostic efficiencies, there are no enzyme markers that are specific for any single liver disease. ● ● ● When evaluating these disorders, therefore, it is appropriate to consider a panel of markers, sometimes called live function tests (LFTs). usually includes bilirubin, AST, ALT,ALP,and sometimes GGT and 5'NT although these tests can reflect various disease processes in the liver, they do not reflect hepatic reserve for synthesis and metabolic functions Hepatocellular Versus Obstructive Liver Diseases Acute Injury When Acute Hepatocellular Injury : ■ ■ AST and ALT and are therefore rarely used for diagnostic purposes. ALP, GGT, and 5'NT are not as markedly elevated. ALT and AST in acute liver injury -1 disease acute hepatitis enzyme marker ALT and AST elevated>1000U/L (viral or toxic) HAV ALT elevated in 3 to 4 weeks after infection ALT return to normal within 8 to 12 weeks HBV and HCV preclinical incubation phase is longer and ALT and AST may remain normal for 2 to 6months ALT and AST return to normal within 2 to 3months ALT and AST in acute liver injury -2 disease chronic active hepatitis end-stage liver disease enzyme marker ALT and AST elevated 5 to10 fold ALT and AST return to normal or subnormal Markers For Liver Function And Disease -1 Disease or function Markers Function evaluation Normal synthesis capacity Excretory function Albumin, retinol binding protein, prealbumin,prothrombin time, cholinesterase Bilirubin, bile acids, rose bengal and sulfobromophthalein excretion Metabolic function Ammonia, amino acids, serum protein, lipids, electrophoresis,globulins Drug metabolism Antipyrine breath and clearance test, 14CO2 breath test Markers For Liver Function And Disease -2 Disease or function Markers Pathological evaluation Hepatocellular injury ALT, AST,LDH, Obstruction Bilirubin, ALP, GGT,5’-NT bile acids Infections Viral and autoimmune serologies Malignancies Carcinoembryonic antigen, α-fetoprotein Relationship of AST and ALT to ALP and GGT in Hepatitis Cholestasis -1 ● ● The best markers for intrahepatic and extrahepatic cholestasis are ALP, GGT, and 5'NT The largest elevations (four- to 10-fold) of ALP are typically seen in obstruction owing to gallstones or malignancy and in biliary cirrhosis. Cholestasis -2 • AST and ALT are generally only slightly elevated in cholestasis, rarely more than 500 U/L. • Measurement of total and direct bilirubin are also important in making the diagnosis of obstructive jaundice. Multiplies of normal Relationship of AST and ALT to ALP and GGT in Cholestasis De Ritis Ratio (AST/ALT) De Ritis Ratio (AST/ALT) -1 • Further differentiation of specific liver diseases is aided by calculating the ratio of AST to ALT levels. — acute or chronic ? — intra- or extrahepatic ? • recommended by the International Federation of Clinical Chemistry (IFCC) • de Ritis ratio is normally approximately 1.15 ALT versus AST levels in various liver diseases De Ritis(AST/ALT) Disease Acute disorders of the liver acute viral hepatitis infectious mononucleosis chronic disorders of the liver alcoholic liver disease postnecrotic cirrhosis chronic active hepatitis chronic persistent hepatitis -2 AST/ALT <1.0 >1.0 normal De Ritis(AST/ALT) -3 Intrahepatic and Extrahepatic obstruction Disease AST/ALT extrahepatic cholestasis <1.5 intrahepatic cholestasis ≥1.5 Couses acute passage of a stone biliary cirrhosis and malignancy De Ritis(AST/ALT) - 4 Intrahepatic and Extrahepatic obstruction Other laboratory tests: ALP extrahepatic >intrahepatic Conjugated bilirubin extrahepatic >intrahepatic Amylase extrahepatic >intrahepatic Multiplies of normal Relationship of AST and ALT to ALP and GGT in Malignancy De Ritis Ratio (AST/ALT) -5 Alcoholic Liver Disease ● ● Disproportionate increases of AST relative to ALT are observed AST/ALT>6.0 Multiplies of normal Relationship of AST and ALT to ALP and GGT in Alcoholic Live Disease De Ritis Ratio (AST/ALT) -6 Muscle Disease The largest increases of AST relative to ALT are seen in myocardial and skeletal muscle diseases ● ● AST/ALT>10.0 Markers of Alcohol Use Markers of Alcohol • Markers of alcohol use that most widely used marker for alcoholism is GGT • Significant elevations of GGT are also observed after prolonged drinking episodes of several months or more. • it is not a specific test • Other markers currently being studied include carbohydrate-deficient transferrin and fatty acid ethyl esters. MYOCARDIAL AND SKELETAL MUSCLE DISEASE CHD: coronary heart disease UA: unstable angina AMI: acute myocardial infarction Unstable Angina and AMI -1 A: Stable coronary artery plaque not vulnerable for rupture. B: Unstable plaque that is vulnerable for rupturing by shear stresses. Unstable Angina and AMI -2 ● Rupture of this plaque leads to the syndrome of unstable angina, the disease that immediately precedes an AMI. Both conditions, collectively known as acute coronary syndromes, can produce chest pain at rest, lead to specific changes in tile electrocardiogram, and a mild or severe release of enzymes and proteins into blood. ● Congestive Heart Failure ● ● ● Heart failure is a very common disease, Chronic congestive heart failure (CHF) is seen in cardiomyopathies and valve disease. New markers are being developed, such as brain natriuretic peptide (BNP) that might have a role in the management and monitoring of these patients. Skeletal Muscle Disorders ● ● Evidence of high CK activity in the serum is useful for the diagnosis and evaluation of both acute and chronic skeletal muscle diseases. The measurement of enzymes and isoenzymes is useful in the diagnosis of muscle disorders. Enzymes and Proteins Useful in Myocardial Disease Enzymes Useful in Myocardial Disease CK (creatine kinase) -1 The reference range of total CK at 37°C : 38-174U/L for adult men 96-140 U/L for adult women. CK (creatine kinase) -2 CK Isoenzyme Tissue Distribution CK (creatine kinase) -3 CK Isoforms and CK Variants CK (creatine kinase) ● -4 CK and CK Isoenzyme Analytical Measurements ● ● Most normal samples will exhibit a single band owing to CK-MM. Patients with AMI will have high concentrations of CK-MM and MB. CK (creatine kinase) -5 Ck isoforms as measured by agarose electrophoresis CK (creatine kinase) -6 CK Isoenzyme Reference values • CK-MB : Cutoff values for electrophoresis and immunoinhibition are usually set around 5% of total CK or 10 U/L.For immunoassays, decision limits are expressed in mass quantities and are approximately 5 to 10ng/mL. • CK-BB is normally absent in adult serum. • CK-MB and CK-BB levels are higher in children LDH and LDH Isoenzymes LDH (Lactose Dehydrogenase ) Reference The interval for the forward reaction is approximately 80 to 200 U/L at 37°C. approximately 200 to 400 U/L for the reverse reaction. LDH tissue distribution The decision limit most widely used is that LDH1 activity in excess of 40% of total LDH activity supports the diagnosis of AMI. Proteins Useful in Myocardial Disease Myoglobin • found in all skeletal muscle and myocardial tissues • myoglobin was an early marker for AMI • Reference limits for serum myoglobin vary but are generally less than 100 μg/L • Myoglobin is also increased in patients with skeletal muscle disease or injury, and in patients with acute or chronic renal failure. Troponin • Troponin is consists of three isotypes Troponin-T (cTnT) Troponin-I (cTnI ) Troponin C (cTnC) • cTnT and cTnI are better diagnostic markers for AMI than existing enzymes such as CK- MB Use of Cardiac Markers in the Diagnosis of AMI Cardiac Markers in the Diagnosis of AMI -1 ● The diagnosis of AMI is defined by the WHO: ● clinical signs and symptoms ● ● specific changes in electrocardiographic recordings elevated serum enzymes and proteins total CK, CK-MB, LDH, and LDH isoenzymes myoglobin and the cardiac troponins Cardiac Markers in the Diagnosis of AMI -2 ● Cardiac Markers in the Diagnosis of AMI ● ● ● Early Diagnosis: Myoglobin CK Isoforms Definitive Diagnosis : CK-MB Troponin Late Diagnosis : LDH cTnT and cTnI Cardiac Markers in the Diagnosis of AMI -3 Estimates Of Clinical Sensitivity And Specificity Of Diagnostic Tests For AMI Markers Sensitivity 2-8h 8-24h 24-72h >72h Myoglobin CK-MB isoforms CK-MB LDH1 Troponin 95 90 60 40 75 75 60 95 85 95 0 0 98 95 98 0 0 50 90 98 specificity 70 90 95 85 90 Cardiac Markers in the Diagnosis of AMI - 4 Activity versus time curves in serum for biochemical markers of acute myocardial infarction. Cardiac Markers in the Diagnosis of AMI -5 • The cardiac troponins (T or I) are the most efficient markers available today for diagnosis of AMI • The specificity of troponin is also increased over CK-MB or myoglobin • cardiac troponin has been recommended by the NACB as the preferred marker for the definitive diagnosis of AMI • With the development of structural markers such as cTnT and cTnI, the NACB has recommended discontinuance of LDH isoenzymes Release of cardiac troponin from damaged myocytes Enzymes and Proteins in Skeletal Muscle Disease Enzymes and Proteins in Skeletal Muscle Disease • The important enzyme markers of skeletal muscle necrosis include total CK, CK-MB, and, to a lesser extent, AST and aldolase. • In cases of concomitant skeletal muscle injury and AMI, measurement of troponin allows differentiation between skeletal muscle injury and myocardial damage. Enzymes and Proteins in Skeletal MuscleDisease Extensive skeletal muscle injury myoglobin total CK in serum in serum and urine (is observed in patients with rhabdomyolysis) May induce acute renal failure PANCREATIC DISEASES Enzymes of Pancreatic Origin • Amylase versus Marcroamylase • Amylase Isoenzymes (s type and p type) Amylase Isoenzymes Isoforms (S1 and P2 ) • Lipase • Trypsin Clinical Uses of Pancreatic Enzymes In Acute Pancreatitis In Chronic Pancreatitis In Other Disorders Clinical Uses of Pancreatic Enzymes -1 ● In Acute Pancreatitis ● Laboratory findings include an elevated serum amylase, amylase clearance, and lipase. ● Amylase and lipase levels rise within a few hours after onset and remain elevated for 36 to48 hours. ● In Acute Pancreatitis Sensitivity and specificities in Acute Pancreatitis Sensitivity specificities accuracy Amylase Lipase 90% 90 % 40% 60% 95.8% Clinical Uses of Pancreatic Enzymes -2 ● In Chronic Pancreatitis ● ● Serum enzyme levels in chronic pancreatitis are less useful than in the acute presentation. Amylase and lipase levels are very often within normal limits and may actually be low during the end stages of the disease Clinical efficiency of tests in acute and chronic pancreatitis Disorder α-Amylase total pancreatic amylase lipase Clinical sensitivity (%) Acute pancreatitis Chronic pancreatitis Other disorders 79.5 75.0 92.0 Acute pancreatitis pos 29.0 neg 99.4 Chronic pancreatitis pos 13.6 neg 99.5 87.2 81.3 92.5 87.2 81.3 92.1 Predictive values (%) pos 32.4 neg 99.4 pos 31.2 neg 99.4 pos 15.5 neg 99.7 pos 14.8 neg 99.1 Clinical Uses of Pancreatic Enzymes -3 ● In Other Disorders ● ● Injury to or obstruction of surrounding tissue, such as a perforated ulcer or peritonitis, may also cause compression of the pancreas, resulting in enzyme release. Elevations of amylase, immunoreactive trypsin, and, to a lesser extent, lipase also occur in other nonpancreatic disorders. Amylase of high levels are seen in patients with renal failure. ● MISCELLANEOUS ENZYMES MISCELLANEOUS ENZYMES ACP (Acid Phosphatase) CHE (Cholinesterase) ACE (peptidyl-dipeptide hydrolase) G6PD (Glucose-6-Phosphate Dehydrogenase) MISCELLANEOUS ENZYMES -1 ● ACP ● ● Measurement of acid phosphatase was primarily used for monitoring patients with prostatic cancer. With the development of prostate-specific antigen (PSA), assays for acid phosphastase, if used at all, are only used on rare occasions. MISCELLANEOUS ENZYMES - 2 ● CHE ● In the serum, however, only pseudocholinesterase (PCHE) acylcholine acylhydrolase. ● Low levels of PCHE are found in patients with various forms of liver disease. MISCELLANEOUS ENZYMES - 2 ● CHE ● ● Nonhepatic disorders, such as AMI, infections, and pulmonary embolism, have also been shown to decrease PCHE levels. The activity of PCHE is also important in monitoring industrial and agricultural workers who use and are exposed to organophosphate insecticides. MISCELLANEOUS ENZYMES - 3 ● ACE It is produced by the lungs and catalyzes the conversion of the decapeptide angiotensin I to the decapeptide angiotensin II. ● It is a vital enzyme in the control of aldosterone secretion and regulation of blood pressure. ● MISCELLANEOUS ENZYMES - 3 ● ACE It is elevated in approximately 50% to 80% of cases of sarcoidosis, a multisystem granulomatous disease that most commonly involves the lungs. ● ● Several other conditions can produce elevated activities. MISCELLANEOUS ENZYMES - 4 ● G6PD ● It is an important erythrocyte enzyme ● G6PD deficiency affects black men and Whites of Mediterranean descent. ● These individuals develop varying degrees of hemolytic anemias.