* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Physiology Ch 11
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Artificial heart valve wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
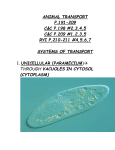
Chapter 11 The Cardiovascular System Anatomy of the Heart cardiovascular system - uses blood to transport oxygen, nutrients, cell wastes, hormones, etc. to and from the cells - the heart provides the force to move the blood heart - approximately the size of a fist - flanked by the lungs apex - end of the heart - points down and to the left - rests on diaphragm base - top of the heart - great vessels emerge here pericardium - double sac (serous membrane) surrounding the heart epicardium - visceral pericardium - hugs external surface of heart - part of heart wall parietal pericardium - outer layer of pericardium fibrous pericardium - fibrous layer which reinforces parietal pericardium - protects and anchors heart serous fluid pericarditis 3 - slippery fluid between pericardial layers - reduces friction as heart beats - inflammation of pericardium - can reduce serous fluid causing pericardial layers to stick (adhesions) Layers of Heart Wall epicardium - visceral pericardium myocardium - bundles of cardiac muscle endocardium - thin sheet of endothelium lining heart chambers chambers of the heart atria - 2 of them left atrium and right atrium (LA and RA) - superior to ventricles - receiving chambers (collect blood) ventricles - 2 of them left ventricle and right ventricle (LV and RV) - thick-walled - discharging chambers (contract and pump blood into circulation) septum - tissue that divides heart into right and left sides (interventricular or interatrial septum) heart - acts as a double pump - right side pumps blood to lungs to pick up O2 - left side pumps blood to rest of body to deliver O2 pulmonary circulation - involves right side of heart - RA receives O2-poor blood from superior vena cava and inferior vena cava - blood flows to RV which pumps blood to lungs through pulmonary trunk - pulmonary trunk divides into right pulmonary artery & left pulmonary artery which bring blood to lungs - O2 is picked up and CO2 is unloaded - blood flows back to left side of heart (LA) through pulmonary veins systemic circulation - involves left side of heart - O2-rich blood flows from LA to LV - LV pumps blood through the aorta from which systemic arteries branch to supply all body tissues (LV is thicker chamber than RV) - O2-poor blood flows through systemic veins to superior or inferior vena cava and then to RA valves - allow blood to flow in only 1 direction through heart atrioventricular (AV) valves bicuspid or mitral valve tricuspid valve semilunar valves pulmonary valve aortic valve atrioventricular (AV) valves bicuspid or mitral valve tricuspid valve chordae tendineae semilunar valves pulmonary valve aortic valve - between atria & ventricles - prevent backflow into atria when ventricles contract - open during ventricular relaxation - closed during ventricular contraction - left AV valve - 2 flaps of endocardium - right AV valve - 3 flaps of endocardium - tiny white cords anchoring flaps to ventricle walls - between ventricles & 2 large vessels leaving the ventricles - prevent arterial blood from reentering heart - open during ventricular contraction - closed during ventricular relaxation - between RV and pulmonary trunk - between LV and aorta coronary circulation coronary arteries cardiac veins - right and left coronary arteries branch off of the aorta - bring blood to nourish the myocardium - drain the myocardium - empty into a vessel on back of heart (coronary sinus) which then empties into RA angina pectoris - crushing chest pain which occurs when myocardium is deprived of O2 myocardial infarction - death of heart cells deprived of oxygen - AKA heart attack Physiology of the Heart intrinsic conduction system sinoatrial (SA) node - AKA nodal system - regulates heart activity - causes muscle contraction to occur in 1 direction (from atria to ventricles) - causes heart to beat about 75 times per minute - in RA - starts each heartbeat, sets pace for the heart - often called the pacemaker - impulse then spreads through atria to atrioventricular (AV) node, through AV bundle, through the bundle branches (in interventricular septum), and finally through the Purkinje fibers (in ventricle walls) SA node AV node AV bundle bundle branches Purkinje fibers tachycardia bradycardia - rapid heart rate (>100 beats per minute) - slower heart rate than normal (<60 beats per minute) systole - ventricular contraction diastole - ventricular relaxation cardiac cycle - events of 1 complete heartbeat a) mid-to-late diastole - heart completely relaxed - pressure in heart is low - blood flows into ventricles from atria - AV valves are open; semilunar valves are closed - then atria contract forcing rest of blood into ventricles b) ventricular systole - ventricles contract (atria are relaxed & fill with blood) - pressure in ventricles increases rapidly - AV valves are forced closed, semilunar valves open - blood leaves ventricles c) early diastole - ventricles relax - semilunar valves close - pressure in ventricles drops - AV valves open - ventricles fill with blood again heart sounds - “lub-dup” first sound (lub) second sound (dup) AV valves closing semilunar valves closing heart murmurs - abnormal heart sounds - often indicate valve problems - if a valve doesn’t close tightly, a swishing sound is heard when the valve closes due to backflow of blood stroke volume - amount of blood pumped out by a ventricle with each heartbeat - about 70 ml/beat cardiac output - amount of blood pumped out by each side of the heart in 1 minute - product of heart rate (HR) and stroke volume (SV) CO = HR x SV example: CO = 75 beats minute x 70 mL = 5250 mL/min beat - varies with demands of the body - increases when HR or SV increase, and drops when HR or SV decrease physical factors affecting heart rate age - HR decreases with age gender - HR faster in females; 72-80 vs. 64-72 in males body temperature - heat increases HR by increasing metabolic rate of heart cells - cold decreases HR exercise - HR increases (nervous system triggers and also muscles generate heat) congestive heart failure - decreases pumping efficiency of heart - often caused by weakening of heart due to coronary atherosclerosis (fatty buildup in coronary arteries), high blood pressure, or multiple heart attacks pulmonary edema - due to failure of left side of the heart - blood backs up into lungs causing blood vessels to swell - fluid leaks from vessels into lung tissue peripheral congestion - due to failure of the right side of the heart - blood backs up in systemic circulation - edema (swelling) occurs most noticeable in feet, ankles, fingers Blood Vessels vascular system arteries arterioles capillaries venules veins - closed transport system made up of blood vessels - blood vessels leaving the heart (carry blood away from heart) - branch into smaller and smaller arteries - smallest arteries - branch into capillaries - smallest blood vessels - form capillary beds in tissues - exchange of materials occurs between tissue cells and blood - drained by venules - smallest veins - join to form veins -drain tissues and return blood to heart - empty into vena cavae which enter the heart walls of arteries and veins have 3 layers: tunica intima - thin inner layer of endothelium - lines interior of vessels tunica media - middle layer - mostly smooth muscle and elastic tissue - vessels constrict or dilate to increase or decrease blood pressure tunica externa - outer layer - mostly fibrous connective tissue - supports & protects vessels arteries - thickest walls of all the blood vessels (especially tunica media) veins - thinner walls - blood often flows against gravity - larger veins have valves to prevent backflow - contraction of skeletal muscles also helps blood return to heart capillaries - walls 1 cell layer thick (only tunica intima) - exchanges made between blood and tissue cells - form networks called capillary beds microcirculation - circulation through a capillary bed varicose veins - common in people who stand for long periods, in obese people, and pregnant women - blood pools in legs due to insufficient venous return of blood - veins become twisted and dilated aorta - largest artery of the body (about size of garden hose) - ascending aorta - part of aorta rising upward from LV aortic arch - ascending aorta arches to the left thoracic aorta - aorta plunges downward through thorax abdominal aorta - aorta passes through diaphragm into abdominopelvic cavity iliac arteries - final branches of abdominal aorta - 1 supplies each leg a few more arteries: carotid arteries axillary arteries radial arteries femoral arteries popliteal arteries dorsalis pedis artery -supply head - run through armpits - supply forearm - supply thighs - run through back of knee - supplies dorsum of foot superior vena cava - veins draining head and arms empty here inferior vena cava - veins draining lower body empty here Physiology of Circulation pulse - pressure waves caused by the expansion and recoil of an artery with each beat of the LV - equal to heart rate - averages 70 – 76 beats/min in a resting person pressure points - areas where arteries are close to surface - pulses can be palpated here - also pressure can be applied here to stop blood flow to distal tissues during hemorrhage blood pressure - pressure blood exerted against the inner walls of blood vessels - highest in large arteries and drops throughout the circulatory pathway - reaches zero at the vena cava - if a vein is cut blood flows evenly from the wound - if an artery is cut blood leaves in rapid spurts systolic blood pressure - pressure in the arteries at the peak of ventricular contraction diastolic blood pressure - pressure when ventricles are relaxing blood pressure - given in millimeters of mercury (mm Hg) - systolic pressure given before diastolic (example: 120/80) peripheral resistance - amount of friction encountered by blood as it flows through blood vessels - may be increased by narrowing of blood vessels by nervous system or atherosclerosis, by increased blood volume, or by increased blood thickness rise in blood pressure - may be caused by anything that increases cardiac output or peripheral resistance - examples: age weight time of day exercise body position emotional state drugs hypertension - high blood pressure - chronic hypertension strains heart and damages arteries - myocardium may enlarge as heart pumps against increased resistance - when strained too much, heart weakens and becomes “flabby” - damage to blood vessels speeds up atherosclerosis primary (essential) hypertension - no specific cause found (90% of cases) factors thought to be involved in hypertension: hypotension diet (high cholesterol, saturated fat, sodium) obesity heredity race stress - low blood pressure - usually systolic pressure below 100 mm Hg - usually no cause for concern coronary artery disease - filling of blood vessels with calcified fatty deposits - diet is most important contributing factor - risk is lowered if people eat less animal fat, cholesterol, and salt - other preventative measures: avoid stress don’t smoke exercise