* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download laboratory science
Survey
Document related concepts
Transcript
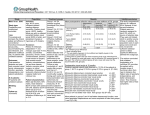
laboratory science Blue light-absorbing intraocular lens and retinal pigment epithelium protection in vitro Janet R. Sparrow, PhD, Ashley S. Miller, Jilin Zhou, MD Purpose: To compare the Alcon AcrySof威 Natural (SN60AT) and AcrySof (SA60AT), the AMO Sensar威 (AR40e) and ClariFlex威, and the Pfizer CeeOn威 Edge 911A intraocular lenses (IOLs) as to their ability to protect retinal pigment epithelial (RPE) cells from light damage mediated by the lipofuscin fluorophore A2E. Setting: Department of Ophthalmology, Columbia University, New York, New York, USA. Methods: Cultured human RPE cells (ARPE-19 cell line) that had accumulated A2E were exposed to blue (430 nm ⫾ 30), green (550 ⫾ 10 nm), or white (390 to 750 nm) light with and without an IOL in the light path. Results: The blue light-absorbing AcrySof Natural IOL was associated with significant reduction (78% to 82%; P⬍.01) in the death of A2E-laden RPE that were exposed to blue, white, and green light. The decrease in the incidence of cell death was greater in magnitude than would be expected from the amount of light that was absorbed by the IOL. The considerably smaller declines in cell death observed with the AcrySof, Sensar, ClariFlex, and CeeOn Edge IOLs were likely due to nonspecific reductions in light transmittance. Conclusions: By absorbing blue light, the AcrySof Natural IOL shields RPE cells that have accumulated the aging lipofuscin fluorophore A2E from the damaging effects of light. A long-term population-based clinical trial would determine whether a blue light-absorbing IOL can reduce the risk for or progression of age-related macular degeneration. J Cataract Refract Surg 2004; 30:873–878 2004 ASCRS and ESCRS T he design of intraocular lenses (IOLs) should be based on the properties of the human ocular lens, especially in the transmission properties of the IOL. Notably, the human crystalline lens absorbs most ultraviolet light between 300 nm and 400 nm.1 Thus, to provide the same protection to the retina afforded by the natural lens, the use of ultraviolet light-absorbing IOLs became the standard of practice once these lenses were developed.2–8 However, the transmission properties of most IOLs are not comparable to those of the natural Accepted for publication January 27, 2004. Reprint requests to Janet R. Sparrow, PhD, Department of Ophthalmology, Columbia University, 630 West 128th Street, New York, New York 10032, USA. email: [email protected]. 2004 ASCRS and ESCRS Published by Elsevier Inc. human lens, since the latter yellows with age while IOLs in current use are colorless.2,9–13 The color change in the natural lens is likely attributable to oxidation products of tryptophan (n-formyl-kynurenine) and to glycosylation of lens proteins.14 It results in a progressive increase in absorbance within the blue range of the visible spectrum.2,9 Filtering the shorter wavelengths of the visible spectrum is particularly significant because it is also this portion of the spectrum that produces photochemical damage to the retinal pigment epithelium (RPE).15–17 It is now generally accepted that at least 1 of the intracellular chromophores responsible for the blue light sensitivity of RPE cells18,19 is the lipofuscin constituent A2E.20–22 This fluorophore is unique to RPE cells and 0886-3350/04/$–see front matter doi:10.1016/j.jcrs.2004.01.031 LABORATORY SCIENCE: BLUE LIGHT-ABSORBING IOL has been shown to accumulate in human RPE cells throughout the lifetime of an individual, with levels being highest in the aged eye.21 Thus, replacement of a senile cataractous crystalline lens with a colorless IOL may leave the RPE vulnerable at an age when its content of blue light sensitive A2E is already high. The RPE fluorophore A2E is maximally excited by light in the blue region of the spectrum.18 When irradiated, A2E generates singlet oxygen that proceeds to add to carbon–carbon double bonds of A2E to generate highly reactive epoxides (A2E-epoxides) along the sidearms of the molecule.23, 24 The cellular injury induced by the illumination of A2E-laden RPE includes oxidative DNA base changes,25,26 and it is likely that as electrophiles that can readily react with many cellular molecules, A2E-epoxides may account for much of the cellular damage accrued.25 The photochemical events provoked by the irradiation of A2E-laden RPE ultimately result in the initiation of a cell death program. The sensitivity to blue light conferred by the lipofuscin fluorophore A2E may explain why atrophic age-related macular degeneration (AMD) has been linked to both RPE lipofuscin27–33 and cumulative light exposure.34 Moreover, the loss of RPE cells in atrophic AMD is a critical event as it leads to photoreceptor cell degeneration. Given that the attenuation of blue light afforded by the yellowed senescent lens may defend lipofuscinfilled RPE cells against blue light damage, we are interested in efforts being made to develop IOLs that replicate the transmission characteristics of the aging crystalline lens. In this study, we constructed a cell culture system that allowed us to compare several IOLs as to their ability to protect A2E-laden RPE from blue light damage. In this cell culture system, A2E accumulates in the lysosomal compartment of a human RPE cell line, as it does in RPE of the eye.35 Moreover, the levels of A2E are comparable to the level occurring in vivo.18,35 This model also allows us to study RPE cells with and without intracellular deposits of A2E. Materials and Methods The IOLs studied were the Alcon AcrySof威 Natural (SN60AT) (acrylic, 20.0 diopters [D], 6.0 mm optic diameter) and AcrySof (SA60AT) (acrylic, 20.0 D, 6.0 mm optic diameter); the AMO ClariFlex威 (CLRFLXB) (silicone, 20.0 D, 6.0 mm optic diameter) and Sensar威 (AR40e) (acrylic, 20.0 D, 6.0 mm optic diameter); and the Pharmacia 874 CeeOn威 Edge (911A) (silicone, 20.0 D, 6.0 mm optic diameter). A2E Accumulation in Culture Human RPE cells (ARPE-19, American Type Culture Collection), which are devoid of endogenous A2E,35 were grown in 8-well, plastic chamber slides (Laboratory-Tek, Nunc), as described.35 Once confluent, the cells were allowed to accumulate synthesized A2E21 from a 20 M concentration added to the medium. With this protocol, A2E accumulates in the lysosomal compartment of the cells to levels that are comparable to amounts present in vivo.18,35 Illumination and Placement of the IOL Immediately before illumination, the culture medium was replaced with phosphate-buffered saline containing calcium, magnesium, and glucose. For quantitative measurements of light-induced cell death, the cells were exposed to blue light (430 nm ⫾ 30 [SD], 8 mW/cm2), green light (550 ⫾ 10 nm, 8 mW/cm2), or white light (246 mW/cm2) over a 0.8 mm ⫻ 8.5 mm field. The light was delivered from a tungsten halogen source for 20 minutes, and power was measured with a Newport optical power meter (model 840). The spectral range of the lamp was 390 to 750 nm, with a lower output at the shorter wavelengths. The IOL to be tested was applied to the undersurface of the culture well, where it remained attached, unaided. It was centered over the light path. To obtain a visual representation of IOL protection, 1.0 mm diameter disks were cut from the center of the IOL using a trephine blade (Katena Products, Inc.). The IOL disks were positioned on the undersurface of the well, which was then irradiated (430 ⫾ 30 nm, 16 mW/cm2) from below. Detection of Nonviable Cells The nuclei of dead RPE cells were labeled with a membrane impermeant dye (Dead Red, Molecular Probes), and the nuclei of all cells with 4⬘,6⬘-diamino-2-phenylindole (DAPI), as reported.25,26 Blue light-illuminated A2E-containing RPE labeled in this way are undergoing an apoptotic form of cell death.36 Digital images (5 fields per illumination zone) were obtained using a Zeiss Axioplan II microscope with Axiocam camera and KS400 image processing software. Subsequently, Dead Red and DAPI-stained nuclei were counted. Dead cells were quantified as a percentage of the total number of cells in a field. Means are based on 3 experiments. Statistical analysis was by an analysis of variance followed by the Newman-Keul multiple comparison test (Prism, GraphPad Software). A P value of 0.05 or less was considered significant. J CATARACT REFRACT SURG—VOL 30, APRIL 2004 LABORATORY SCIENCE: BLUE LIGHT-ABSORBING IOL Figure 1. (Sparrow) Quantitation of nonviable RPE cells after A2E accumulation and blue light illumination (430 nm) with and without an IOL placed in the light path. The percentage of nonviable cells was determined by labeling all nuclei with DAPI and the nuclei of nonviable cells with a membrane-impermeable dye. The data were normalized to the percentage of nonviable cells in the absence of an IOL. Values are mean ⫾ SEM. Figure 2. (Sparrow) A blue light-absorbing IOL protects A2Eladen RPE from cell death due to 430 nm irradiation. The nuclei of nonviable RPE were labeled with a membrane impermeable dye (left), and all nuclei were stained with DAPI (right). The left and right panels are corresponding fields of illuminated A2E-laden RPE. In the absence of an IOL in the light path (top), the entire field is covered with nonviable cells. Placement of a blue light-absorbing IOL (1.0 mm diameter disk; AcrySof Natural) in the light path reduced the number of nonviable cells in a circular zone corresponding to the area covered by the IOL (bottom, dotted circle). Results Using a fluorescence assay that labels the nuclei of nonviable cells, it was observed that illuminated RPE that did not contain A2E (no A2E, no IOL) remained viable, while blue light-illuminated (430 nm peak with a bandwidth of 60 nm, 8 mW/cm2) RPE that had previously accumulated A2E underwent marked cell death. In the present experiments, 41.1% ⫾ 4.1% (3 experiments) of the A2E-laden cells in a field of illumination became nonviable after blue light exposure in the absence of an IOL (Figure 1). When the yellowtinted AcrySof Natural IOL was placed in the center of the light path, transmission of the 430 nm light was reduced by approximately 50% and cell death was reduced by 80% (P⬍.001) compared to irradiation in the absence of an IOL (Figure 1). When the AcrySof, Sensar, ClariFlex, or CeeOn Edge IOLs were in place, the frequency of nonviable cells was not different (P⬎.05) than cell death in the absence of an IOL. The modest but consistent declines in cell death that were detected with these IOLs (Figure 1) were undoubtedly due to the small reductions in light transmission (⬃5%) that were measured. The ability of the AcrySof Natural IOL to attenuate blue light-mediated cell death was evident when fields of irradiated cells were imaged. In the absence of an IOL, the nuclei of nonviable cells were uniformly distributed across the illuminated field (Figure 2). Conversely, placement of the blue light-absorbing AcrySof Natural IOL (a 1.0 mm disk) within the light path spared a circular zone of cells, the diameter of this area corresponding to the diameter of the IOL disc. Within this sector, all nuclei were labeled with DAPI but labeled nuclei of nonviable cells were only occasionally observed. With the use of wide-band white light (390 to 750 nm; 246 mW/cm2) that included all wavelengths toward which A2E exhibits sensitivity, the death of A2E-laden RPE reached a frequency of 35% (35.4% ⫾ 2.7% of the cells in an illumination zone; 3 experiments). In the presence of the blue light-absorbing AcrySof Natural IOL, cell death from white light was reduced by 82% (P⬍.001) compared to that without an IOL (Figure 3). In comparison, the AcrySof IOL diminished the incidence of nonviable cells by 22% (P⬍.05); with the Sensar, ClariFlex, and CeeOn Edge IOLs, cell death was decreased by 37% to 39% (P⬍ .01). Again, the decreases observed with the colorless IOLs were likely related to the reductions in spectral transmittance associated with all IOLs. When compared with blue and white light, green light (550 ⫾ 20 nm) delivered at an intensity that was J CATARACT REFRACT SURG—VOL 30, APRIL 2004 875 LABORATORY SCIENCE: BLUE LIGHT-ABSORBING IOL Figure 3. (Sparrow) Quantitation of nonviable cells after white light Figure 4. (Sparrow) Quantitation of nonviable cells after green light (390 to 750 nm) illumination of A2E-laden RPE with and without the indicated IOL placed in the light path. The percentage of nonviable cells was normalized to values obtained in the absence of an IOL. Values are mean ⫾ SEM. illumination (550 nm) of A2E-laden RPE with and without the indicated IOL placed in the light path. Values for percentage of nonviable cells were normalized to values obtained in the absence of an IOL. Means ⫾ SEM are presented. the same as that of the blue light (8 mW/cm2) induced the death of only a small number of A2E-laden RPE cells (2.9% ⫾ 0.6%; 3 experiments). With green light irradiation, all IOLs reduced the death of RPE that had accumulated A2E (Figure 4). With the AcrySof Natural, the number of nonviable cells was decreased by 78% (P⬍.01) compared to cell death without an IOL; while cell death declined by 33% with the AcrySof (P⬎.05) and by 52% to 57% (P⬍.05) with the Sensar, ClariFlex, and CeeOn Edge IOLs. with the other IOLs were probably due to IOL-associated nonspecific decreases (5% to 10%) in light transmission that have been reported.2,7,8,37 The AcrySof Natural IOL did not completely abolish cell death in this model. However, this is not surprising since by design, this IOL does not block all blue light. Rather, the yellow tint of the lens is intended to confer a spectral transmission similar to that of the crystalline lens of an adult.1 That A2E-containing RPE are less sensitive than to green light is to be expected: A2E has an excitation maximum of approximately 430 nm with the emission elicited at 550 nm being less than 5% of that elicited at 430 nm.18 Ham et al.15 were the first investigators to demonstrate that retinal injury from wavelengths that peak around 425 nm is initiated by photochemical processes in the RPE. The action spectrum of this damage corresponds to the absorption spectrum of the aging fluorophore A2E,18 and there is now an abundance of experimental evidence that A2E is a sensitizing molecule that can mediate light injury to RPE, leading to RPE atrophy.18,23,25,26,36 Since lipofuscin fluorophores, including A2E, accumulate with age, the natural yellowing of the aging human lens is fortunate as it may dampen the damaging potential of short wavelength blue light. For some time, it has been postulated that cumulative photochemical damage from lifetime exposures to light are a cause of AMD,38 although the results of Discussion The study shows that by absorbing predominantly in the blue region of the spectrum, the AcrySof Natural IOL shields RPE cells that have accumulated the lipofuscin fluorophore A2E from the damaging effects of light. The protection afforded by the AcrySof Natural IOL was pronounced for wide-band white light just as it was for narrow-band blue light. The reduction in cell death afforded by this blue light-filtering IOL was greater in magnitude than would be expected from the decline in transmitted blue light. That a reduction in blue light transmission of approximately 50% resulted in an 80% decline in cell death probably occurred because blue light levels were brought below the threshold for lethal damage for a significant proportion of the cells. Small but consistent declines in cell death observed 876 J CATARACT REFRACT SURG—VOL 30, APRIL 2004 LABORATORY SCIENCE: BLUE LIGHT-ABSORBING IOL epidemiological studies are inconclusive.39,40 Nevertheless, it is of interest that the Chesapeake Bay Waterman Study reported an association between the incidence of advanced AMD and blue light exposure during the 20year period that preceded the study.34 Other reports suggest a relationship between the incidence of AMD and cataract extraction. For instance, the National Health and Nutrition Survey observed 3087 patients between 1970 and 1974 and reports that aphakic subjects had an increased risk for developing AMD.41 In a study of 47 patients who presented with bilateral drusen and pigmentary changes, choroidal neovascularization was observed in 19.1% of the eyes that had had cataract extraction with implantation of a colorless IOL compared with an incidence of 4.3% in the fellow phakic eyes.42 The Beaver Dam Study comprised 4926 patients from 1988 to 1990 and found a positive association between cataract extraction and clinical indications of early AMD.43 Indeed, both the 5-year and 10-year follow-up studies confirm that eyes that had had cataract surgery before baseline evaluation were more likely to exhibit progression of AMD.44,45 Nevertheless, similar associations were not reported by the Age-Related Eye Disease Study (DF Martin, ARVO abstract 1907, 2002). Circumstances that lead to damage in the aging RPE cell are considered as a prelude to the photoreceptor cell degeneration that characterizes the visual impairment associated with AMD. We speculate that a yellow-tinted IOL that simulates the adult natural lens and protects lipofuscin-containing RPE from blue light damage may reduce the risk for or progression of AMD. This concept warrants evaluation by a long-term population-based clinical study. References 1. Boettner EA, Wolter JR. Transmission of the ocular media. Invest Ophthalmol 1962; 1:776–783 2. Lindstrom RL, Doddi N. Ultraviolet light absorption in intraocular lenses. J Cataract Refract Surg 1986; 12:285–289 3. Komatsu M, Kanagami S, Shimizu K. Ultravioletabsorbing intraocular lens versus non-UV-absorbing intraocular lens: comparison of angiographic cystoid macular edema. J Cataract Refract Surg 1989; 15:654– 657 4. Werner JS, Hardenbergh FE. Spectral sensitivity of the pseudophakic eye. Arch Ophthalmol 1983; 101:758– 760 5. Lawrence HM, Reynolds TR. Erythropsial phototoxicity associated with nonultraviolet-filtering intraocular lenses. J Cataract Refract Surg 1989; 15:569–572 6. Peyman GA, Zak R, Sloane H. Ultraviolet-absorbing pseudophakos: an efficacy study. Am Intra-Ocular Implant Soc J 1983; 9:161–170 7. Hammer HM, Yap M, Weatherill JR. Visual performance in pseudophakia with standard and ultravioletabsorbing intraocular lenses: a preliminary report. Trans Ophthalmol Soc U K 1986; 105:441–446 8. Mainster MA. The spectra, classification, and rationale of ultraviolet-protective intraocular lenses. Am J Ophthalmol 1986; 102:727–732 9. Mellerio J. Yellowing of the human lens: nuclear and cortical contributions. Vis Res 1987; 27:1581–1587 10. Weale RA. Human lenticular fluorescence and transmissivity, and their effects on vision. Exp Eye Res 1985; 41:457–473 11. Gaillard ER, Zheng L, Merriam JC, Dillon J. Age-related changes in the absorption characteristics of the primate lens. Invest Ophthalmol Vis Sci 2000; 41:1454–1459 12. Weale RA. Aging and vision. Vis Res 1986; 26:1507– 1512 13. Weale RA. Age and the transmittance of the human crystalline lens. J Physiol 1988; 395:577–587 14. Chylack LT Jr. Aging changes in the crystalline lens and zonules. In: Albert DM, Jakobiec FA, eds, Principles and Practice of Ophthalmology. Basic Sciences. Philadelphia, PA, WB Saunders Co, 1994; 702–710 15. Ham WT Jr, Mueller HA, Ruffolo JJ Jr, et al. Basic mechanisms underlying the production of photochemical lesions in the mammalian retina. Curr Eye Res 1984; 3:165–174 16. Ham WT Jr, Ruffolo JJ Jr, Mueller HA, et al. Histologic analysis of photochemical lesions produced in rhesus retina by short-wavelength light. Invest Ophthalmol Vis Sci 1978; 17:1029–1035 17. Ham WT Jr, Allen RG, Feeney-Burns L, et al. The involvement of the retinal pigment epithelium (RPE). In: Waxler M, Hitchens VM, eds, Optical radiation and Visual Health. Boca Raton, FL, CRC Press, 1986; 43–67 18. Sparrow JR, Nakanishi K, Parish CA. The lipofuscin fluorophore A2E mediates blue light-induced damage to retinal pigmented epithelial cells. Invest Ophthalmol Vis Sci 2000; 41:1981–1989 19. Schütt F, Davies S, Kopitz J, et al. Photodamage to human RPE cells by A2-E, a retinoid component of lipofuscin. Invest Ophthalmol Vis Sci 2000; 41:2303– 2308 20. Eldred GE, Lasky MR. Retinal age pigments generated by self-assembling lysosomotropic detergents. Nature 1993; 361:724–726 21. Parish CA, Hashimoto M, Nakanishi K, et al. Isolation and one-step preparation of A2E and iso-A2E, fluoro- J CATARACT REFRACT SURG—VOL 30, APRIL 2004 877 LABORATORY SCIENCE: BLUE LIGHT-ABSORBING IOL 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 878 phores from human retinal pigment epithelium. Proc Natl Acad Sci USA 1998; 95:14609–14613 Sakai N, Decatur J, Nakanishi K, Eldred GE. Ocular age pigment “A2E”: an unprecedented pyridinium bisretinoid. J Am Chem Soc 1996; 118:1559–1560 Sparrow JR, Zhou J, Ben-Shabat S, et al. Involvement of oxidative mechanisms in blue-light-induced damage to A2E-laden RPE. Invest Ophthalmol Vis Sci 2002; 43:1222–1227 Ben-Shabat S, Itagaki Y, Jockusch S, et al. Formation of a nonaoxirane from A2E, a lipofuscin fluorophore related to macular degeneration, and evidence of singlet oxygen involvement. Angew Chem Int Ed Engl 2002; 41:814–817 Sparrow JR, Vollmer-Snarr HR, Zhou J, et al. A2Eepoxides damage DNA in retinal pigment epithelial cells. Vitamin E and other antioxidants inhibit A2E-epoxide formation. J Biol Chem 2003; 278:18207–18213 Sparrow JR, Zhou J, Cai B. DNA is a target of the photodynamic effects elicited in A2E-laden RPE by bluelight illumination. Invest Ophthalmol Vis Sci 2003; 44: 2245–2251 Weiter JJ, Delori FC, Wing GL, Fitch KA. Retinal pigment epithelial lipofuscin and melanin and choroidal melanin in human eyes. Invest Ophthalmol Vis Sci 1986; 27:145–152 Wing GL, Blanchard GC, Weiter JJ. The topography and age relationship of lipofuscin concentration in the retinal pigment epithelium. Invest Ophthalmol Vis Sci 1978; 17:601–607 Delori FC, Dorey CK, Staurenghi G, et al. In vivo fluorescence of the ocular fundus exhibits retinal pigment epithelium lipofuscin characteristics. Invest Ophthalmol Vis Sci 1995; 36:718–729 Delori FC, Goger DG, Dorey CK. Age-related accumulation and spatial distribution of lipofuscin in RPE of normal subjects. Invest Ophthalmol Vis Sci 2001; 42: 1855–1866 von Rückmann A, Fitzke FW, Bird AC. Fundus autofluorescence in age-related macular disease imaged with a laser scanning ophthalmoscope. Invest Ophthalmol Vis Sci 1997; 38:478–486 Holz FG, Bellmann C, Margaritidis M, et al. Patterns of increased in vivo fundus autofluorescence in the junctional zone of geographic atrophy of the retinal pigment epithelium associated with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 1999; 237: 145–152 Holz FG, Bellman C, Staudt S, et al. Fundus autofluorescence and development of geographic atrophy in agerelated macular degeneration. Invest Ophthalmol Vis Sci 2001; 42:1051–1056 34. Taylor HR, West S, Muñoz B, et al. The long-term effects of visible light on the eye. Arch Ophthalmol 1992; 110:99–104 35. Sparrow JR, Parish CA, Hashimoto M, Nakanishi K. A2E, a lipofuscin fluorophore, in human retinal pigmented epithelial cells in culture. Invest Ophthalmol Vis Sci 1999; 40:2988–2995 36. Sparrow JR, Cai B. Blue light-induced apoptosis of A2Econtaining RPE: involvement of caspase-3 and protection by Bcl-2. Invest Ophthalmol Vis Sci 2001; 42: 1356–1362 37. Mainster MA. Spectral transmittance of intraocular lenses and retinal damage from intense light sources. Am J Ophthalmol 1978; 85:167–170 38. Mainster MA. Light and macular degeneration: a biophysical and clinical perspective. Eye 1987; 1:304–310 39. Darzins P, Mitchell P, Heller RF. Sun exposure and agerelated macular degeneration; an Australian case-control study. Ophthalmology 1997; 104:770–776 40. Cruickshanks KJ, Klein R, Klein BEK. Sunlight and age-related macular degeneration; the Beaver Dam Study. Arch Ophthalmol 1993; 111:514–518 41. Liu IY, White L, LaCroix AZ. The association of agerelated macular degeneration and lens opacities in the aged. Am J Public Health 1989; 79:765–769 42. Pollack A, Marcovich A, Bukelman A, Oliver M. Agerelated macular degeneration after extracapsular cataract extraction with intraocular lens implantation. Ophthalmology 1996; 103:1546–1554 43. Klein R, Klein BEK, Wang Q, Moss SE. Is age-related maculopathy associated with cataracts? Arch Ophthalmol 1994; 112:191–196 44. Klein R, Klein BEK, Jensen SC, Cruickshanks KJ. The relationship of ocular factors to the incidence and progression of age-related maculopathy. Arch Ophthalmol 1998; 116:506–513 45. Klein R, Klein BEK, Wong TY, et al. The association of cataract and cataract surgery with the long-term incidence of age-related maculopathy. Arch Ophthalmol 2002; 120:1551–1558 From the Department of Ophthalmology, Columbia University, New York, New York 10032, USA. None of the authors has a financial or proprietary interest in any product mentioned. Presented at the XXI Congress of the European Society of Cataract and Refractive Surgeons, Munich, Germany, September 2003. Supported by grants from Alcon Laboratories, Ft. Worth, Texas; the National Eye Institute (EY 12951), Bethesda, Maryland; and by unrestricted funds from Research to Prevent Blindness, New York, New York, USA. J CATARACT REFRACT SURG—VOL 30, APRIL 2004