* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CV-4-2014
Haemodynamic response wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Common raven physiology wikipedia , lookup
Hemodynamics wikipedia , lookup
Synaptic gating wikipedia , lookup
End-plate potential wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Cushing reflex wikipedia , lookup
Electrocardiography wikipedia , lookup
Pre-Bötzinger complex wikipedia , lookup
Homeostasis wikipedia , lookup
Circulatory system wikipedia , lookup
Vasopressin wikipedia , lookup
Microneurography wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
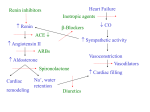
Cardiovascular Physiology Qiang XIA (夏强), MD & PhD Department of Physiology Room C518, Block C, Research Building, School of Medicine Tel: 88208252 Email: [email protected] Regulation of Cardiovascular Activities Lecture Outline •Nervous Regulation •Humoral Regulation •Autoregulation Nervous Regulation Innervation of cardiovascular system Nervous regulation of the circulation Cardiac mechanisms of norepinephrine Mechanisms of norepinephrine —increase Na+ & Ca2+ permeability • If , phase 4 spontaneous depolarization, autorhythmicity • Ca2+ influx , phase 0 amplitude & velocity , conductivity • Ca2+ influx , Ca2+ release , [Ca2+ ]i , contractility Asymmetrical innervation of sympathetic nerve Cardiac mechanisms of acetylcholine Mechanisms of acetylcholine —increase K+ & decrease Ca2+ permeability • K+ outward , |MRP| , phase 4 spontaneous depolarization , autorhythmicity • Inhibition of Ca2+ channel, phase 0 amplitude & velocity , conductivity • Ca2+ influx , [Ca2+ ]i , contractility Cardiac effect of parasympathetic stimulation Interaction of sympathetic and parasympathetic nerves Predominance of autonomic nerves Cardiovascular Center A collection of functionally similar neurons that help to regulate HR, SV, and blood vessel tone Vasomotor center Located bilaterally mainly in the reticular substance of the medulla and of the lower third of the pons – Vasoconstrictor area – Vasodilator area – Cardioinhibitor area – dorsal nuclei of the vagus nerves and ambiguous nucleus – Sensory area – tractus solitarius Vasomotor center Higher cardiovascular centers – Reticular substance of the pons – Mesencephalon – Diencephalon – Hypothalamus – Cerebral cortex – Cerebellum Baroreceptor Reflexes • Arterial baroreceptors – Carotid sinus receptor – Aortic arch receptor • Afferent nerves (Buffer nerves) • Cardiovascular center: medulla • Efferent nerves: cardiac sympathetic nerve, sympathetic constrictor nerve, vagus nerve • Effector: heart & blood vessels Baroreceptor neurons function as sensors in the homeostatic maintenance of MAP by constantly monitoring pressure in the aortic arch and carotid sinuses. Characteristics of baroreceptors: Sensitive to stretching of the vessel walls Proportional firing rate to increased stretching Responding to pressures ranging from 60180 mmHg Receptors within the aortic arch are less sensitive than the carotid sinus receptors The action potential frequency in baroreceptor neurons is represented here as being directly proportional to MAP. i.e., MAP is above homeostatic set point i.e., reduce cardiac output Baroreceptor neurons deliver MAP information to the medulla oblongata’s cardiovascular control center (CVCC); the CVCC determines autonomic output to the heart. Reflex pathway Typical carotid sinus reflex Physiological Significance Maintaining relatively constant arterial pressure, reducing the variation in arterial pressure Humoral Regulation • Vasoconstrictor agents • Vasodilator agents Renin-angiotensin system Juxtaglomerular cell Renin Physiological effects of angiotensin II – Constricts resistance vessels – Acts upon the adrenal cortex to release aldosterone – Stimulates the release of vasopressin – Facilitates norepinephrine release from sympathetic nerve endings – Stimulates thirst centers within the brain Epinephrine & Norepinephrine • Sources Epinephrine---adrenal medulla Norepinephrine---- adrenal medulla sympathetic nerves Catecholamines Norepinephrine Epinephrine Effects Receptor Heart Vessels Epinephrine Norepinephrine a-adrenoceptor ++ +++ b-adrenoceptor ++ + heart rate + cardiac output +++ + (in vitro) - (in vivo) ± constriction (skin, visceral) + +++ - +++ relaxation (SM, liver) total peripheral resistance ± Blood pressure systolic +++ +++ +++ diastolic ± ++ MAP + ++ Clinical application positive inotropic agent pressor agent A 23-year-old woman presents to your emergency service with an anaphylactic reaction after being stung by several bees. She complains of wheezing and shortness of breath. On examination, the client is in acute distress. BP is 98/56 mmHg, PR 110/min, RR 28/min, and temperature 98.7°F. She is immediately treated with supplemental oxygen. In treating this condition further, what drug is required most urgently? A Theophylline B Glucagon C Cimetidine D Methylprednisolone E Epinephrine Vasopressin (antidiuretic hormone, ADH) Endothelium-derived vasoactive substances •Vasodilator factors PGI2--prostacyclin EDRF, NO--endothelium-derived relaxing factor, nitric oxide EDHF--endothelium-dependent hyperpolarizing factor •Vasoconstrictor factors Endothelin Atrial natriuretic peptide (ANP) •Produces natriuresis and diuresis •Decreases renin release •Reduces total peripheral resistance via vasodilatation •Decreases heart rate, cardiac output Autoregulation Definition: Intrinsic ability of an organ to maintain a constant blood flow despite changes in perfusion pressure, independent of any neural or humoral influences The End.