* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiovascular System Chapter 36 “White” Cardiovascular system
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Aortic stenosis wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Artificial heart valve wikipedia , lookup
Rheumatic fever wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
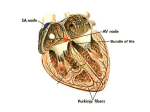
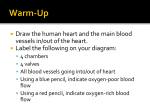
Cardiovascular System Chapter 36 “White” Cardiovascular system consists of the heart and its vascular and peripheral vascular systems. Stroke volume – The volume of blood pumped by the ventricles with each contraction. Function: 1. Provide O2, nutrients, and hormones to the body cells and remove PCO2 and waste products of cellular metabolism from body cells. Blood Circulation: “General Circulation” Inferior or superior vena cava Right Atrium Tricuspid valve Right ventricle Pulmonary artery Lungs Back through pulmonary vein Left atrium Mitral Valve Left ventricle Aorta Conduction System: Pacer (SA Node) AV Node Bundle of His Purkinje Fibers Heart Sounds: Normal S1 = Lub = mitral and tricuspid closure S2 = Dub = closure of the pulmonic and aortic valve Abnormal: S3 = Heard as low pitch sound Sounds like (Lubb-Dubb-by or “Kentucky”) Clients with Congestive Heart Failure Health History Should Include: 1.) Onset of symptoms – what precipitated 2.) Major risk Factors: Age, male gender, diabetes, heredity, and familial history of chest pain or MI These cannot be altered. 3.) Other factors: Cigarette smoking, physical inactivity, contraceptive methods, dyslipidemia, obesity and overweight, and triglyceride levels Assessment: Subjective date: Ask duration, onset, location, does it radiate. 1.) 2.) 3.) 4.) 5.) 6.) 7.) Chest pain Dyspnea (SOB) Edema with or without pitting (fig. 32-6) Fainting = causes decrease in cardiac output and decrease blood flow to the brain Palpatations Diaphoresis Fatigue Orthopnea- pt had difficulty breathing lying down and must sit upright to breath! For peripheral vascular disease: 1.) Pain – Quality of pain should be noted 2.) Parasthesia and/or paralysis in the hands, thigh, calf, ankles, foot, abdomen, or lower back Objective Data: 1.) Skin- cyanosis (peripheral vascular) 2.) Skin turgor- fluid hydration 3.) Respirations - Rate and ease of breathing (ex. CHF) 4.) Heart Sounds – murmers 5.) Radial pulse – if apical pulse is palpated but no radial leads to decreased cardiac output 6.) Ascites – excess fluid in abdomen 7.) Peripheral pulses for blood (pedal pulse) 8.) Weight gain – feet, ankles, or legs -Client can gain 10 lbs. before it is detected -Daily weights: Same time and same scale For peripheral vascular disease assess: 1.) Rate, rhythm and quality of peripheral pulses 2.) If artery is occluded, the foot and leg becomes red when leg is in dependent position and pale when elevated. If vein is occluded, the foot or leg becomes cyanotic when in a dependent position and has normal coloration when elevated. With venous involvement the anterior area of the lower leg and ankle have a brown pigmentation with venous involvement. - Observe ankles for stasis dermatitis = an inflammation of the skin due to decreased circulation - A positive Homan’s sign is present with DVT - HOW TO TEST FOR DVT: Pt dorsiflexes foot and there is pain in calf of leg or behind the knee. May indicate a blood clot. Common Diagnostic Tests for C-V System Disorders: -Table in book (ie ABG’s, Cardiac enzymes (LDH and CPK), chest x-ray, echocardiogram, thalium scan, EKG, Holter moniitor , stress test) NSR: Normal Sinus Rhythm: -SA Node (located in the right atrium) fires and initiates an electrical impulse and spreads through both atria, will yield a “P” wave on the EKG. -Definition of EKG: a graphic recording of the hearts electrical activity. Cardiac-Rhythm/Dysrhythmia -Electrical conduction begins with: SA Node firing and initiates an impulse from SA Node, the electrical impulse spreads thru both atria This yields a P wave on the EKG. (P wave is yielded by contraction of both atria.) - After atrial contraction the electrical impulse reaches the AV node where there is a pause (1/10 sec) allowing blood to enter ventricles. - The electrical impulse starts down the AV Bundle of His which divides into Right and Left Bundle Branches. - The electrical impulses continue from R and L Bundle Branches to the Purkinje Fibers. The Purkinje Fibers transmits impulses to the myocardial cells causing the ventricles to contract! Seen on EKG as “QRS Complex” - QRS= Impulse traveling thru AV Node, Bundle of His, B. Branches, Purkinje Fibers and Ventricles - There is a pause after QRS Complex known as ST Segment. -ST Segment = Represents the period B/W contraction and beginning of recovery or repolarization of ventricular muscles. -T Wave= Represents repolarization of the ventricles. After repolarization of the ventricles the cycle begins all over again! Dysrhythmia’s: -common causes are CAD, MI, electrolyte imbalances, and drug toxicity -Def.-Irregularity in rate, rhythm, or conduction of electrical impulses -Dysrhythmia can be in: A.) Atria B.) Ventriclar or C.) Conduction System -S/S vary from asymptomatic to cardiac arrest Ectopic Beats- irregular beats -Beats that originate somewhere other than SA Node. Bradycardia -heart rate <60 beats/minute -cause of sinus bradycardia are: 1.) myocardial ischemia 2.) electrolyte imbalance 3.) vagal stimulation 4.) heart block 5.) drug toxicity 6.) intracranial tumors 7.) sleep 8.) vomiting Rx: Medication: Atropine and/or permanent pacemaker Tachycardia - Causes a decreased amt of blood to be pumped to the coronary arteries and throughout the body. -There is a limited amt of time for the ventricles to fill with blood. Causes: 1.) exercise 2.)stress 3.)fever 4.)meds 5.)pain 6.)anemia 7.)pericarditis 8.) heart failure 9.)excessive caffeine 10.) tobacco use RX: - Beta Blockers = beta adrenergic cells are located in the heart and stimulation causes increase heart rate. (Beta Blockers will then Decrease Heart Rate) Beta blockers reduce myocardial 02 demands by decreasing BP and decreasing contractility of the heart muscle. (ie Blockers will lower heart rate) Examples: Inderal, Corgard, Timolol - Calcium Channel Blockers = (ie Dilates coronary arteries) - Digitalis: Slow Heart Rate Atrial Dysrhythmias = All occur from disturbances in the electrical conduction in the atria resulting in premature beats or abnormal atrial rhythms. Common causes: MI, CHF, electrolyte imbalance, emotional stress, and drugs They include: PAC, Atrial tachycardia, Paraxysomal supraventricular tachycardia, Atrial flutter, and Atrial fib. 1st. PAC: -An ectopic impulse not originating in the SA node, but originating in artial tissue -S/S: Asymptomatic BUT : If pulse rate increases patient should be evaluated -Cause: Stress, caffeine, and smoking - Can be a symptoms of: Myocardial ischemia, developing CHF, dig toxicity, hypokalemia, or an inflammatory condition. 2nd Atrial Tachycardia: -Known as supraventricular dysrhythmia - An ectopic impulse that causes the atria to contract at a rate of 140 – 250 beats/min - It occurs with 1.) hypokalemia 2.) Dig. Toxicity 3.) Ischemia -Rx: symptomatic: i.e. if hypokalemia Rx. (K) 3rd Paroxysmal Supraventricular Tachycardia (PSVT’s): -Rapid atrial beat accompanied by an abnormal conduction in the AV node. -Cause: Myocarditis, caffeine, alcohol ingestion, smoking and stress - May be present in pts with CAD, mitral valve prolapsed, acute pericarditis 4th Atrial Flutter: -Rapid atrial contraction heart rate 250 – 350 beats/min - EKG displays sawtooth wave pattern - AV Node attempts to block some of the atrial impulses, and ventricles are contracting at a rate of 300 beats/min. -This causes a decrease in the blood supply to the body. - This arrhythmia requires immediate intervention!!!! -Cause: 1.) CAD 2.) PE 3.) Mitral valve disease 4.) Acute MI 5.) Cardiomyopathy -S/S: Pt experiences palpatations 5th Atrial Fibrillation: -Erratic electrical activity of the atria resulting in heart rate 350 – 600 beats/min -The atria quivers rather contracts b/c it is bombarded with impulses -Cause: 1.) CAD 2.) Acute MI 3.) Hypertensive heart disease 4.) Hyperthyroidism -RX: 1.) quinidine 2.) procanaimide Hydrochloride (Procan SR) 3.) Lanoxin – digoxin - Calcium Channel Blockers a.) verapamil (Calan) b.) nifedipine (Procardia) - Beta Blockers a.) atenolol (Tenormin) b.) timolol maleate (Blocadren) - Cardioversion Ventricular Dysrhythmia’s: PVC, V-Tach, V-Fib, Ventricular Asystole 1st PVC’s: -Arise from ectopic beats in the ventricles on EKG -Wide bizarre QRS Complex - No P waves - Cause: myocardial ischemia, electrolyte imbalances, exercise, CHF, dig toxicity, anxiety, hypoxia, caffeine, excessive alcohol ingestion -RX: 1.) Lidocaine 2.) Procan SR 3.) Norpace 4.) Bretylol 5.) Mag sulfate 2nd Ventricular Tachycardia: -Can lead to life threatening dysrhythmia - The occurrence of 3 or more consecutive PVC’s - V-rate +100 beats/min and may go as high as 140 – 240 beats/min. -EKG wide abnormal QRS Complex -Cause: 1.) Cardiomyopathy 2.) Hypoxemia 3. dig toxicity 4. electrolyte imbalance -S/S a.) low BP b.) weak or absent peripheral pulses c.) unconsciousness - Rx: 1.) 02 2.) Procan SR (to slow electrical conduction 3.) Lidocaine hydrochloride 4.) Cardioversion/ defibrillation -Cardioversion- delivery of a synchronized electrical shock to change a dysrhythmia to NSR (Normal Sinus Rhythm) or a rhythm that will improve oxygenation of tissue. (may be elective or emergency) prep is in Book -Defibrillation- delivery of an unsynchronized high energy electrical shock during an emergency situation such as cardiac arrest or pulselessness to a sinus rhythm/NSR -Automatic implantable cardioverter defibrillator (AICD)- used in controlling V-Tach and V. Fib. In individuals with periodic episodes of VTach. -This device senses the dysrrhythmia and automatically sends an electrical shock directly to the heart. The implantation (picture in book) returns it to NSR. 3rd Ventricular Fibrillation: -Serious dysrrhythmia!! Life threatening!! - Disorganized chaotic quivering of the ventricles -A series of jagged, unidentifiable waves on EKG. - Rx: Initiate CPR and defibrillate client 4th Ventricular Asystole: -Straight line on EKG -Ventricles are not contracting -Client loses consciousness with no pulse or respirations - CPR is started and is defibrillated -Rx: 1.) Atropine Sulfate IV 2.) Epinepherine IV Artrioventricular blocks: -When the electrical conduction is interrupted B/W the atria and ventricles at the AV node. -The client is classified as: 1st, 2nd, or 3rd degree blocks 1st degree AV Block: -The impulse is delayed in traveling thru AV node -S/S: NONE -Rx: NONE 2nd Degree AV Block: -Some of the impulses pass thru the AV Node to the ventricles and others are blocked. -S/S: 1.) Vertigo 2.) irregular pulse 3.) weakness -Rx: Temporary Pacer 3rd degree AV Block: -When no impulses are able to pass from the atria thru the AV node to the ventricles. -Cause: Myocardial ischemia, drug toxicity, electrolyte imbalances -Rx: Atropine Sulfate, Permanent Pacer!! Pharmacological Effects: -Arrhythmia originates in atria: Rx: digitalis -Arrhythmia originates in ventricles: Rx: Lidocaine -Diet: Low-Fat, Low cholesterol,l restrict caffeine!! Inflammatory Diseases: 1st Rheumatic Heart Disease: -Complication of rheumatic fever -Rheumatic fever occurs from a post beta-hemolytic strep infection -S/S: 1.) Mild fever, polyarthritis, carditis, chorea and rash 2.) The endocardium, myocardium, and epicardium become inflamed and damage occurs to the mitral valve. Mitral valve becomes thick and stenoised resulting in mitral prolapsed. 3.) Once infected patients are prone to develop it again. 4.) Pts are placed on prophylactic antibiotic therapy prior to dental procedures or invasive surgery. -Antibiotic therapy reduced morality rate!! 2nd Infective Endocarditis: -Infection of the inside lining of the heart in particular the heart valves. - Cause: Bacteria, fungus, rickettsia that invades the valves, they form vegetations that cause scar tissue on valves (esp. mitral valve leading to mitral stenosis.) The valves cannot close properly. -S/S: Fever, heart murmer, enlarged spleen, petechiae on the conjunctivae, buccal mucosa, and distal extremities -2 types: acute and subacute -Diagnostic: 1.) Transesophageal echocardiography 2.) Increased RBC – increase Sed. Rate and WBC 3.) Blood cultures to determine causative organisms -Rx: a.) Valve replacement or repair in severe cases b.) IV antibiotics for 2 – 6 weeks Penicillin, Vancocin, Garamycin c.) Bedrest and decreased workload d.) Antibiotics prophylactically before having dental work – GU or GI invasive procedures 3rd Myocarditis: -Inflammation of the myocardium -Lymphocytes and leukocytes invade the muscle -Fibers of the heart cause chamber to enlarge and muscle to weaken leading to CHF -Cause : Bacteria, virus, fungus, or parasites or autoimmune reaction (rheumatic fever or Lupus) -S/S: 1.) Flulike symptoms (Fever, pharangitis, myalgias, and GI complications) 2.) Chest pain 3.) pericardial friction rub (on auscultation) -Diagnostic: 1.) Elevate Sedimentation 2.) Elevate LDH, SGOT levels 3.) Endomyocardial biopsy -Rx: a.) Digitalis b.)Broad spectrum antibiotics c.) Antiinflammatory agents d.) 02 e.) Bedrest 4th Pericarditis: -Sac surrounding the heart becomes inflamed -Cause: 1.) Viral, bacterial, fungal, or parasite 2.) Could be idiopathic -S/S: 1.) pericardial pain (pain on anterior surface of chest wall), may radiate to neck, back or abdomen. 2.) pericardial friction rub (on auscultation) 3.) pain worsens when client coughs 4.) pericardial effusion (fluid in pericardial space) 5.) Assess for cardiac tamponade (S1 and S2 muffled sound) 6.) Heart movement is limited by scar tissue and cardiac failure may occur -Rx: a.) pericardiocentesis b.) surgical procedure – pericardiectomy or pericardial window c.) antipyretics d.) analgesics e.) anti-inflammatory agents f.) antibiotics g.) digitalis h.) diuretics i.) monitoring with EKG Valvular Heart Diseases: 1. Stenosis and Insufficiency A.) Mitral stenosis – diseased valves become narrowed and thickened -S/S: a.) exertional dyspnea b.) fatigue c.) orthopnea d.) murmur - Diagnostic: 1.) Chest xray 2.) EKG (Atrial fib) 3.) Echocardiogram B.) Mitral insufficiency -Valves become hard and do not close completely Leads to Blood backs up!! -S/S: a.) dyspnea b.)palpatations c.) fatigue d.) atrial fib e.) murmur and gallop -Diagnostic: 1.) Chest xray 2.) EKG (indicates Atrial Fib) 3.) Atrial Fib 2. Aortic Stenosis: -Valve cusps become hard and calcify - S/S: 1.) syncope 2.) dyspnea 3.) arrhythmias 4.) angina 5.) murmur and gallop -Diagnostic: chest xray, EKG (left ventricular hypertopy inverted T-waves) echocardiogram fusion 3. Aortic Insufficiency -Valve cusps don’t close completely -Blood backs up into Left Ventricles -S/S: Palpatations, chest pain, dyspnea, dizziness, fatigue, pulsation of neck veins -Diagnostic: 1.) Chest xray Mitral Valve Prolapse: -Valve leaflets become damaged. -S/S: 1.) palpitations 2.) fatigue 3.) angina 4.) dizziness 5.) syncope -Rx: a.) Prophylactic antibiotics before dental procedures and G.U. and G.I. invasive procedures b.) Surgical procedure – commussurotomy: to separate the valve leaflets Percutaneous Balloon Valvuloplasty: - done in cardiac lab, catheter is placed in the affected valve and balloon is inflated to expand valve. -Often used for elderly or hi-risk surgical clients