* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Valvular Heart Disease
Electrocardiography wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Heart failure wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Infective endocarditis wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Rheumatic fever wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
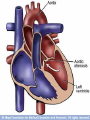
Valvular Heart Disease Dr.Isazadehfar Types • • • • • • Mitral Stenosis Mitral Regurgitation Mitral Valve Prolapse Aortic Stenosis Aortic regurgitation Tricuspid valve is affected infrequently – Tricuspid stenosis – causes Rt HF – Tricuspid regurgitation –causes venous overload Rheumatic Heart Disease • Inflammatory process that may affect the myocardium, pericardium and or endocardium • Usually results in distortion and scarring of the valves Rheumatic Heart Disease, cont. • Subjective symptoms – Prior history of rheumatic fever – General malaise – Pain – may or may not be present • Objective symptoms – – – – Temperature Murmurs Dyspnea polyarthritis Rheumatic Heart Disease • Diagnosis – – – – – – – – – H/P WBC and ESR C-reactive protein Cardiac enzymes EKG Chest x-ray Echo Cardiac cath Cardiac output Rheumatic Heart Disease • Nursing Care – – – – – – Vital signs Rest and quiet environment Give antibiotics, digitalis, and diuretics Provide adequate nutrition Monitor I/O Explain treatment and home care Cardiac Physiology Systole S1-S2 AV/PV – opens MV/TV – closes Diastole S2-S1 AV/PV – closes MV/TV – opens Cardiac Physiology Cardiac Physiology Regurg/ Insuff – leaking (backflow) of blood across a closed valve Stenosis – Obstruction of (forward) flow across an opened valve Systole S1-S2 Diastole S2-S1 AV/PV – opens-------Aortic Stenosis MV/TV – closes------Mitral Regurg AV/PV – closes------Aortic Regurg MV/TV – opens-------Mitral Stenosis These concepts are set in stone, it can’t occur any other way, It would be anatomically impossible Cardiac Anatomy Mitral Stenosis • • • • • • • • Usually results from rheumatic carditis Is a thickening by fibrosis or calcification Can be caused by tumors, calcium and thrombus Valve leaflets fuse and become stiff and the cordae tendineae contract These narrows the opening and prevents normal blood flow from the LA to the LV LA pressure increases, left atrium dilates, PAP increases, and the RV hypertrophies Pulmonary congestion and right sided heart failure occurs Followed by decreased preload and CO decreases Mitral Stenosis, cont. • Mild – asymptomatic • With progression – dyspnea, orthopneas, dry cough, hemoptysis, and pulmonary edema may appear as hypertension and congestion progresses • Right sided heart failure symptoms occur later • S/S – Pulse may be normal to A-Fib – Apical diastolic murmur is heard Etiology of Mitral Stenosis • Rheumatic heart disease: 77-99% of all cases • Infective endocarditis: 3.3% • Mitral annular calcification: 2.7% Mitral Stenosis MS Pathophysiology • Progressive Dyspnea (70%): LA dilation pulmonary congestion (reduced emptying) – • • • worse with exercise, fever, tachycardia, and pregnancy Increased Transmitral Pressures: Leads to left atrial enlargement and atrial fibrillation. Right heart failure symptoms: due to Pulmonary venous HTN Hemoptysis: due to rupture of bronchial vessels due to elevated pulmonary pressure Mitral Stenosis Heart Sounds in MS • Diastolic murmur: – Low-pitched diastolic rumble most prominent at the apex. – Heard best with the patient lying on the left side in held expiration – Intensity of the diastolic murmur does not correlate with the severity of the stenosis Heart Sounds in MS • Loud Opening S1 snap: heard at the apex when leaflets are still mobile – Due to the abrupt halt in leaflet motion in early diastole, after rapid initial rapid opening, due to fusion at the leaflet tips. – A shorter S2 to opening snap interval indicates more severe disease. Management of MS Serial echocardiography: – Mild: 3-5 years – Moderate:1-2 years – Severe: yearly Mitral Regurgitation • Primarily caused by rheumatic heart disease, but may be caused by papillary muscle rupture form congenital, infective endocarditis or ischemic heart disease • Abnormality prevents the valve from closing • Blood flows back into the right atrium during systole • During diastole the regurg output flows into the LV with the normal blood flow and increases the volume into the LV • Progression is slowly – fatigue, chronic weakness, dyspnea, anxiety, palpitations, cough • May have A-fib and changes of LV failure • May develop right sided failure as well Mitral Regurgitation Physical Exam • • • • • Holosystolic Apical Blowing Murmur Laterally displaced apical impulse Split S2 (but is obscured by the murmur) S3 Gallop (increased volume during diastole) Radiation depends on the etiology Mitral Valve Prolapse • Cause is variable and may be associated with congenital defects • More common in women • Valvular leaflets enlarge and prolapse into the LA during systole • Most are asymptomatic • Some may report chest pain, palpitations or exercise intolerance • May have dizziness, syncope and palpitations associated with dysrhythmias • May have audible click and murmur Mitral Regurgitation -MVP Mitral Regurgitation -MVP Mitral Regurgitation -MVP Diagnosis and Treatment • • • • • Echo 2D/Color B-Blockers (hyperadrenergic symptoms, Palpitations) Aspirin (TIAs without etiology) SBE Prophylaxis (only if associated with MR) Severe Symptomatic MR – same as chronic MR Aortic Stenosis • Valve becomes stiff and fibrotic, impeding blood flow with LV contraction • Results in LV hypertrophy, increased O2 demands, and pulmonary congestion • Causes – rheumatic fever, congenital, arthrosclerosis • Atherosclerosis and calcification is primary cause in the elderly • Complications – right sided heart failure, pulmonary edema, and A-fib • S/S – Early: dyspnea, angina, syncope Late: marked fatigue, debilitation, and peripheral cyanosis, crescendodecrescendo murmur is heard Aortic Stenosis Physical Exam • • • • • Harsh Systolic Ejection Murmur – late peaking S4 gallop (from LVH) Sustained Bifid LV impulse (from LVH) Pulsus Parvus et Tardus (Carotid Impulse) Heart sounds- soft and split second heart sound Presentation of Aortic Stenosis - - - Syncope: (exertional) Angina: (increased myocardial oxygen demand; demand/supply mismatch) Dyspnea: on exertion due to heart failure (systolic and diastolic) Sudden death Aortic Stenosis Echo Surveillance • Mild: Every 5 years • Moderate: Every 2 years • Severe: Every 6 months to 1 year Summary • Disease of aging • Look for the signs on physical exam • Echocardiogram to assess severity • Asymptomatic: Medical management and surveillance • Symptomatic: AoV replacement (even in elderly and CHF) Aortic Regurgitation • Aortic valve leaflets do not close properly during diastole • The valve ring that attaches to the leaflets may be dilated, loose, or deformed • The ventricle dilates to accommodate the ↑ blood volume and hypertrophies • Causes: infective endocarditis, congenital, hypertension, Marfan’s • May remain asymptomatic for years • Develop dyspnea, orthopnea, palpitations, ,and angina • May have ↑ systolic pressure with bounding pulse • Have a high pitch, blowing, decrescendo diastolic murmur Etiology of Acute AR • Endocarditis • Aortic Dissection • Physical Findings: – Wide pulse pressure – Diastolic murmur – Florid pulmonary edema Aortic Regurg – pathophysiology Aortic Regurgitation • Progressive Symptoms include: - Dyspnea: exertional, orthopnea, and paroxsymal nocturnal dyspnea - Nocturnal angina: due to slowing of heart rate and reduction of diastolic blood pressure - Palpitations: due to increased force of contraction Aortic Regurgitation Physical Exam • Diastolic Decrescendo Blowing Murmur at the left sternal border • Hyperdynamic LV apical impulse • Bounding Pulses • S4, S3 Gallop-advanced AI • Apical Rumble – “Austin Flint Murmur” (apex): Regurgitant jet impinges on anterior MVL causing it to vibrate • Systolic ejection murmur: due to increased flow across the aortic valve • Assessment for Valve Dysfunction • Subjective symptoms – – – – – – – – Fatigue Weakness General malaise Dyspnea on exertion Dizziness Chest pain or discomfort Weight gain Prior history of rheumatic heart disease Assessment, cont. • Objective symptoms – – – – – – – – – Orthopnea Dyspnea, rales Pink-tinged sputum Murmurs Palpitations Cyanosis, capillary refill Edema Dysrhythmias Restlessness Diagnosis • History and physical findings • EKG • Chest x-ray • Cardiac cath • Echocardiogram Medical Treatment • Nonsurgical management focuses on drug therapy and rest • Diuretic, beta blockers, digoxin, O2, vasodilators, prophylactic antibiotic therapy • Manage A-fib, if develops, with conversion if possible, and use of anticoagulation Interventions • Assess vitals, heart sounds, adventitious breath sounds • O2 as prescribed • Emotional support • Give medications • I/O • Weight • Check for edema • Explain disease process, provide for home care with O2, medications Surgical Management of Valve Disease • Mitral Valve – Commissurotomy – Mitral Valve Replacement – Balloon Valvuloplasty • Aortic Valve Replacement Mechanical Valve Mechanical Valve Porcine Valve Tissue Valve Tissue Valve Common Murmurs and Timing (click on murmur to play) Systolic Murmurs • Aortic stenosis • Mitral insufficiency • Mitral valve prolapse • Tricuspid insufficiency Diastolic Murmurs • Aortic insufficiency • Mitral stenosis S1 S2 S1