* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download heart - WordPress.com
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
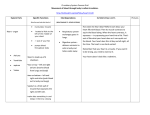
HUMAN ANATOMY LECTURE SIXTEEN CARDIOVASCULAR SYSTEM CARDIOVASCULAR SYSTEM Includes: • heart • blood vessels • fluid connective tissue component BLOOD FUNCTION - maintain homeostasis by: • • • • • • Transportation of gases, nutrients, and waste products Transport of regulatory molecules (hormones) Regulation of pH and ion concentration of interstitial fluids Maintenance of body temperature Protection against foreign substances (toxins and pathogens) Clot formation CHARACTERISTICS • Fluid connective tissue consisting of cells (formed elements) and cell fragments (formed elements) surrounded by a liquid matrix (plasma) • Temperature ~38 °C • pH 7.35 - 7.45 PLASMA • • 91% water, 7% proteins (albumin, globulins, fibrinogen), 2% other High capacity for holding heat - distributes heat generated from metabolic activity of tissues Albumin • • Most abundant (60%) of plasma proteins Important in transport of materials in the blood - A.A. and some hormones Globulins • Function as antibodies and for transport of some ions and hormones Fibrinogen • Responsible for formation of blood clots FORMED ELEMENTS • Erythrocytes (RBC), leukocytes (WBC), thrombocytes (platelets) • Produced by a process called HEMATOPOIESIS - in adults occurs in red bone marrow • Derive from STEM CELLS that differentiate into specific cell types ERYTHROCYTES - RED BLOOD CELLS • Biconcave disc with thin central region and thicker edges - increases surface area for movement of gases in and out of cell - ability to form stacks within tiny blood vessels - flexibility to bend or stretch • Lack organelles (to make room for more gases) - not able to divide so are replaced every ~120 days • HEMOGLOBIN is the main component - composed of 4 globins (large protein molecules) and a heme (pigment molecule that holds iron) - heme with oxygen = oxyhemoglobin (bright red) - heme without oxygen = deoxyhemoglobin (dark red) - heme with carbon dioxide = carbaminohemoglobin BLOOD TYPING • Antigens (proteins) appear on the surface of RBC’s TYPE A blood has A ANTIGENS TYPE B blood has B ANTIGENS TYPE AB blood has AB ANTIGENS TYPE O blood has NO ANTIGENS • Antibodies in the plasma attack antigens TYPE A blood has B ANTIBODIES TYPE B blood has A ANTIBODIES TYPE AB blood has NO ANTIBODIES TYPE O blood has A and B ANTIBODIES • Donors give blood and recipients receive blood LEUKOCYTES - WHITE BLOOD CELLS • • • • • • Spherical cells that lack white hemoglobin (clear/white) Much larger than RBC’s, have nucleus and other organelles Primary functions are: - to protect the body against invading microorganisms - to remove dead cells and debris from the tissues by phagocytosis Move out of the blood and through the tissues by ameboid movement cytoplasmic streaming into projections of the cellular membrane Migrate through body tissues to areas of infection or injury - able to chemically detect signs of tissue damage Many are capable of phagocytosis (engulfing) of pathogens, cell debris, etc. TYPES OF LEUKOCYTES • Named for appearance when stained - large cytoplasmic granules = GRANULOCYTES - very small granules = AGRANULOCYTES GRANULOCYTES (1) Neutrophils – most common • • • Have a very dense segmented nucleus with 2 – 5 lobes attached by a string-like structure - polymorphonuclear leukocytes Highly mobile, first to the site of an injury Phagocytize foreign substances, attack bacteria “marked” by antibodies (2) Basophils – least common • • Have many granules that stain very dark Migrate to injury site and discharge granules into interstitial fluid - histamine dilates blood vessels and heparin to prevent blood clotting (3) Eosinophils • • Granules stain red Attack objects coated with antibodies and release chemicals that reduce inflammation AGRANULOCYTES (1) Lymphocytes – smallest WBC • • • Large, round nucleus surrounded by a thin layer of cytoplasm Continuously migrate through bloodstream, through tissues, and back into the bloodstream Production of antibodies and other chemicals that destroy microorganisms, produce allergic reactions, control tumors, and regulate immune system (2) Monocytes – largest WBC • • • Large spherical cells Leave bloodstream and become macrophages - phagocytize bacteria, dead cells, and other cellular debris within tissues Release chemicals that attract other WBC’s THROMBOCYTES - PLATELETS • Fragments of cells - bits of cytoplasm surrounded by cell membrane • Produced in bone marrow by megakaryocytes (very large cells) • Prevent blood loss by: (1) formation of platelet plugs to seal holes in small vessels (2) formation of clots to seal larger wounds in vessels - platelet plug forms to close site temporarily - chemicals released causing vasoconstriction, bring more platelets to the injury site, promoting vessel repair - plasma proteins form permanent clot HEART • Located in the thoracic cavity between the lungs, within the mediastium • The apex (pointed tip) is the most inferior region - directed anteriorly and to the left, deep to the 5th intercostal space (between the ribs) • The base (flat top) is directed superiorly and slightly posteriorly deep to the 2nd intercostal space • Functions: - generating blood pressure - routing blood through the systemic (body) and pulmonary (lungs) circuits - ensuring one-way blood flow EXTERNAL ANATOMY Pericardium - double-layered closed sac anchoring the heart and vessels within the mediastium • Consists of: - fibrous pericardium = outer layer with dense network of collagen fibers - serous pericardium = thin layer of connective tissue • Serous pericardium is divided into: - visceral pericardium or epicardium covering the outer surface of the heart - parietal pericardium lining the fibrous pericaridium Pericardial cavity (space) between the visceral and parietal pericardium - full of pericardial fluid produced by serous pericardium – reduces friction as the heart moves within the pericardium PERICARDIUM Auricles extend from each atria - expandable extension of atria Coronary sulcus - deep groove separating atria and ventricles - anterior and posterior interventricular sulci mark the separation between the left and right ventricles (fat builds up in these depressions) HEART WALL Three layers of tissue: Epicardium (visceral pericardium) • thin, serous membrane forming the outer layer • simple squamous epithelium over a layer of loose connective tissue and fat Myocardium • Middle layer of cardiac muscle, blood vessels, nerves • Concentric layers of cardiac muscle tissue • The atrial myocardium contains muscle bundles that wrap around the atria and from figure eights encircling the large vessels • Superficial muscles wrap around the ventricles with deeper layers spiraling around and between the ventricles Endocardium • Smooth inner surface of heart chambers • Simple squamous epithelium continuous with lining of the large vessels • Form the heart valves by folding with connective tissue between the layers MUSCLE LAYERS INTERNAL ANATOMY • Divided into four chambers: right and left atrium - right and left ventricles • Interatrial septum separates the atria and thicker interventricular septum separates the ventricles ATRIA • Smaller, thinner walled upper chambers - receive blood right atrium - superior and inferior vena cava bring blood from upper and lower body - small coronary sinus enters from the wall of the heart left atrium - pulmonary veins (4) bring blood from the lungs VENTRICLES • Major pumping chambers - push blood to heart and body right ventricle - pulmonary trunk to pulmonary arteries to lungs left ventricle – aorta carries blood to body • Left ventricle wall is thicker than the right – pumps blood further • Walls have muscular ridges called trabeculae carneae INTERNAL STRUCTURE HEART VALVES One-way valves prevent the backflow of blood as chambers contract Fibrous connective tissue rings (skeleton of the heart) around the valves provide solid support for the valves ATRIOVENTRICULAR VALVES • Located between the atrium and ventricles right AV valve - tricuspid valve with 3 cusps (folds) left AV valve – bicuspid (mitral) valve with 2 cusps • After blood flows from atria to ventricles the valves are pushed backward toward atria forcing the opening shut • Papillary muscles attach to valves by thin, strong connective tissue strings called chordae tendinae - muscles contraction prevents valves from opening SEMILUNAR VALVES • Found in aorta and pulmonary trunk • Consists of three pocketlike semilunar cusps • When ventricles contract blood pushes valves open - during relaxation blood flows back toward the ventricle, entering pockets of cusps causing them to bulge inward and meet in the center, thus blocking the vessel VALVES BLOOD SUPPLY TO THE HEART • • • • • • Myocardium is thick and very active metabolically Coronary arteries supply blood to the heart wall Two c. arteries originate from base of the aorta, just above the semilunar valve - the left c. artery supplies the left side and the right c.artery supplies the right side - both lie within the coronary sulcus Cardiac veins drain blood from the myocardium The great cardiac vein runs along the interventricular sulcus - running parallel to the c.arteries and carries blood to the coronary sinus (a large vein within the coronary sulcus on posterior side of heart) The coronary sinus drains into the right atrium HEARTBEAT • Contraction of the atria and ventricles is coordinated by specialized cardiac muscle cells (nodes) in the heart wall that form the conduction system of the heart SINOARTERIAL NODE • The impulse originates in the SA node which contain pacemaker cells that establish heartbeat • Embedded in the posterior wall of the right atrium near the entrance of the superior vena cava • Send electrical impulses across the atria causing them to contract • Connected to the AV node by internodal pathways in the atrial walls ATRIAVENTRICULAR NODE • Found within the floor of the right atrium near the opening of the coronary sinus • Impulse is conducted into a bundle of fibers - the atrioventricular bundle or bundle of His down the septum and divide into left and right bundle branches • At the tips of the bundle branches the conducting tissue forms many small bundles of Purkinje fibers - extend to the apex of the heart and to the cardiac muscle of the ventricle walls - conduct action potentials very quickly SA node atria contract AV node bundle of His Purkinje fibers ventricles contract while atria relax entire heart relaxes ELECTROCARDIOGRAM • Electrodes are placed on the surface of the body to measure electrical current of the heartbeat • P wave - contraction of the atria • QRS complex - contraction of the ventricles • T wave - relaxation of atria BLOOD VESSELS Walls of blood vessels (arteries and veins) are made up of three layers: (1) Tunica intima - inner endothelial lining with connective tissue layer - arteries have thick layer of elastic fibers (2) Tunica media - concentric rings of smooth muscle bound to other layers by collagen fibers - in arteries separated from tunica externa by a layer of elastic fibers - larger arteries have very thick layer (3) Tunica externa - outermost layer, a connective tissue sheath for anchoring - in arteries collagen fibers with elastin ARTERIES Carry blood away from the heart Have thick, muscular, elastic walls that allow changes in diameter in response to changes in blood pressure - allow artery to expand and contract ELASTIC ARTERIES • Largest in diameter with thickest walls • Greater portion of elastic tissue as compared to smooth muscle compared to smaller arteries MUSCULAR or DISTRIBUTING ARTERIES • Medium-sized arteries distribute blood to skeletal muscles and organs • Walls are thick as compared to their diameter - thick tunica media layer • Blood flow is controlled by vasoconstriction and vasodilation ARTERIOLES • Tunica media is only one or two layers of smooth muscle in larger arterioles, small arterioles only have smooth muscle scattered throughout • Innervated by sympathetic nerve fibers - vasoconstriction CAPILLARIES • Very thin walls allow exchange between blood and surrounding fluids • Diameter so narrow that red blood cells flow through in single file • Origin of each branch has precapillary sphincters of smooth muscle that regulate blood flow • At arteriole end oxygen and nutrients leave and at venous end carbon dioxide and waste products enter VEINS Collect blood from tissues and organs and returns it to the heart Walls are thinner than arteries because blood pressure is much lower VENULES • Take blood from capillaries • Lack tunica media layer MEDIUM-SIZED VEINS • Tunica media layer is thin with little smooth muscle • Thickest layer is tunica externa • Tunica intima folds inward forming one-way valves to prevent backflow of blood - more in veins of lower limbs LARGE VEINS • Have all tunica layers with thin media and thicker externa layers ARTERIES vs VEINS • Artery walls are thicker - more muscle and elastic fibers in the tunica media • Lumen of the artery often looks smaller than that of a vein because it recoils when not being stretched - looks pleated • Arteries retain cylindrical shape - veins often collapse • Arteries are more resilient - keep their shaped stretched • Arteries don’t have valves CARDIOVASCULAR SYSTEM SYSTEMIC SYSTEM - heart to body to heart left ventricle aorta arteries of tissue or organ capillaries veins right atrium vena cava PULMONARY SYSTEM - heart to lungs to heart right ventricle pulmonary trunk pulmonary arteries lungs left atrium pulmonary veins